A 44-year-old man who smoked 20 cigarettes per day was referred from the rheumatology department, where he had been under investigation for arthritis and Raynaud phenomenon, which affected the fingers of both hands and the toes of the right foot. This condition had developed several months earlier after the appearance of painful migratory lesions on the lower limbs.
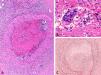
Physical ExaminationOn examination, erythematous nodules were observed in a linear distribution on both ankles (Fig. 1), and there were violaceous macular lesions with a necrotic appearance on the pads of the fingers (Fig. 2.)
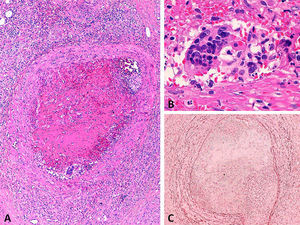
HistopathologyBiopsy of one of the nodules revealed a medium-sized vessel in the superficial subcutaneous tissue, with an occlusive intraluminal thrombus. There was a mixed inflammatory infiltrate in the vessel wall and the adjacent fat (Fig. 3A), and a granulomatous reaction with multinucleated giant cells at the periphery of the thrombus (Fig. 3B). Orcein staining revealed elastic fibers throughout the full thickness of the vessel wall, confirming it to be a vein (Fig. 3C).
Additional TestsCapillaroscopy was normal. Laboratory tests (blood and urine, basic biochemistry, viral serology, tumor markers, tests for hypercoagulability, and screening for autoimmune disease and cyroglobulins) were negative or normal and echocardiography was unremarkable. Arteriography was requested.
¿What Is Your Diagnosis?
DiagnosisThromboangiitis obliterans (Buerger disease).
Clinical Course and TreatmentArteriography of the upper limbs revealed occlusion of both ulnar arteries; the palmar arch arising from the radial arteries was incomplete and there was a near total absence of distal vasculature. The arterial study revealed no involvement above the elbow. The patient stopped smoking and the lesions gradually improved.
CommentThromboangiitis obliterans is a segmental, nonatherosclerotic, occlusive inflammatory vascular disease of the small and medium-sized arteries and veins of the extremities. This disease primarily affects young male smokers and is most prevalent in Asian and Eastern Europe populations.1
Though its pathogenesis is unclear, tobacco use is central to the initiation and progression of the disease. Thromboangiitis obliterans is considered a smoking-related autoimmune process that affects genetically predisposed patients.2
Clinical manifestations are due to distal ischemia, and the main symptom is pain at rest. The disease presents as painful digital ulcers accompanied by cyanosis and coldness, which can progress to gangrene and require amputation of the affected limb. Some cases, including the one described here, are suggestive of a connective tissue disease, as they initiate with arthritis and Raynaud phenomenon.3 Raynaud phenomenon and/or migratory thrombophlebitis of superficial veins occur in 40% of patients. Although rare, the visceral arteries (mesenteric, coronary, retinal, cerebral, pulmonary, or renal) may be affected.4
Biopsy, which will reveal an inflammatory occlusive thrombus, is rarely indicated. The biopsy is most likely to be diagnostic in the acute phase of the disease and in a vessel from an area of superficial thrombophlebitis,1 as occurred in the present case.
In cases with no pathognomonic signs or symptoms, the diagnosis is one of exclusion.1 Although no clear consensus has been reached, a number of diagnostic criteria have been proposed: young male smoker (under 45 years of age) with signs and symptoms of distal ischemia of the extremities (intermittent claudication, pain at rest, ischemic ulcers, or gangrene), absence of connective tissue disease, hypercoagulability or diabetes mellitus, the exclusion a proximal source of emboli by echocardiography, and a compatible arteriography.5 Arteriography is characterized by segmental lesions with abrupt arterial occlusion, gradual tapering (mouse tail) of the lumen, and collateral circulation with ‘corkscrew’ morphology.
Cessation of smoking is the only means of slowing the progression of the disease and avoiding amputation.1 Even the use of nicotine patches or gum may be sufficient to maintain disease activity. The goal of treatment in refractory cases is to relieve intractable pain and avoid amputation by debridement and the administration of analgesics, antiplatelet drugs, and antibiotics. Alternative approaches include prostaglandin infusion, sympathectomy, revascularization (a very limited technique due to poor distal beds), and the administration of immunosuppressants and vascular endothelial growth factor analogs. The response is variable.6
Please cite this article as: Floristán M, et al. Fumador con fenómeno de Raynaud y nódulos dolorosos en las piernas. Actas Dermosifiliogr. 2013;104:717–8.