Accurate subtyping of basal cell carcinoma (BCC) is crucial for the effective management of this disease and it is particularly important to distinguish between aggressive and nonaggressive histologic variants. Histologic subtype is not always accurately identified by biopsy and this can have serious implications. High-resolution ultrasound (HRUS) is a recent technique that has proven to be of value in differentiating between variants of BCC. The aim of this study was to investigate the potential usefulness of HRUS for detecting invasive disease in recurrent BCC treated nonsurgically following an initial diagnosis of noninvasive BCC by biopsy.
Material and methodsThis was a prospective observational study of consecutive cases of BCC with clinical suspicion of recurrence following nonsurgical treatment and a pretreatment diagnosis of superficial BCC by punch biopsy. Before surgical excision, the recurrent lesions were evaluated by HRUS followed by a punch biopsy of the site of suspected recurrence. The diagnostic agreement between HRUS, punch biopsy, and excisional biopsy was then evaluated.
ResultsEight lesions were studied. HRUS identified invasive disease in 3 of the 4 cases that were incorrectly classified as superficial subtypes by punch biopsy.
ConclusionHRUS could be useful for detecting persistent tumor after nonsurgical treatment and for choosing the site most likely to harbor invasive disease for punch biopsy.
La determinación del subtipo histológico de carcinoma basocelular (CBC) es crucial en el adecuado abordaje del mismo (sobre todo diferenciar variantes agresivas de no agresivas). En ocasiones la biopsia falla en la correcta catalogación del mismo con sus conocidas consecuencias. La ecografía cutánea de alta frecuencia (ECAF) es una técnica reciente que ha mostrado potencialidad en la distinción de variantes de CBC. El objetivo del estudio fue mostrar la posible utilidad de la ECAF en la identificación de la invasividad del CBC recurrente tras tratamientos no quirúrgicos diagnosticados mediante biopsia como no invasivos.
Material y métodosEstudio observacional, prospectivo de casos consecutivos de CBC con sospecha clínica de recurrencia tras tratamiento no quirúrgico y que previamente a dicho tratamiento habían sido diagnosticados por biopsia-punch como variantes superficiales. Previamente a la extirpación quirúrgica de los mismos se realizó una ecografía de la lesión y posteriormente un punch de la zona sospechosa de persistencia. Finalmente se estudió la tasa de concordancia entre los resultados diagnósticos de cada una de las pruebas (ECAF, biopsia-punch y biopsia escisional).
ResultadosSe incluyeron 8 casos. De entre los 4 casos en los que la biopsia-punch realizó una mala clasificación de invasividad (eran realmente subtipos invasivos pero la biopsia-punch determinó subtipos superficiales), la ECAF fue capaz de detectar dicha invasividad en 3 de ellos.
ConclusiónLa ECAF podría ser de utilidad en la detección de persistencias tumorales de CBC tras tratamientos no quirúrgicos, permitiendo guiar la biopsia-punch en la detección del área más sospechosa de infiltración.
Basal cell carcinoma (BCC) is the most common type of cancer in white people. Consequently, some authors have defined it as a health problem of epidemic characteristics that is associated with considerable health care spending.1 Diagnosis has traditionally been based on punch biopsy, although this approach could lead to an erroneous histologic classification—aggressive subtypes classified as nonaggressive—with severe consequences for therapy and prognosis.2–6 High-resolution ultrasound (HRUS) is a recent technique that is still being investigated and has proven to be of value in the diagnosis and management of BCC. The potential of HRUS has been evaluated mainly in the measurement of tumor dimensions and mapping of presurgical margins, and although differential ultrasound patterns have been reported for subtypes of BCC, this aspect has received less attention.7–15 The objective of the present study was to show the potential usefulness of HRUS for identifying invasive disease in recurrent BCC after nonsurgical treatment of tumors diagnosed as noninvasive by biopsy.
Material and MethodsWe performed an observational prospective study of consecutive cases of BCC with clinical suspicion of recurrence following nonsurgical treatment and a pretreatment diagnosis of superficial BCC by punch biopsy. The patients were seen at the Skin Cancer Clinic of the Department of Dermatology of Hospital Costa del Sol, Marbella, Spain between September 2012 and June 2013. The inclusion criteria were those set out above (ie, recurrent BCC after nonsurgical treatment that was not previously classed as noninvasive with biopsy), and the exclusion criteria were refusal or inability to undergo an ultrasound study after clinical evidence of recurrence.
