Dermatologic surgery has 2 main objectives: 1) to guarantee surgical radicality; and 2) to achieve optimal aesthetic and functional results. These 2 paradigms and their hierarchy must be considered when performing surgical procedures on the skin. Even the easiest intervention, the elliptical excision, presents some features that should be known to achieve such goals. One of these features is the incision orientation.
The optimal incisions orientation is still matter of debate, especially because studies that compare the outcomes of performing incisions in different directions are lacking. However, some anatomical, clinical, and histological observations may point out why incising the skin in one orientation is better than another.
Knowing the theory behind skin incisions/excisions become of outmost importance when dealing with primary cutaneous melanoma surgery. Especially if the melanocytic lesion is suspected to be an invasive melanoma and a sentinel lymph node biopsy will be required.
La cirugía dermatológica tiene 2 objetivos principales: 1) asegurar la radicalidad quirúrgica, y 2) obtener unos resultados estéticos y funcionales óptimos. Se tienen que considerar estos 2 paradigmas y su jerarquía cuando se realizan intervenciones quirúrgicas en la piel. Incluso la intervención más sencilla, el huso, presenta algunas características que deberían ser conocidas para obtener dichos objetivos. Una de estas características es la orientación de la incisión.
La orientación óptima de las incisiones es todavía materia de debate, especialmente porque no hay estudios que comparen los resultados según la dirección de la incisión. Sin embargo, algunas observaciones anatómicas, clínicas e histológicas podrían indicar por qué cortar la piel con una orientación es mejor que otra.
Conocer la teoría detrás de las incisiones/extirpaciones cutáneas se vuelve imprescindible cuando hay que enfrentarse a la cirugía del melanoma cutáneo primario. Especialmente si se sospecha que la lesión melanocítica es un melanoma invasivo y se requerirá una biopsia del ganglio centinela.
Cutaneous tumors have generally a radial growth and, thus, produce circular defects when removed. However, if a circular defect is closed directly, two cones of exceeding tissue appear at the apexes of the linear closure. Excising these standing cones permits to achieve optimal aesthetic results, but it is not required to remove completely the tumor. If the removal of these standing cones is anticipated during the excision of the tumor, an elliptical shape is formed.
DiscussionDermatologic surgery has two objectives: 1) to guarantee surgical radicality, namely, the complete removal of the tumor; and 2) to achieve optimal aesthetic and functional outcomes.1–3 Both these objectives need to be considered every time a surgical procedure on the skin is planned.
Usually, a cutaneous tumor is removed by incising the skin following an elliptical shape. This shape is so common and useful that it is performed almost automatically. However, it could be helpful to consider elliptical excisions as formed by two parts: 1) a circular center, including the clinically visible tumor and a surgical margin of surrounding unaffected skin; and 2) two 30̊ tip triangles at the circular center periphery, one specular and diametrically opposed to the other. The circular shape of the center is because cutaneous tumors have usually a radial growth and, thus, they tend to appear as roundish lesions. On the other hand, the two triangles are excised to remove the exceeding conical tissue (“dog's ear”) that appears when the circular defect is closed directly. These triangles are known as Burow's triangles when used to allow skin flaps movement during more complex reconstructive procedures.4 It is important to understand that the removal of the circular center is performed to excise completely the tumor (first objective), whereas the removal of the Burow's triangles aims to achieve an optimal cosmetic result (second objective). Therefore, they are not required if the main objective is to obtain surgical radicality. This is evident when performing an incisional or excisional biopsy using a punch; the circular defect is closed without removing more tissue (i.e., the Burow's triangles). Exaggerating, the elliptical excision could be considered as the simplest type of advancement flap.
