Fox-Fordyce disease (FFD), or apocrine miliaria, is a rare inflammatory disease of the apocrine glands characterized by the presence of pruritic follicular papules in apocrine-rich areas of the skin. We present a case of histologically confirmed FFD with extensive involvement of 2 unusual sites, the chest and abdomen.
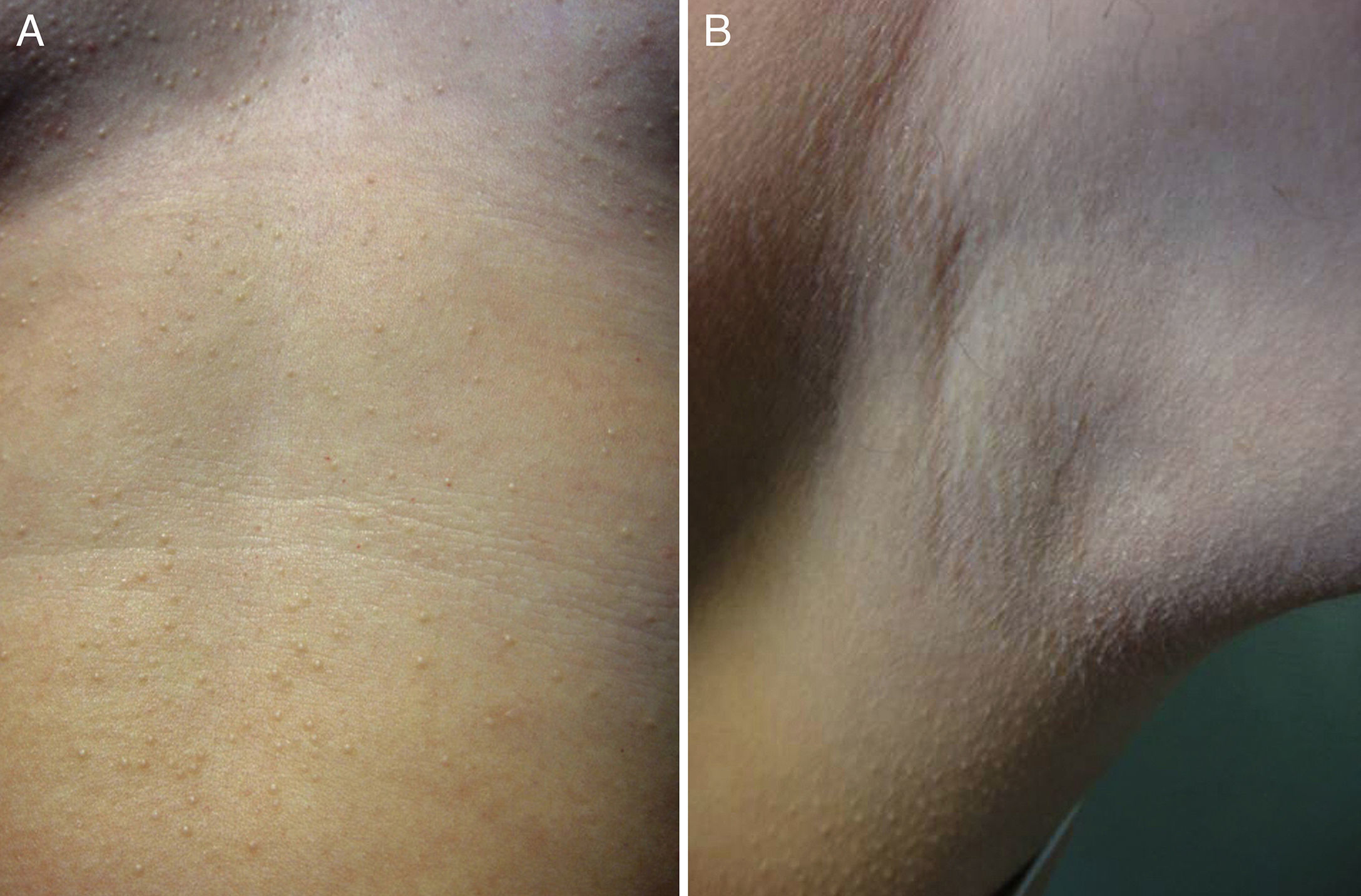
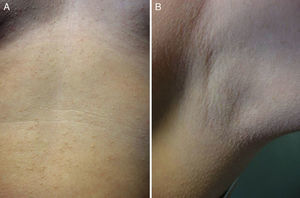
A 39-year-old woman was referred for evaluation of an asymptomatic rash that had appeared 2 years earlier. There was no significant personal or family medical history. The rash had first appeared in the presternal area and had then spread over the abdomen to the pubic region. The rash consisted of multiple minute nonconfluent red-to-yellow papules on the breasts and especially the lower chest and abdomen, as far as the pubic region (Fig. 1). The axillae, areolae, and genitals were uninvolved.
