A healthy newborn infant aged 12hours, of Ecuadorian origin and with no family history of melanoma or other tumors of interest, was referred for evaluation of a congenital lesion of the nail of the third finger of the left hand. The infant had not suffered any birth or postnatal trauma to the affected finger.
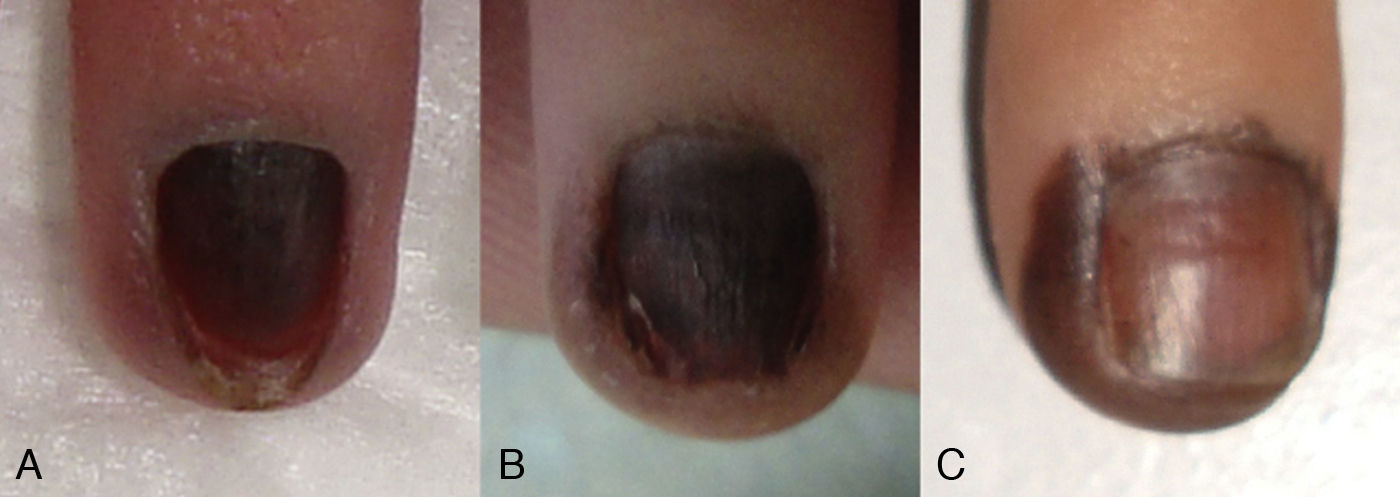
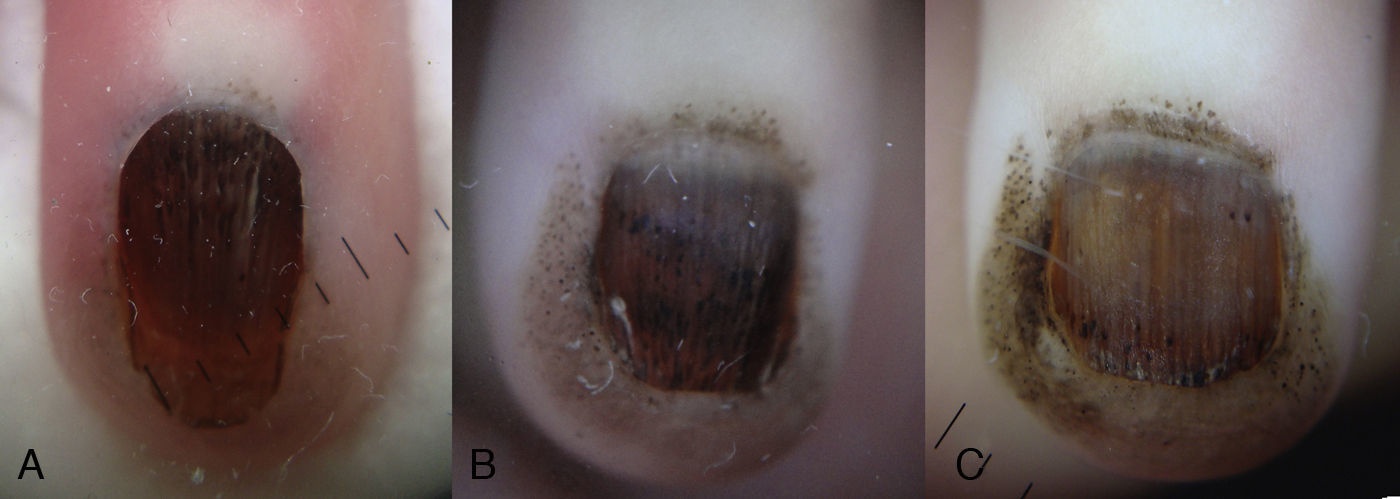
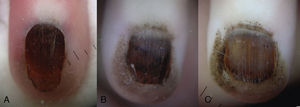
Physical examination showed practically the whole nail surface to be a homogeneous erythematous-brown color (Fig. 1A). Dermoscopy revealed black globules arranged linearly on the brown background of the nail plate and a marked gray periungual pigmentation with brown globules (Fig. 2A). Correlation of the clinical and dermoscopic findings suggested melanocytic nevus of the nail matrix as the most likely diagnosis, although other melanocytic lesions or hemorrhage could not be excluded at that time. Given the apparent benign nature of the lesion, it was decided to keep the infant under close observation.
