Porokeratosis is a skin keratinization disorder that gives rise to a number of clinical variants; the underlying disorder can be acquired or hereditary. Clinically, it presents as a macule or annular plaque characterized by a central atrophic patch surrounded by a clearly defined hyperkeratotic border. Histology shows a compact parakeratotic column known as a cornoid lamella. The various clinical forms of the disease are defined by the number and distribution of the lesions: porokeratosis of Mibelli, disseminated superficial actinic porokeratosis, linear porokeratosis, porokeratosis palmaris et plantaris disseminata, and punctate porokeratosis. Although the lesions are benign, some of their characteristics are associated with a greater risk of malignant transformation, hence the importance of deciding how to approach these lesions and knowing the different therapeutic options available.
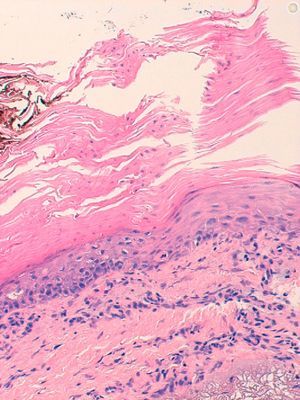
We report the case of an 82-year-old woman with no relevant personal medical history, who visited our department with a skin lesion on the anterior aspect of her left leg that had grown gradually over 2-3 years. The solitary, erythematous, rounded plaque measuring 4×3cm had well defined margins and was covered by a whitish scale (Fig. 1). The results of a skin biopsy revealed cornoid lamellae with no signs of cellular atypia (Fig. 2). On the basis of both the clinical examination and histology report, a diagnosis of porokeratosis of Mibelli was established. Because of the size and location of the lesion, photodynamic therapy (PDT) was proposed as a good therapeutic option. A cream containing methyl 5-aminolevulinate (MAL) was applied to the lesion, which was then covered with occlusive dressings for 3hours. The cream used was Metvix. Upon removal of the dressings, the whole surface of the lesion was observed to emit intense red fluorescence under ultraviolet light. The lesion was then exposed to red light from an LED lamp (Aktilite, 37J/cm2) for 9minutes. Two weeks later, the area of treated skin was ulcerated, perhaps as a result of exposure of the lesion to sunlight a few hours after the treatment; a new session of PDT was therefore ruled out and local therapies were prescribed. Three months after the PDT session, the lesion had almost completely resolved and only a slightly erythematous, crusted area remained (Fig. 3).
The pathogenesis of porokeratosis is still poorly understood and the disorder is thought to be the result of the proliferation of abnormal clones of keratinocytes induced by the interaction of genetic factors, immunosuppression, and environmental triggers such as exposure to sunlight. The association with irradiation explains why the lesions are more often located in sun-exposed areas of the body and are more evident in summer.1,2 Although these chronic lesions are benign, all clinical forms of porokeratosis are associated with some risk of malignant transformation. Large, long-standing, or linear lesions and those that present in elderly or immunocompromised patients have the greatest risk of malignant transformation.2 Reported neoplasms, in order of frequency, are Bowen disease, epidermoid carcinoma, and basal cell carcinoma.1,2 Because of the risk of malignancy, it is important to consider the best approach to take when presented with this dermatosis and to know the different therapeutic options available.
The fact that many different therapies are used is indicative of the lack of an ideal treatment that is safe and effective; each case should therefore be evaluated on an individual basis. In the case of multiple, disseminated lesions, the most appropriate approach may be watchful waiting and biopsy of the lesions in which malignant transformation is suspected.2 Usual treatments include the following: calcipotriol, tacalcitol, 5-fluorouracil, imiquimod, topical and systemic retinoids, laser therapy, cryotherapy, dermabrasion, and surgical excision.1,2 PDT is approved for the treatment of actinic keratosis, superficial and nodular basal cell carcinoma, and Bowen disease. Its use has recently been extended to a number of infectious and inflammatory skin disorders and certain cancers; the results reported to date indicate varying degrees of efficacy.3 PDT has been used to treat porokeratosis on the basis of the clinical and histological similarities between this disorder and actinic keratosis. Moreover, it is a safe, well tolerated technique associated with good cosmetic results and minimal side effects. However, the results of the few documented cases are contradictory. Most studies have been carried out in patients with disseminated superficial actinic porokeratosis and various photosensitizing agents have been used (δ-aminolevulinic acid, MAL, and hypericin), all with poor results. The lesions resolved in only 1 case,4 and improved slightly or remained unchanged in the others.5–7 In the literature, we found only 1 case of porokeratosis of Mibelli that had been successfully treated with PDT. Unlike our case, those authors used a single session of PDT with MAL and blue light in combination with daily application of 5-fluorouracil cream.1 While the normal PDT regimen in the treatment of most skin disorders involves more than 1 session, we were only able to apply a single session in the present case owing to the appearance of side effects, and this may explain the incomplete response obtained. However, it is also possible that the immunomodulatory effect of PDT and the inflammation already present in the lesion (visible in the clinical and histological images) may have favored a good therapeutic response with just 1 session. Ulceration is a rare adverse event,8 and its appearance was probably due in some measure to the fact that the patient was an elderly woman and the leg was exposed to sunlight after treatment, contrary to express instructions.
In conclusion, we report a case of porokeratosis of Mibelli in which treatment with PDT obtained a partial response. Nevertheless, because the results achieved with photodynamic therapy in the treatment of porokeratosis are highly varied, we believe that further studies with larger series of cases are needed if we are to reach clear conclusions regarding its utility in this setting.
Please cite this article as: Gutiérrez Paredes E, et al. Poroqueratosis de mibelli, ¿ una nueva indicación de la terapia fotodinámica? Actas Dermosifiliogr. 2013;104:259–61.