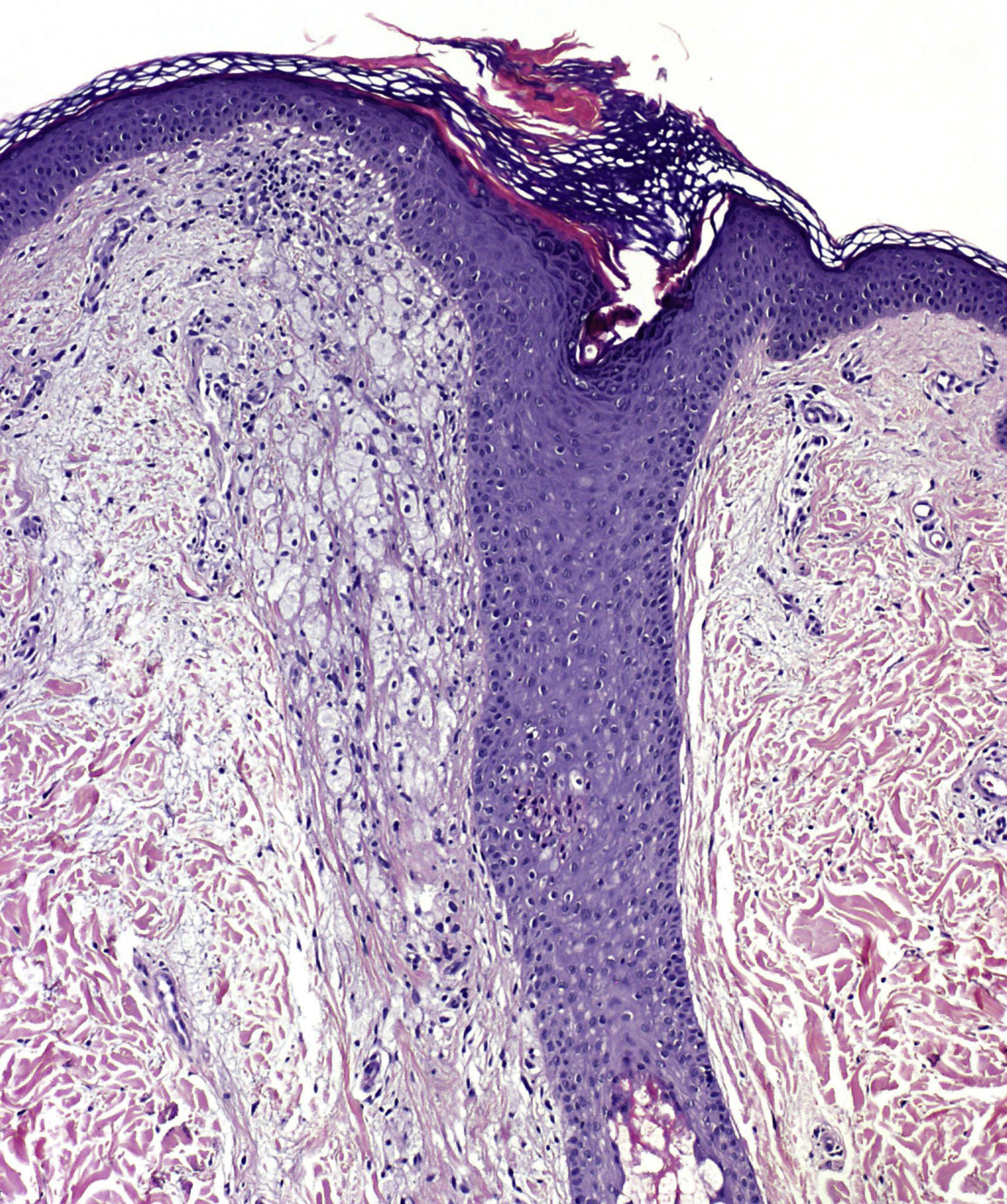
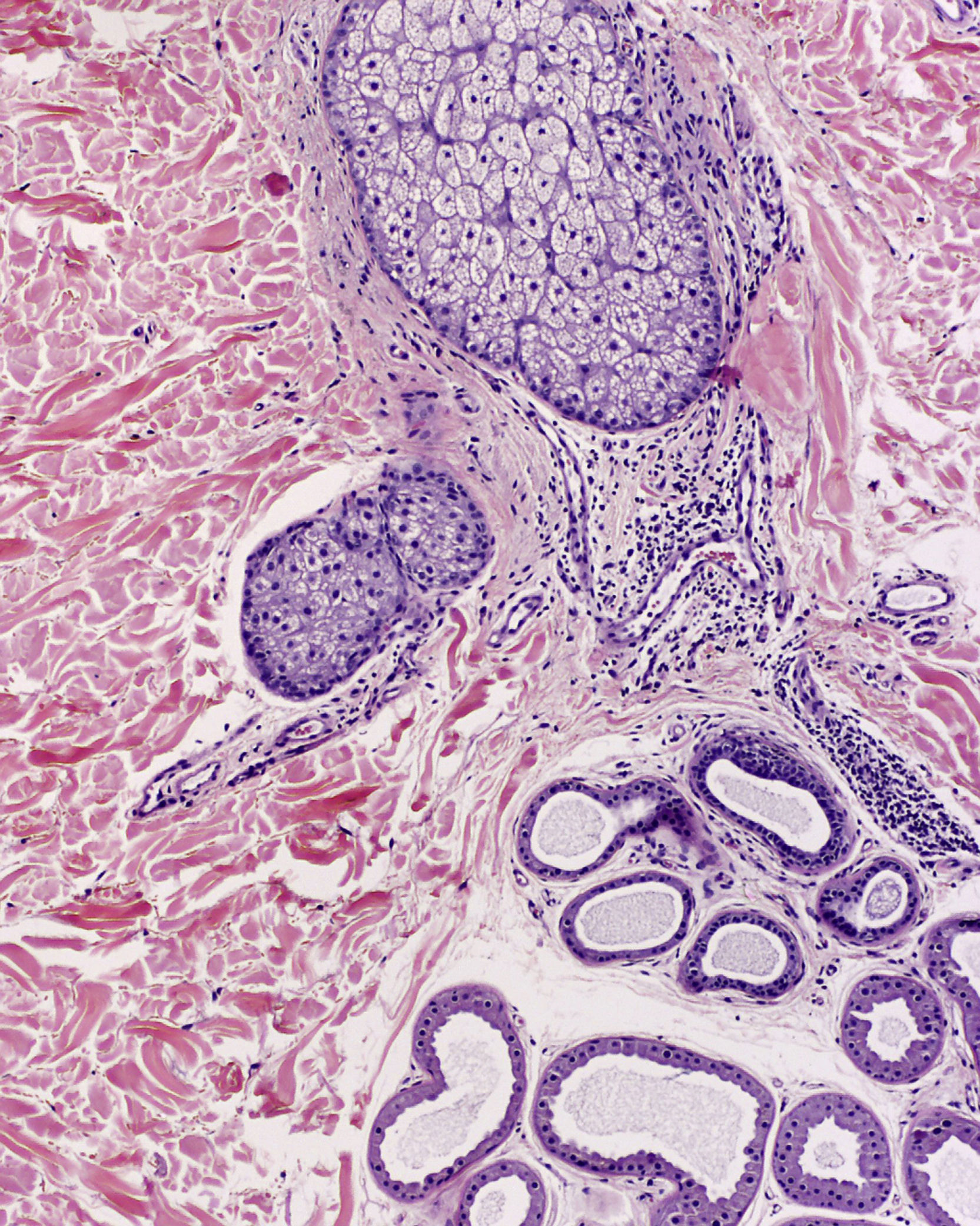
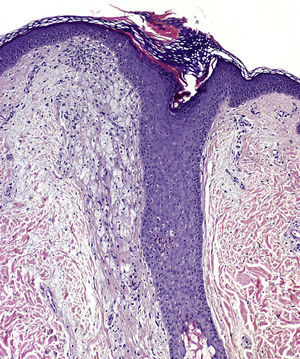
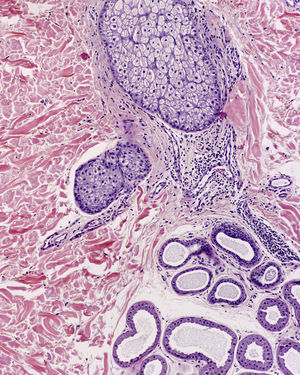
Histologic examination of a papule from the lower presternal region revealed dilatation and hyperkeratotic plugging of the follicular infundibulum, which was surrounded by abundant foamy histiocytes (xanthomized macrophages) (Fig. 2); a mild-to-moderate periadnexal chronic lymphocytic inflammatory response; and clusters of apocrine cells, with a tendency to cystic dilatation, between the reticular dermis and hypodermis (Fig. 3).