Surgical defects can also be left to heal by second intention healing and, thus, there is no exceeding tissue to be removed. Nevertheless, it is generally optimal to close surgical defects directly (if local tissue permits direct closure). This direct closure can be virtually realized with any orientation, both for elliptical and circular defect. In case of elliptical defects, a Burow's triangle is anticipated at each end of the linear closure, and it is instantly removed. In case of circular defects, a standing cone will appear at each apex of the closure, and it may be subsequently removed or not. Remarkably, some authors advocated this last surgical approach because it leads to shorter scars.5,6 However, subsequently removing the standing cones may be less precise because of the local tissue modification due to surgery (e.g., edema) or because of different positioning of the body during the procedure. As per the direction of the closure, even the removal of standing cones can be virtually made with any orientation or shape.7 Other techniques to correct exceeding tissue are suturing using the rule of halves7 or removing a semilunar slice of skin instead of a triangle (crescentic technique).8
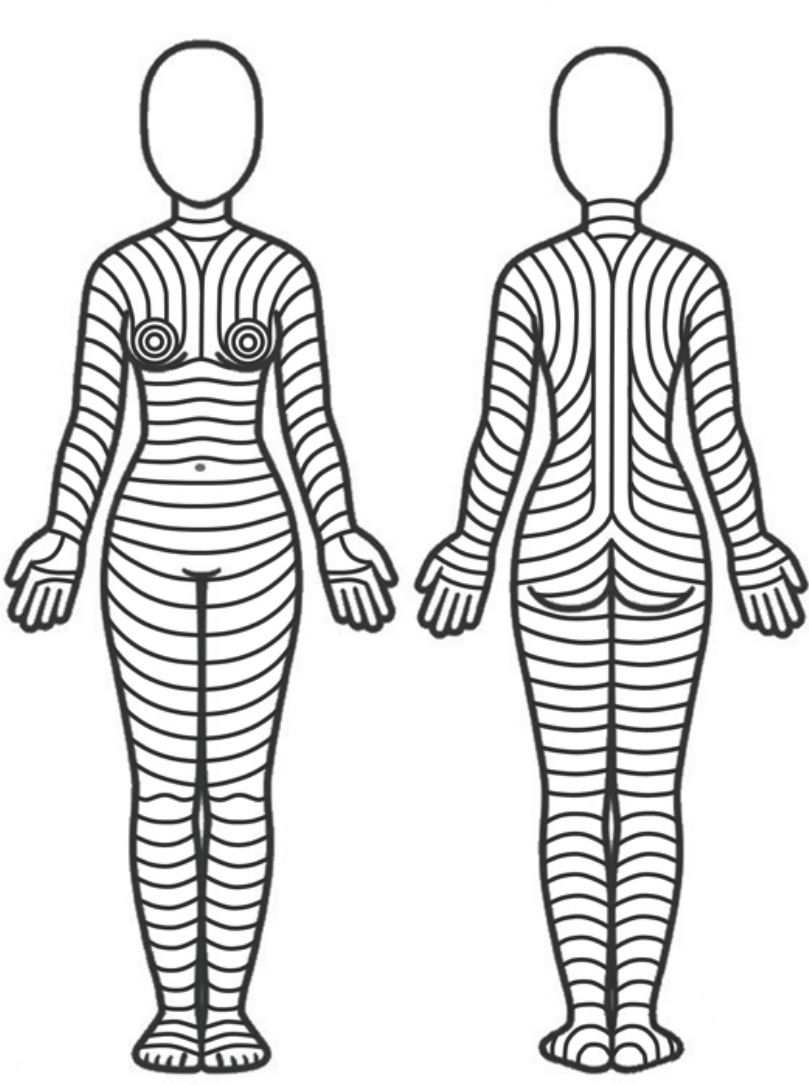
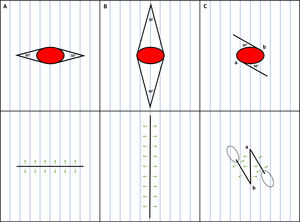
Is there an optimal orientation for skin incisions/excisions?The optimal orientation of skin incisions/excisions is still matter of debate, especially because studies that compare the outcomes of performing incisions in different directions are lacking. However, some anatomical, clinical, and histological observations suggest that skin incisions/excisions should follow the skin main folding lines (MFLs) (Fig. 1). Essentially, these lines lie parallel to the wrinkles in elderly patients and perpendicular to striae distensae in young patients. It is important to evaluate or evocate these lines with the patient standing in anatomical position, because body posture can modify their pattern.
