Cutaneous hemangiomas are the most frequent benign tumors in children. When they affect the lumbar and perineal area some cases can be associated with an occult spinal dysraphism. The management of these hemangiomas lack consensus. We report 3 cases of children with lumbosacral and perineal hemangiomas with magnetic resonance image abnormalities and we review the literature to find out the type and timing of tests that should be performed to complete the study in these patients. Ultrasound is typically requested as young as possible, as this imaging technique is not possible 11the posterior spinal elements have ossified. MRI is the gold standard for diagnosing occult spinal dysraphism. According to the literature, the mean age for MRI screening should be around 6 months, when the fat formation in the filum terminale is expanded. In our opinion, an MRI scan should be performed at 6 months of age in every children with lumbar or perineal hemangioma regardless the lesion size, neurological symptoms or the ultrasound results.
Los hemangiomas infantiles son los tumores benignos más frecuentes en la población pediátrica. Cuando afectan al área lumbar y perineal, algunos casos pueden asociarse a alguna malformación subyacente como una disrafia espinal oculta. El manejo de estos hemangiomas carece de consenso. Describimos 3 casos de niños con hemangiomas lumbosacros y perineales con anomalías en la resonancia magnética y revisamos la literatura para valorar qué pruebas y en qué momento se deben realizar para completar el estudio en estos pacientes. Por lo general, se solicita una ecografía lo más precozmente posible, ya que esta técnica no es posible realizarla una vez que los elementos espinales posteriores se han osificado, lo que generalmente ocurre a los 6 meses de edad. La resonancia magnética es la prueba de referencia para diagnosticar una disrafia espinal oculta. De acuerdo con la literatura, la edad media para este examen debe ser alrededor de los 6 meses, cuando la formación de grasa en el filum terminale se ha visto incrementada. En nuestra opinión, se debería realizar una resonancia magnética a los 6 meses de edad en todos los niños con hemangioma lumbar o perineal, independientemente del tamaño de la lesión, la ausencia de síntomas neurológicos o los resultados de la ecografía.
Cutaneous hemangiomas are the most frequent benign tumors in the pediatric population, occurring in up to 10 percent of children by 1 year of age. They appear especially in the head and neck, and just the 10 percent of them in the perineal area.1 These hemangiomas are more affected with complications as ulceration, bleeding or infection, due to the direct contact with urine or feces, and are more likely to be treated with propranolol.2 Most hemangiomas regress spontaneously, so no additional tests are usually needed,3 but in the lumbar and perineal area some cases can be associated with congenital anomalies, including anorectal, urinary tract, spine, and external genitalia malformations, especially in the segmental forms4–9 where the published data show that up to 35% of them are associated with an underlying malformation.10 There is sufficient information showing that midline hemangiomas that overlie the spine, particularly in the lumbar region, can be associated with occult spinal dysraphism (OSD), that is why they are considered as high-risk skin lesions together with hypertrichosis, subcutaneous lipoma and caudal appendage,11,12 and when there are present a combination of 2 or more, it establishes the strongest indicator of an underlying dysraphic malformation.13
In 2006, Girard et al.14 proposed the acronym PELVIS syndrome (perineal hemangiomas, external genitalia malformations, lipomyelomeningocele, vesicorenal abnormalities, imperforate anus, and skin tag) to describe 2 cases with extensive sacral and perineal hemangiomas associated with severe malformation of the external genitalia, urinary tract and imperforate anus. After this publication, other acronyms have been proposed to describe similar clinical entities, with the name of SACRAL or LUMBAR syndrome.15–17 In the literature, most described cases of hemangiomas with associated malformations are those with extensive cutaneous lesions, affecting an important area of the perineum or lumbosacral area, in which the neuroimaging study is expected to be made,14 although when to do it is not clear. Nevertheless, when the lesions are little in size, do not deviate the middle line or have no additional signs or symptoms, the management and evaluation is not well established without consensus about the tests that should be performed in order to complete the study.
Case 1A healthy 2-month-old girl was admitted to our dermatology department because she developed a lumbar infantile hemangioma. She had no previous known illnesses, had an unremarkable gestation, and was born at term by normal spontaneous vaginal delivery. Her parents were nonconsanguineous and there was no family history of birth defects.