There were no relevant findings in the blood panel and the basic hormone panel, which included testosterone, dehydroepiandrosterone sulfate, progesterone, estradiol, luteinizing hormone, and follicle-stimulating hormone.
No improvement was noted after successive attempts at topical treatment with tretinoin, corticosteroids, and clindamycin.
FFD was first described by Fox and Fordyce in 1902.1 This rare skin condition is most common in women aged 13 to 35 years. The etiology and pathogenesis of FFD are unknown, although genetic, endocrine, environmental, and metabolic factors have been proposed.2 Plugging of the apocrine duct at its point of entry in the follicular infundibulum appears to be the chief factor involved in the development of FFD. Plugging is thought to cause secretions to accumulate and then extravasate into the infundibulum and the peri-infundibular dermis, leading to a secondary inflammatory response that largely consists of macrophage recruitment.3
Clinical presentation usually includes multiple white-to-yellow follicular papules symmetrically located in characteristic regions with an abundance of apocrine glands.4 Lesions are frequently pruritic and worsen in the summer months and at times of emotional stress. Involved areas show little body hair growth and no sweating.
FFD chiefly manifests in areas rich in apocrine glands: the axillae, mammary areolae, periumbilical region, mons pubis, labia minora, scrotum, foreskin, perianal region, free margins of the eyelids, and external ears. Apocrine glands are sparsely present in all other skin regions, especially the trunk and head,5 but FFD has only occasionally been reported in sites other than those listed. Unusual reported locations include the presternal and periumbilical regions and internal surface of the thighs.6,7
The defining histopathologic features of FFD vary widely. Descriptions include dilatation and hyperkeratosis of the follicular infundibulum, spongiosis and dyskeratosis of the infundibular epithelium, vacuolar degeneration of the dermoepidermal junction, presence of periadnexal inflammatory lymphocytic infiltrate, parakeratosis of the infundibular epithelium in the form of cornoid lamellae, dilatation of the apocrine glands, and perifollicular xanthomatosis. The last is considered among the most characteristic findings.3,8,9
Generally speaking, treatment of FFD is less than satisfactory, and the condition is typically chronic.6 Treatment approaches used with varying results include topical and intralesional corticosteroids, topical or systemic retinoids, topical antibiotics (such as clindamycin), oral contraceptives, and topical pimecrolimus.10 Highly refractory cases have sometimes led to surgical treatment, including electrocoagulation, excision, and liposuction.
In conclusion, we believe that FFD should be considered in the differential diagnosis of any progressive rash of red-to-yellow papules on the chest or abdomen. Clinically similar, easily confused conditions more frequently described at these sites include syringomas, steatocystoma multiplex, or lichen nitidus, and distinguishing them from FFD requires the correlation of both clinical and histologic findings.
Please cite this article as: Ballester I, López-Ávila Á, Ortiz S. Enfermedad de Fox-Fordyce con presentación clínica atípica. Actas Dermosifiliogr. 2013;104:832–834.