A glomus tumor is a benign vascular tumor derived from neuromyoarterial structures. Up to 80% of these lesions are located in the arms, with subungual sites being particularly frequent.1 These subungual tumors are characterized clinically by intense spontaneous pain or pain on trauma and cold intolerance. Treatment of these lesions is a challenge given the difficulty in preoperative localization of the tumor2 and complications associated with surgery such as recurrence and nail dystrophy.3
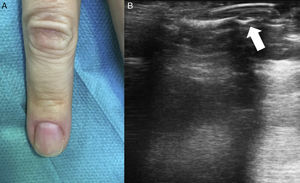
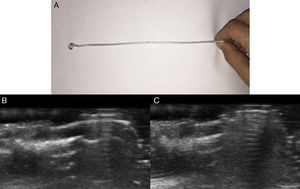
Description of the TechniqueA 43-year-old woman, who had previously undergone prior surgery for a subungual glomus tumor on the fourth finger of the right hand with the same technique described below, but without preoperative ultrasound, attended the clinic with intense paroxysmal pain. The clinical examination was normal, with no evidence of recurrence of the subungual glomus tumor (Fig. 1A). A skin ultrasound with an 18MHz transducer was performed and tumor recurrence was detected in the nail bed. The tumor measured 3.1mm in diameter (Fig. 1B). Prior to surgery, the tumor was localized by ultrasound and the nail plate was marked using a homemade guide (Fig. 2A). For this, the ultrasound transducer was oriented longitudinally with respect to the nail apparatus and the ultrasound guide was introduced perpendicular to the transducer to generate a comet tail reverberation that would hide the tumor (Fig. 2B). At this point, we kept the ultrasound guide fixed, withdrew the transducer, and marked the nail plate (Fig. 2C).
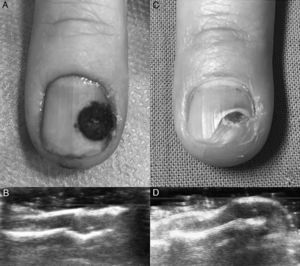
Subsequently, after peripheral nerve block anesthesia of the finger with mepivacaine 2%, minimally invasive surgery was performed with removal of the nail plate using a 5mm punch, tumor excision with 4mm punch, dissection with a no. 15 scalpel, electrocoagulation of the nail bed, and induction of hemostasis with Gelita and Monsel solution (ferric subsulfate 20%). Histological study confirmed diagnosis of glomus tumor recurrence. The outcome of surgery was favorable. Pain resolved after the procedure and no evidence of tumor persistence was detected by ultrasound (Fig. 3A-D).
Indications and Contraindications for the TechniqueThe technique is suitable for treating subungual glomus tumors of difficult clinical preoperative localization or recurrent tumors. The procedure should be used preferably for small tumors (<3mm) with a distal subungual location, thus avoiding the classic transungual approach with a high risk of oncydystrophy.4 This approach is simple and less traumatic. A drawback of the technique to highlight is that the lesion cannot be well visualized during surgery compared with a transungual approach. With this technique, use of preoperative ultrasound and marking the exact site of the tumor on the nail plate with a guide avoided having to perform the surgery blind.
ComplicationsThe technique we present is very safe and complications are infrequent. Although operative bleeding is limited, it may be appropriate to apply a tourniquet prior to the procedure to enable directed bloodless surgery for complete excision of the lesion.
ConclusionThis ultrasound-guided approach is useful for the treatment of recurrent subungual lesions or those that are hard to localize prior to excision.
Surgical excision using a tourniquet, partially extracting the plate with prior orientation of the affected quadrant by an imaging test and an ultrasound-guided procedure as described avoid full excision of the nail plate and damage to the matrix. The patient described had a favorable postoperative outcome for both techniques, with a low risk of complications.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Domínguez-Cruz J, Ortiz-Prieto A, Martín-Carrasco P, Conejo-Mir J. Extirpación eco-guiada mínimamente invasiva del tumor glómico digital. Actas Dermosifiliogr. 2018;109:271–273.