The methodology applied was as follows: in cases of suspected residual BCC after nonsurgical treatment, the lesion was analyzed using HRUS (DermascanC- 20 mHz [resolution 60×200μm], Cortex Technology). A punch biopsy was then performed of the portion that was clinically and dermoscopically suspected of invasiveness. The clinical and dermoscopic criteria for selection of the tumor area to be biopsied were that it had to present arborizing telangiectasias, brown-blue-gray ovoid nests, or ulceration.16,17 The lesion was then surgically removed, and serial sections were taken for study. Finally, the diagnostic agreement of the results (invasive vs noninvasive) obtained by HRUS, punch biopsy, and excisional biopsy was compared.
In histologic terms, the superficial and the expansive/nodular variants of BCC were considered noninvasive, and the remainder were considered invasive.
Differential ultrasound patterns of subtypes were detected based on relevant publications.8,9,15,18 Thus, the superficial subtype was defined as a heterogeneous, hypoechoic, flattened, solid tumor with irregular borders; the nodular subtype was similar to the superficial subtype, although it was oval in shape; the infiltrative subtype was described as having irregular hypoechoic bands that originate in the main tumor mass and invade the underlying dermis; and in the morpheaform subtype, increased echogenicity was described around the main hypoechoic tumor mass and attributed to the increased fibrosis that is characteristic of these tumors. Multiple large intralesional hyperechoic spots have also been considered possible characteristics of BCC.15 Specifically, large cotton wool–like hyperechoic spots seem to be typical of this type of tumor and are attributed to the presence of cysts, calcification, and clusters of apoptotic cells in the interior.15
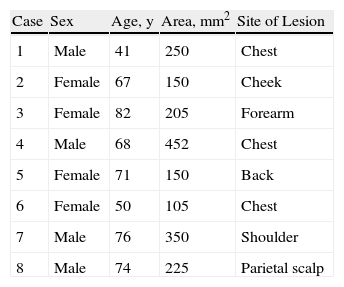
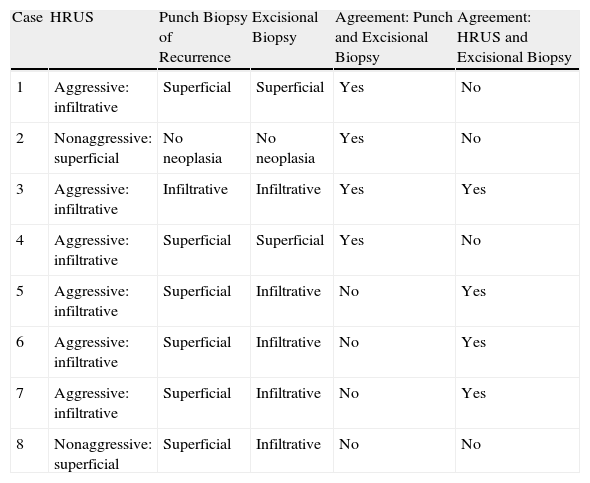
ResultsThe study population comprised 8 patients, 7 of whom had received photodynamic therapy and 1 cryotherapy. Table 1 shows the clinical characteristics of the cases studied. Mean age was 66.12 years (range, 41-82); 4 were women and 4 were men. Most lesions were found on the trunk (5 of 8), and the mean surface of the lesions was 235.87 mm2 (range, 105-452).
The results for the different diagnostic approaches (Table 2) showed that the overall diagnostic agreement between each of the pre-excisional tests (punch biopsy and HRUS) and excisional biopsy was similar (4 of 8 cases).
Results of the Diagnostic Tests.
| Case | HRUS | Punch Biopsy of Recurrence | Excisional Biopsy | Agreement: Punch and Excisional Biopsy | Agreement: HRUS and Excisional Biopsy |
| 1 | Aggressive: infiltrative | Superficial | Superficial | Yes | No |
| 2 | Nonaggressive: superficial | No neoplasia | No neoplasia | Yes | No |
| 3 | Aggressive: infiltrative | Infiltrative | Infiltrative | Yes | Yes |
| 4 | Aggressive: infiltrative | Superficial | Superficial | Yes | No |
| 5 | Aggressive: infiltrative | Superficial | Infiltrative | No | Yes |
| 6 | Aggressive: infiltrative | Superficial | Infiltrative | No | Yes |
| 7 | Aggressive: infiltrative | Superficial | Infiltrative | No | Yes |
| 8 | Nonaggressive: superficial | Superficial | Infiltrative | No | No |
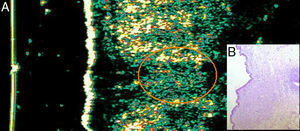
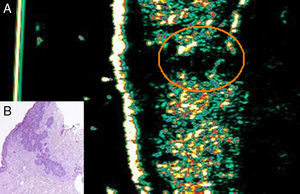
According to the ultrasound patterns described above, HRUS identified 3 of the 4 cases of invasive disease that went undetected with punch biopsy (Figs. 1 and 2). Only 1 false negative was obtained for detection of invasiveness (case 8), and the case went undetected using punch biopsy (Fig. 3). Similarly, 2 false positives were found for detection of invasiveness: case 1, which was associated with intense perilesional fibrosis, and case 4, which involved an accompanying inflamed infundibular cyst (Fig. 4).