The cutaneous examination revealed a segmental lumbosacral hemangioma with deviation of the middle line to the left side (fig. 1), without any other associated skin lesion or neurological sign. After a general physical exam treatment with propranolol was started. After a few doses, the patient presented repeated episodes of hypotension so the treatment was stopped and continued with clinical follow up.
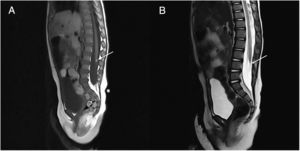
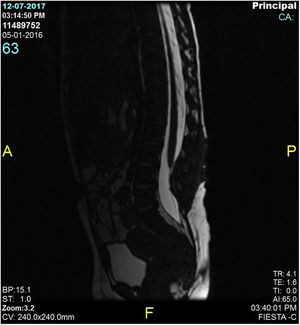
In the initial evaluation a lumbar ultrasound (US) was made showing no structural anomalies. A few months later, the lesion decreased in size but we decided to request a magnetic resonance image (MRI) to complete the study. The MRI demonstrated a 4mm lipoma in association with the conus medullaris and the filum terminale with tethered cord (fig. 2). We extend the study to other urologic anomalies resulting negative. The girl was derived to pediatric neurosurgery for evaluation where she was operated performing a medullary repair of the tethered cord (fig. 3) with good response and normal psychomotor development.
Case 2A 5-month-old boy presented to our dermatology department with a hemangioma overlying the sacral region. He was otherwise healthy and was born after a full-term uneventful gestation.
At the clinical examination he had a 4cm ulcerated hemangioma in the intergluteal fold (fig. 4). The lesion did not deviate the middle line. The mother referred that the lesion ulcerated 2 days before the dermatological revision. He had no other clinical sign or symptom. After a normal physical exam he started treatment with propranolol with good tolerance.
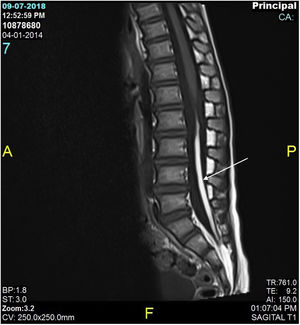
We requested a US that revealed a persistent dermal sinus and a MRI that showed a filum terminale lipoma (fig. 5). With these findings we also performed a urological evaluation that resulted normal. The patient was sent to the pediatric neurosurgery unit for evaluation where they decided to maintain follow up due to the normal neurological clinic.
Case 3A 1-month-old boy who came to our department for presenting a sacral hemangioma, with no other associated clinic. Son of healthy parents, had a uncomplicated pregnancy and delivery. The physical examination showed an ulcerated hemangioma of 3cm with presence of sacral fossa and asymmetry of the intergluteal fold. Treatment with propranolol was started with a very good response. A study was performed with ultrasound that result normal and later MRI that demonstrates the presence of a lipoma of the filum terminale without tethered cord (fig. 6). He was derived to pediatric neurosurgery for evaluation, who decide on conservative management and follow-up.
DiscussionIn the literature, there are few publications concerning the specific neuroimaging study and timing in children with lumbar or perineal hemangiomas. Some authors who have published reports that associate hemangiomas with internal malformations suggest that patients with large hemangiomas of the perineal area, even if neurologically asymptomatic, should have a kidney, abdominal and medullar US performed to rule out a malformation18; others propose a spine MRI to detect spinal dysraphism14 and a pelvic MRI to detect other internal anomalies,16,19 without clarifying the most appropriate moment of these studies. Other authors also suggest that every infant with lumbosacral segmental hemangiomas should undergo a systematic research of OSD and should have performed a medullar US before the 4 months of age, ideally in the neonatal period, and a lumbosacral MRI when the infant is older than 4 months17,20 in order to avoid late neurologic symptoms that can be hardly treated.21,22
In 1989, Albright et al.3 described 6 patients with vast perineal hemangiomas studied with MRI and 1 with myelogram. Three infants had a midline lumbar skin defect, another a subcutaneous lipoma under the hemangioma, and a last one a midline dermal sinus associated with the hemangioma. Despite their normal neurological status, all patients were diagnosed with tethered spinal cords, 4 also with intraspinal lipomas, and 2 with tight filum terminale. Based on these outcomes, the authors proposed that screening for big sized perineal hemangiomas should include an MRI scan to rule out tethered spinal cords.
