Verruciform xanthoma is a rare benign tumor first described by Shafer1 in 1971. It usually arises on the oral mucosa.
An 11-year-old boy was referred to our outpatient clinic for evaluation of a lesion that had been present on the tongue for 6 weeks and was slightly tender on palpation. The child had been diagnosed with acute myeloblastic leukemia 4 years earlier and had received 2 allogeneic bone marrow transplants, the first 3 months after the diagnosis and the second 3 years later. At the time we saw the patient, he was in complete remission, with full chimera of the transplant, and he had never presented signs of graft-versus-host disease (GVHD). He had not received immunosuppressant treatment for the previous 7 months.
Physical examination revealed an elevated, oval-shaped, sessile tumor with a long axis of about 2cm. The tumor was located on the left lateral surface of the tongue and had a whitish, verrucous surface that was not ulcerated (Fig. 1).
Two months before the lesion appeared, asymptomatic reactivation of Epstein-Barr virus (EBV) infection had been detected, evidenced by an increase in the viral load on serial measurements performed as part of the routine follow-up of the patient's hematologic disease.
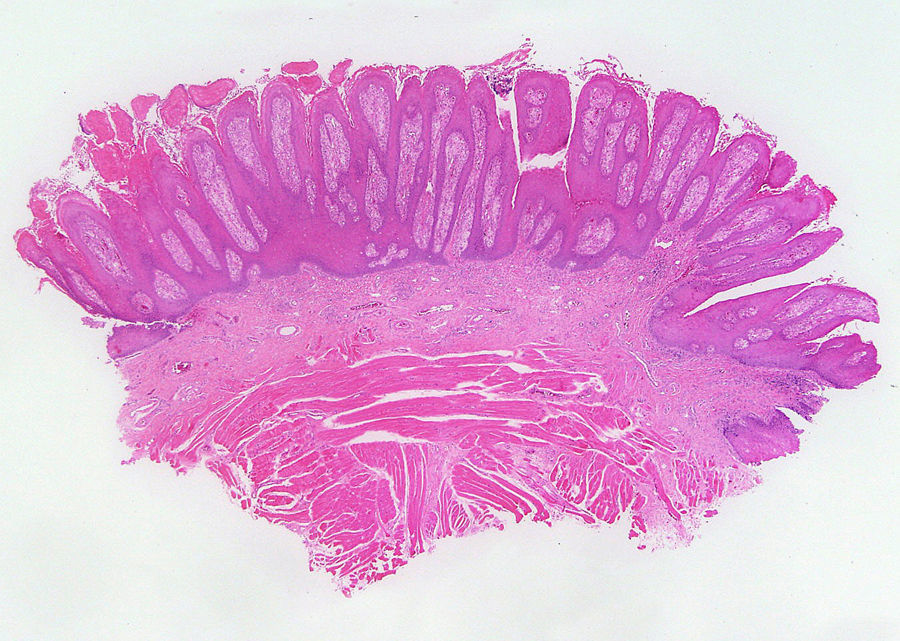
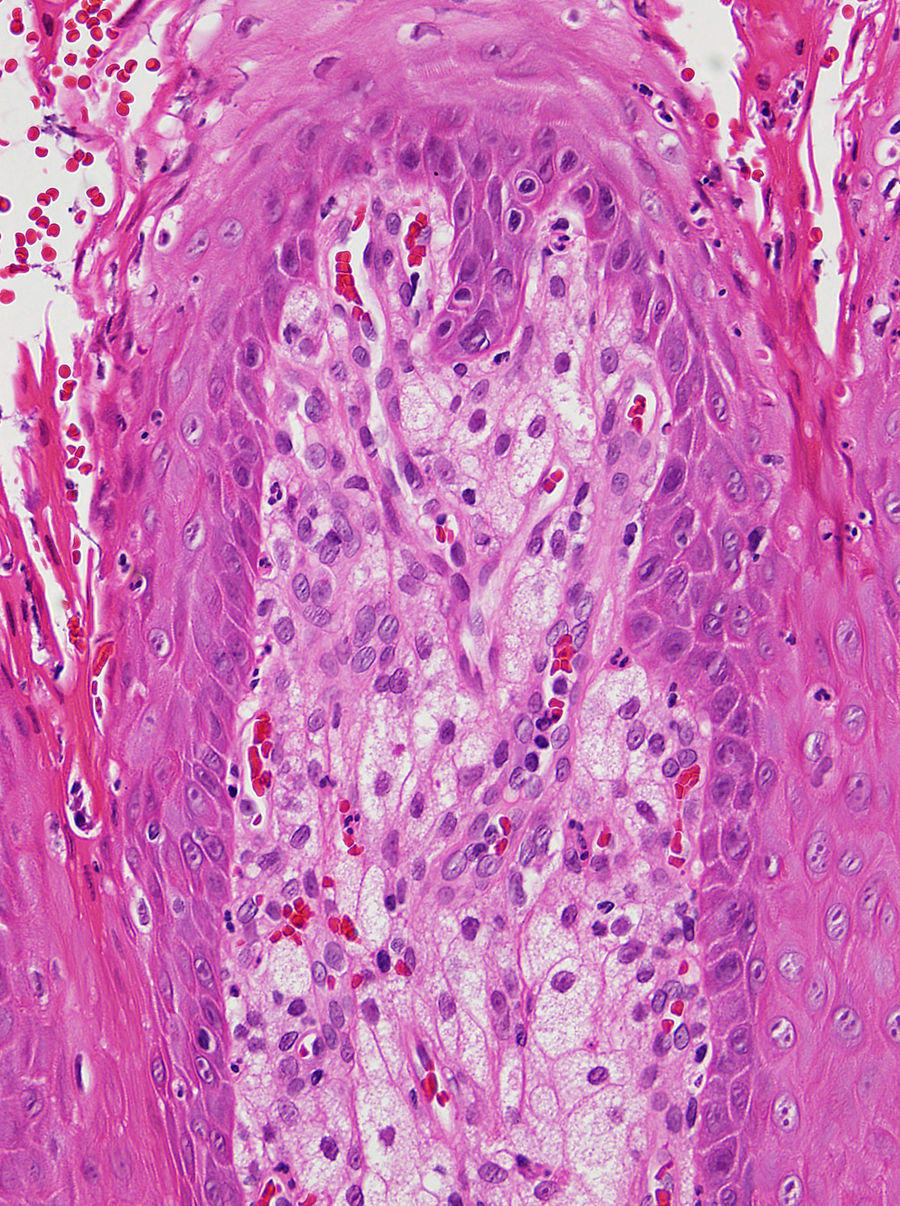
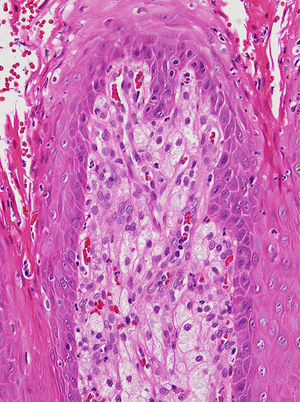
Biopsy showed verrucous acanthosis with hyperkeratosis and isolated plaques of parakeratosis, and there were numerous foamy histiocytes in the dermal papillae (Figs. 2 and 3). The lesion was diagnosed as verrucous xanthoma.
The tumor was completely excised and there were no signs of recurrence during 2 months of follow-up.
Verrucous xanthoma usually presents clinically as a slow-growing asymptomatic lesion with a yellowish, reddish, or gray color, a rough surface with a granular or papillomatous appearance, a sessile or pedunculated base, and it can measure up to 2cm in diameter.2,3 The most common site is the oral mucosa,2 although it can also arise on the genitalia4,5 or, more rarely, on other sites of the skin. Approximately 70% of such tumors arising on the oral mucosa are located on the masticatory mucosa, followed by the hard palate and the tongue, as in our case.3 There have also been isolated cases of multifocal involvement of the skin and mucosas.6
With regard to the epidemiology of the tumor, it can occur at any age, though there is a slightly higher prevalence in middle age (40-60 years).2 Under 50 years of age, the incidence is slightly higher in men whereas, in the population over 50 years, these tumors are slightly more common in women; overall, the frequency is practically the same in men and women.3