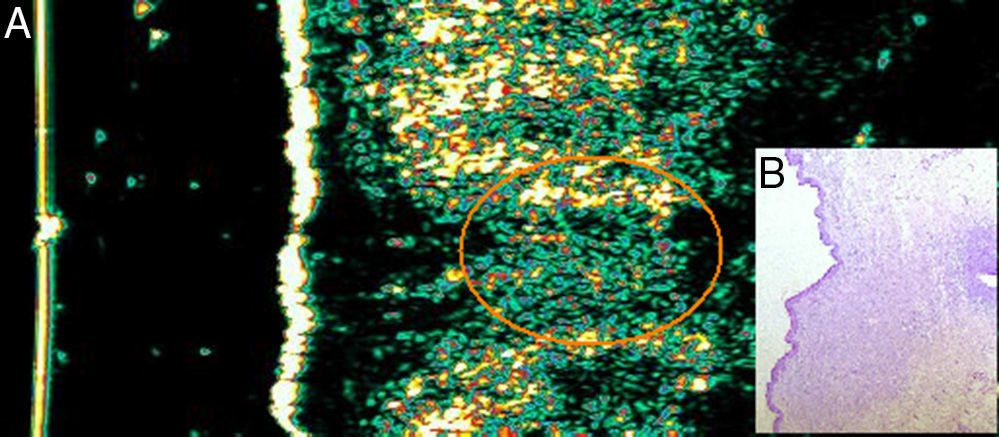
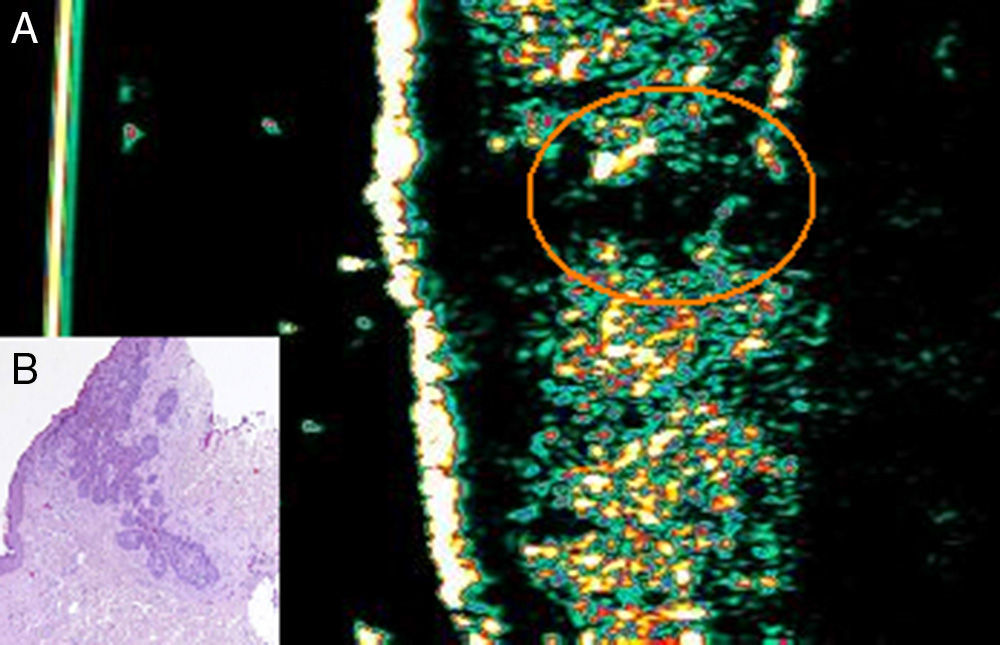
Case 5. Woman aged 71 years with basal cell carcinoma on her back. A, Ultrasound image (20Mhz) of the lesion showing a poorly defined subepidermal oval hypoechoic structure, from which arises a poorly defined hypoechoic extension that invades the underlying dermis and is compatible with infiltration. B, Histologic image of the lesion (hematoxylin-eosin, original magnification×4). The nests of basaloid cells infiltrating the underlying dermis are compatible with infiltrative basal cell carcinoma.