Many years later, a multicenter prospective study of 41 children with lumbosacral midline hemangioma >2,5cm who underwent a MRI found that the relative risk for patients with lumbosacral infantile hemangiomas for spinal anomalies was 640 with a positive predictive value of 51.2%. In the same study the authors compare the results between US and MRI resulting the first one in a false-negative rate of 50%. Cohen's kappa coefficient for agreement between US and MRI was 0.27, showing a level of agreement consistent with chance. The results of this study demonstrate a significant increased risk of spinal abnormalities in the infants with midline lumbosacral hemangioma, and also that spinal US scanning, even when performed before a child is 4 months of age, is not a sufficiently sensitive screening instrument for this high-risk scenery, so these children should undergo MRI as part of their evaluation.10 The same conclusion had been made in the literature when comparing US and MRI,13 like the publication of Brent et al.23 in 2017. They studied 522 infants who had undergone MRI of the lumbar spine to screen for OSD of whom the 5% had a hemangioma as the indication of the imaging study. The rate of OSD ranged from 12% for patients with asymmetrically deviated gluteal crease to 55% for those with other isolated cutaneous stigmata. In the hemangioma group, the 15% had OSD, one of them complex. They compared their results with other previously published study where the US was the main imaging tool, concluding that the prevalence of OSD identified with modern high-resolution MRI screening is significantly higher than that reported with US screening24,25 because of the improved contrast resolution of the first and the low sensitivity of the second.
Another retrospective study have classified the different types of spinal anomalies associated with cutaneous lumbosacral hemangiomas. They included children with hemangiomas >2.5cm associated to spinal dysraphism in the MRI. They analyzed 20 cases and found tethered cord in 60%, spinal lipoma in 50%, intraspinal hemangiomas in 45% and sinus tract was found in 40% of children. With this information they recommended a imaging protocol of MRI sequences of the thoracolumbar junction and lumbosacral spine in the background of cutaneous lumbosacral hemangioma.26
MRI is the gold standard for diagnosing OSD. The best time for testing structural anomalies is not well established. Some authors consider that if there is no evidence of a sinus tract, ulceration, or neurologic signs or symptoms at presentation, MRI can be postponed until 4 to 6 months of age.10 If older are the children when the MRI is performed it allows a better study of the anatomy and a better toleration of sedation if needed. According to the literature, the mean age for MRI screening should be around 6 months, when the fat formation in the filum terminale is expanded. On the other hand, US is typically requested as young as possible, as this imaging technique is not possible once the posterior spinal elements have ossified, which usually occurs by 6 months of age,23 reason why some authors consider US as a fist-line screening test and the MRI only in the case of limitation or abnormality of this study.27
ConclusionThe management of midline lumbosacral and perineal hemangiomas lack consensus.28 We report 3 new cases to the literature of children with hemangiomas in these locations with good evolution. All children where neurologically asymptomatic but despite this, a MRI scan of the lumbar area was performed. In the 3 cases a filum terminale lipoma was revealed and in one of them a tethered spinal cord was found that ended in surgery. Based on our findings, the literature review, and paying special attention in understanding the normal development of children who will show delayed presentation of symptoms, and knowing the usefulness of each image instrument associated with the development of the lumbar area of children, we consider that a MRI scan should be performed at 6 months of age in every children with lumbar or perineal hemangioma regardless the lesion size, absence of neurological symptoms or the ultrasound results.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Subiabre-Ferrer D, García-Rabasco A, Correa-González N, Ortiz-Salvador JM, Barreda-Solana M. Papel de la resonancia magnética en niños con hemangiomas lumbosacros y perineales: informe de 3casos clínicos y revisión de la literatura Eczema y urticaria en Portugal. 2019;110:728–733.