A, The initial dermoscopy revealed the presence of pigmented globules in the nail plate and in the proximal periungual skin. B, Two months later, pigmented globules were visible on a brown background, with narrow and regular longitudinal lines in the nail plate. C, At 6 months the dermoscopic pattern was unchanged.
Two months later the pigmented area had spread beyond the borders of the nail plate and there was clear involvement of the periungual skin (Fig. 1B). Dermoscopy of this new situation revealed pigmented globules on a light-brown background in the periungual skin, narrow and regular longitudinal lines in the nail plate, and globules of black pigment most numerous in the distal third of the plate (Fig. 2B).
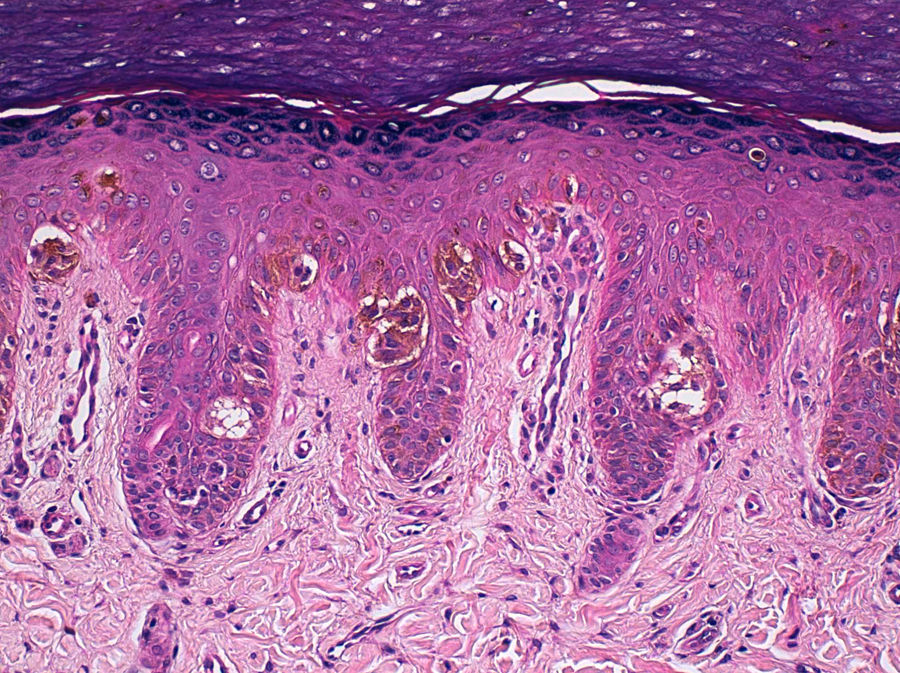
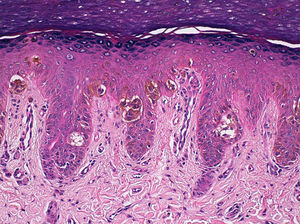
Punch biopsy of the hyponychium was performed and histology revealed a junctional melanocytic proliferation of benign appearance, with melanocytes grouped in nests and as isolated cells in the epidermis (Fig. 3). Histology of a distal fragment of the nail plate showed deposits of melanin. The final diagnosis was periungual and subungual congenital melanocytic nevus (CMN). After 6 months of follow-up the periungual component of the nevus had become more evident but the size of the lesion was unchanged (Fig. 1C and Fig. 2C).