Theoretical pattern of skin main folding lines based on the observations by Lemperle et al.10
Dermatologic surgery is a field where oral tradition flourishes. Many surgical concepts are passed by tutors to pupils without being questioned and, unfortunately, not all this wisdom corresponds to the truth. One of these dictums is to orientate skin incisions/excisions following a pattern of virtual lines, usually referred as Langer's lines9 (Fig. 2A). However, the lines described by Langer were never meant to guide surgeons’ skin incisions.10,11 Moreover, the term “Langer's lines” is often associated to drawings and description of incision lines made by other authors.12 In fact, many patterns of skin incision lines were described during history.10,11 Among the best known and the most used in dermatologic surgery, there are Kraissl's anti-tension lines13,14 and Borges’ relaxed skin tension lines.15–17 It is interesting to point out that, while Kraissl produced drawings of his lines for the whole body (Fig. 2B), Borges did only for the face and palms.
Langer's lines (A) (reprinted from On the anatomy and physiology of the skin. I. The cleavability of the cutis. (translated from Langer, K. (1861). Zur anatomie und physiologie der haut. I. Uber die spaltbarkeit der cutis. Sitzungsbericht der mathematisch-naturwissenschaftlichen classe der kaiserlichen academie der wissenschaften, 44, 19). Br J Plast Surg. 1978;31 1:3–8), Kraissl's anti-tension lines (B) (reprinted from Kraissl CJ. The selection of appropriate lines for elective surgical incisions. Plast Reconstr Surg (1946). 1951;8 1:1–28), Pinkus’ main folding lines (C) (reprinted from Pinkus F. Die faltung der haut. en: Pinkus F, editor. Die normale anatomie der haut jadassohn's handbuch der haut und geschlechtskrankheiten. Berlin: Springer; 1927, p. 4–76), and Paul's biodynamic excisional skin tension lines (D) (reprinted from Paul SP. Biodynamic excisional skin tension lines for surgical excisions: Untangling the science. Ann R Coll Surg Engl. 2018;100 4:330–7).
These patterns of skin incision lines were described in studies based on statical anatomical, clinical and histological observations.11 Therefore, they lacked biomechanical and biodynamical data that may demonstrate why incising the skin in one direction is better than another. Recently, Paul explored this field, following previous observations and hypotheses, and described the biodynamic excisional skin tension lines18 (Fig. 2D). Interestingly, these lines completely contradict the previous patterns described, except on some areas of the face.11,18 These results are exceptionally counterintuitive in anatomical locations such as the neck, where common surgical experience advises to perform incisions horizontally (e.g., thyroidectomy incisions) with excellent aesthetic results (Fig. 3). Is it possible that the measured tension is deceiving? As pointed out by other authors, the aesthetic outcomes of performing skin incisions along biodynamic excisional skin tension lines should be analyzed.19
In the end, there are not prospective studies that compare the results of performing incisions in different orientations. Consequently, it is advisable to still rely on clinical observations and experts’ wisdom.
On the face it is commonly accepted to orientate scars following the pattern of wrinkles.10,11 This is more difficult on the body, where wrinkles are less visible and predictable, even in elderly patients. If not clinically evident, wrinkles can be elicited by muscular movement (Kraissl's anti-tension lines) or by pinching the relaxed skin (Borges’ relaxed skin tensions lines). Nevertheless, these two techniques present variabilities that may alter their results. For example, pinching can be altered by the direction of applied force and both techniques may perform differently depending on the positioning of the body (prone vs supine, lying vs standing, etc.).10
Recently, Lemperle et al. proposed an interesting clinical observation that may point out which lines are to follow in orientating skin incisions on the body.10 They defined these lines as skin MFLs, recovering the term used by Pinkus in 192720 (Fig. 2C). In authors opinion, this definition is easier to understand and better describes the visual appearance of such lines. In their study, Lemperle et al. analyzed patterns of striae distensae and concluded that the orientation of striae lies perpendicular to the orientation of MFLs.10 This could justify why incisions performed parallelly to MFLs achieve better outcomes, because they are not subject to the same changes that promote striae formation. The “primus movens” of striae distensae formation is the destruction of collagen bundles by hormonal factors.10 Instead, in ill-oriented surgical scars (i.e., perpendicularly to MFLs) the collagen bundles are destroyed by the surgeon's scalpel. In both cases, fibroblasts are stimulated to produce newly synthetized collagen fibers and repair the damage. Eventually, reorganization of collagen bundles along the main tension orientation (theoretically, perpendicular to MFLs) and a higher mechanical stimulus on fibroblasts cause the formation of clinically evident striae and suboptimal scars (i.e., hypo or hypertrophic). On the contrary, when the incision is oriented correctly (i.e., parallelly to MFLs), the collagen bundles are more separated than destroyed, there is less damage to repair and, thus, less scar tissue is formed.21 Also, the scar tension is lower because the incision lies parallel to the main tension direction. This leads to less fibroblasts’ stimulation and collagen reorganization.