The clinical differential diagnosis should include condyloma acuminatum, common warts, and squamous cell carcinoma (including the verrucous form).2 In our case, in view of the recent reactivation of EVB infection, we also considered the possibility of lymphoma.7
Histology of verrucous xanthoma reveals a hyperkeratotic squamous epithelium with focal parakeratosis and no cellular atypia; foam cells are observed between elongated epithelial crests.2,6 These cells present a granular cytoplasm and the nucleus is typically eccentric. Immunohistochemistry of these cells is intensely positive for CD68 and negative for S-100.2,3 Three histopathological patterns have been described: verrucous, papillary, and flat. The verrucous pattern is the most common.3
The pathological differential diagnosis includes the common wart, lichen simplex chronicus, and eruptive xanthoma.8 There have been no previous reports of an association between this tumor and infection with EBV. However, there have been descriptions of patients in whom this lesion has arisen on previous mucosal or cutaneous lesions, such as oral lichen planus or mucosal GVHD.3 Our patient did not have GVHD affecting the mucosa or any other previous lesions of the oral mucosa.
The etiology and pathogenesis of verrucous xanthoma is not fully understood. It has been suggested that it may be an inflammatory reaction secondary to recurrent trauma, as the lesions mainly arise on areas subject to friction,9 or that the accumulation of foam cells in the dermis is the primary trigger, though no association with disorders of lipid metabolism has been found in the majority of the cases.6 No pathogenic role of the papillomavirus has been demonstrated.9 Given the known association between EBV and the induction of other lesions of the oral mucosa, such as oral hairy leukoplakia, in immunosuppressed patients, we considered the possibility that the appearance of this lesion could have been related to reactivation of this virus in our patient.7 However, no pathogenic relationship between EBV and verrucous xanthoma has been described to date, and this could therefore be an incidental finding in our case.
The treatment of choice is surgical excision of the lesion and recurrence is extremely rare.3
In summary, we have presented the case of a patient with a lingual tumor having the typical clinical and histopathological features of verrucous xanthoma. The patient presented recent reactivation of EBV infection, an association not previously described in the literature and which could therefore be a casual finding.
Please cite this article as: Maldonado-Cid P, et al. Xantoma verruciforme asociado a reactivación de virus de Epstein-Barr. Actas Dermosifiliogr 2013;104:445–6.