Epidermal hyperplasia and a proliferation of melanocytes with small nuclei and no atypia or pleomorphism; the melanocytes were arranged in nests of different sizes in the deep part of the epithelium and also as individual cells with a pagetoid distribution in the superficial layers of the epithelium (hematoxylin-eosin, original magnification x100).
Periungual and subungual CMN is a very rare entity, with only 2 previous descriptions in the literature.1,2
The lesion presents clinically as a homogeneous pigmentation of the nail plate. Usually it increases in size to affect the periungual skin, a finding that supports the diagnosis of a pigmented melanocytic lesion. Our case is the first in which the dermoscopic features of this type of lesion have been reported; the dermoscopic pattern is similar to that of CMNs at other sites, with pigmented globules of irregular size and distribution clearly visible on a background of homogeneous pigmentation.3 The total melanonychia and the presence of globules in subungual CMNs are due to participation of the nail bed epidermis in the formation of part of the nail plate. The narrow longitudinal lines can be explained by involvement of the nail matrix.4
In contrast to the usual histopathological features of CMNs, in which the dermal component predominates, subungual and periungual CMNs are characterized mainly by junctional melanocytic proliferations. In our case there were also isolated intraepidermal melanocytes.
The differential diagnosis must include disorders of various origins, including melanocytic lesions (ungual lentigo, nevus of the nail matrix, subungual blue nevus, ungual melanoma), racial pigmentation, drug-induced pigmentation, endocrine disorders, trauma, and hemorrhage.5 Histology of the nail plate is a simple and nontraumatic way to differentiate between melanic and hematic origins of the pigment deposits in the nail. In subungual CMNs, the early presence of proximal periungual pigment may be erroneously interpreted as a positive Hutchinson or pseudo-Hutchinson sign, observed respectively in acral melanomas and nail matrix nevus.6 However, the absence of mottled striate melanonychia and the presence of pigmented globules are features more commonly associated with a diagnosis of CMN.
It is often impossible to exclude melanoma histologically in acral and subungual melanocytic lesions, particularly in children, due either to the use of partial biopsies or the unusual characteristics of acral melanocytic nevi in children, which can present isolated nuclear atypia and even a pagetoid distribution of some of the melanocytes.7 In cases of melanonychia in which malignancy is suspected (a broad band of pigment, Hutchinson sign, irregular dermoscopic features, a dark-skinned patient), the lesion must therefore be completely excised.7,8
The management of pigmented nail lesions will therefore depend on whether the rare but very serious childhood acral lentiginous melanoma is suspected.9,10 Dermoscopic and clinical follow-up should be reserved for lesions with low-risk features (narrow bands, uniform dermoscopic characteristics, no changes over time). In such cases, meticulous periodic follow-up (by dermoscopy and a photographic record) would appear to be the most suitable option, as it would avoid the potential cosmetic and functional sequelae of excision or biopsy.5,7,8
In conclusion, we have presented the third case of subungual and periungual CMN to be reported in the literature. Knowledge of this entity can help to prevent aggressive treatments (wide excision, amputation) due to the overdiagnosis of childhood acral lentiginous melanoma.
Our thanks to Dr. Antonio Torrelo of Hospital Niño Jesús in Madrid, Spain.
Please cite this article as: Agusti-Mejias A, et al. Nevus melanocítico congénito subungueal y periungueal. Actas Dermosi-filiogr. 2013;104:446-8.