Beyond clinical observation, this theory could have histological bases. The body surface is furrowed by a lattice pattern of virtual lines created by the connections between the skin, the fascial system, and the underlying musculoskeletal apparatus.22 These interactions may determine the orientation of collagen bundles and elastic fibers in the dermis. The MFLs, as the name suggests, are the principal and most evident of these lines. Lemperle observed that collagen bundles in the dermis run mainly parallel to the MFLs, while the elastic fibers anchoring the collagen fibers run perpendicular to them.21 A similar histological structure has been observed on human body creases, although their architecture is more complex, with a beehive pattern of collagen bundles in the subcutaneous tissue that anchor the skin to the underlying fascia.22 These structural differences could explain why creases are visible and fixed lines, whereas MFLs are mostly invisible and change with body posture (Fig. 4). Remarkably, skin folds around a crease, just as around an MFL. Analogous findings were previously reported by Kraissl, who observed perpendicular strands of connective tissue attaching the skin to the underlying tissues in correspondence of wrinkles and creases.14 In fact, some of the MFLs become clinically evident with cutaneous physiological aging, due to the loss of skin elasticity and changes in the volumes of underlying fat compartments (i.e., wrinkles). Moreover, they may appear during muscles’ contraction or pinching of the skin, as stated above.
According to these considerations, surgical defect should be closed following the MFLs. This should also be true when planning a closure with a local skin flap: the flap aspect subject to higher tension should be oriented parallelly to an MFL.14
Therefore, it is useful to know the theoretical pattern of skin MFLs and to observe or elicit them with the patient in anatomical position (Fig. 1). This pattern must be used as a guide, not as a rule. Other factors (e.g., type of tumor, patient characteristics, patient preferences, etc.) need to be considered when planning skin incisions or reconstructions, and unexpected events (e.g., infections, technical errors, etc.) might influence the surgical outcomes.
Moreover, incising the skin following the MFLs is sometimes not feasible or optimal. For example, when a skin tumor shape is not roundish, but elliptical and oriented against the direction of the MFLs, it is debatable if it is better to perform a larger elliptical excision oriented along the MFLs or a shorter excision against them. Probably, in some of these cases, an anticipated Z-plasty (or other scar revision techniques) can be optimal to put the scar tension in a more favorable direction without removing too much healthy tissue (Fig. 5). The same objective is sought when modifying common skin flaps.8,23
Options to close an elliptical surgical defect (red ellipse) with its main axis oriented against the skin main folding lines (MFLs). A) Shorter ellipse perpendicular to the MFLs. B) Longer ellipse parallel to the MFLs. C) Anticipated 30̊ Z-plasty. Blue lines depict the MFLs; green arrows depict the vectors of tension; dotted ellipses depict the eventual standing cones due to Z-plasty.
Furthermore, if the defect is near a body crease, it is optimal to orientate the surgical defect to lie in the crease even if its orientation is not parallel to the skin MFLs. This is commonly performed when the defect is located at the border between two facial cosmetic units, which are usually divided by creases. It is common experience that scars hidden inside creases result in excellent aesthetic outcomes.7 Probably, this is due to their histological structure, as discussed previously.22 Finally, it is mandatory that the closure tension does not alter lips, eyelids, or eyebrows by pulling them.7
When is not an elliptical excision the best solution?An elliptical excision is not the best solution when dealing with primary cutaneous melanoma surgery. In fact, not performing an elliptical excision in case of lesions highly suspicious to be melanomas has three advantages: 1) not risking altering the lymphatic drainage, 2) orienting the closure in the best direction, 3) removing less healthy tissue in a subsequent wide local excision. This is especially true if the melanocytic lesion is suspected to be an invasive melanoma and a sentinel lymph node biopsy will be required.
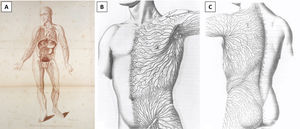
DiscussionThe two previous considerations become especially handy for the excisional biopsy of lesions suspicious to be primary cutaneous melanomas. These lesions should be excised completely with a narrow lateral margin of surrounding unaffected skin (1–3mm) and a deep margin into the upper subcutis. In case of elliptical excision, the longest axis of the ellipse should be oriented parallelly to the lymphatic vessels to avoid cutting into more lymphatics and, theoretically, impair an eventual sentinel lymph node biopsy.24,25 However, orienting the elliptical incision parallelly to the lymphatic vessels may result in a suboptimal aesthetic and functional outcome, because in some area of the body the course of lymphatic drainage is not parallel to the MFLs. Indeed, it can be even perpendicular to them. This is especially true for the limbs, where the lymphatic drainage flows parallelly to the limb main axis, while the MFLs are horizontal or slightly oblique. On the other hand, in the head, neck and trunk regions the lymphatic drainage is more unpredictable and, thus, may differ from the anatomical pattern classically described (Fig. 6).26 In these cases, or in case of doubt, it is practical to perform a simple circular excision of the suspicious lesion without removing the two Burow's triangles needed to shape the ellipse. This permits one to close the defect with any orientation, even perpendicularly to the lymphatic flow, without cutting into more lymphatic vessels. Clearly, the optimal orientation should be parallel to the MFLs (Fig. 7). Potential tissue cones, if persistent, could be removed with the wide local excision, if the lesion is confirmed to be a melanoma, or in a subsequent intervention, if the lesion is diagnosed as benign. However, standing cones may improve and even disappear spontaneously during scar healing process, especially for small size defect, thus many patients may not require further scar revision. The importance of orienting the primary defect parallelly to the MFLs become more evident during the wide local excision. In this procedure, a margin of 0.5–2cm is excised at both sides of the scar, or along the perimeter of the previous defect if secondary intention healing was chosen. Therefore, the surgical defect is usually of wide dimensions and, if oriented improperly, the tension on the scar will be massive, resulting in suboptimal cosmetic and functional outcomes. Moreover, the elliptical excision removes two triangles of healthy tissue that are difficult to consider when measuring the distance from the scar during wide local excision planning. This entails that more healthy tissue may be unnecessarily removed.
Lymphatics of the human body by William Cruikshank (A) (reprinted from Cruikshank WC: The Anatomy of the Absorbing Vessels of the Human Body. London, G Nicol, 1786), and Sappey's drawings of the lymphatic drainage of anterior (B) and posterior trunk (C) (reprinted from Sappey MPC: Anatomie, Physiologie, Pathologie des Vaisseaux Lymphatiques Consideres chez I’Homme et les Vertebres. Paris, A Delahaye et E Lacrosnier, 1874–1885).
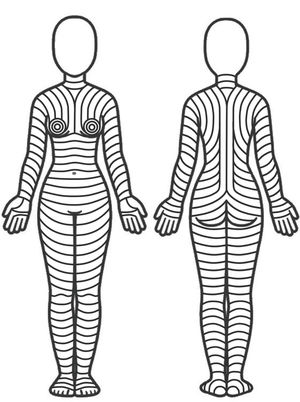
Circular excision of a highly suspicious melanocytic lesion. A) Classic elliptical excision following the lymphatic drainage. B) Circular excision without removing Burow's triangles. C) The circular defect is closed following the skin main folding lines without removing the resulting standing cones. This to not impair lymphatic drainage and spare healthy tissue.
The authors declare no conflict of interest.