Case 6. Woman aged 50 with basal cell carcinoma on her chest. A, Ultrasound image (20Mhz) of the lesion showing a flattened subepidermal hypoechoic structure, underneath which we can see another poorly defined hypoechoic formation that invades the underlying dermis until it reaches the dermal-epidermal junction and is suggestive of inflammation (orange circle). B, Histologic image of the lesion (hematoxylin-eosin, original magnification×10) showing the infiltrative component invading the underlying dermis.
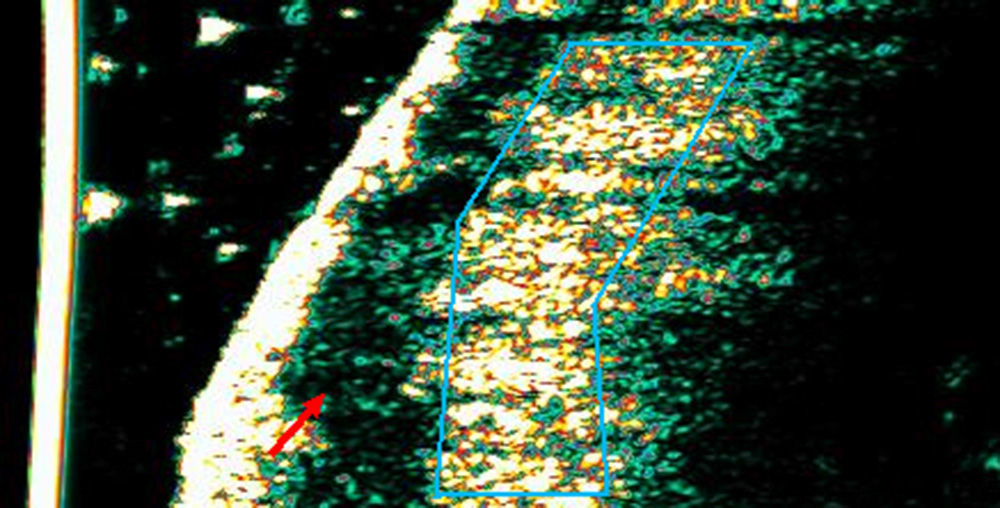
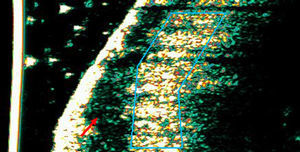
Case 8. Man aged 74 years with basal cell carcinoma on the parietal scalp. A, Ultrasound image (20Mhz) of the lesion showing a flattened subepidermal hypoechoic structure with no hypoechoic extensions invading the underlying dermis suggestive of inflammation (red arrow). The area highlighted in blue shows intense hyperechogenicity in the dermis representing intense fibrosis. This may be the reason why tumor infiltration was not detected.
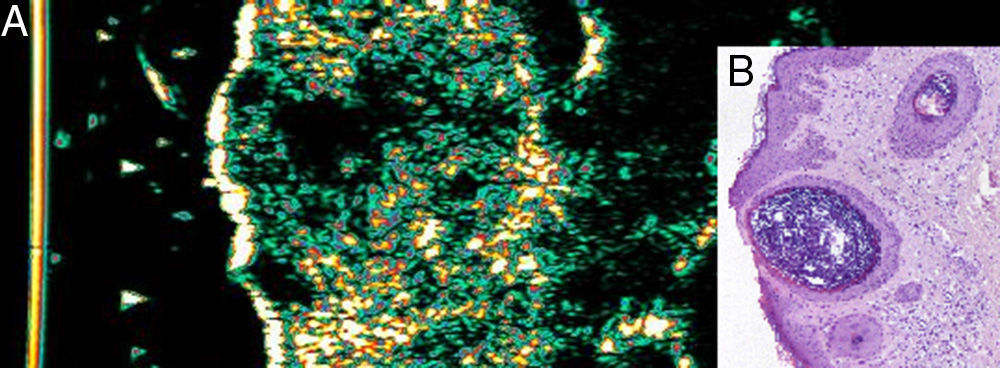
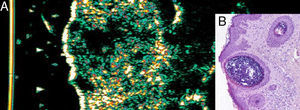
Case 4. Man aged 68 with basal cell carcinoma on his chest. A, Ultrasound image (20Mhz) showing an irregular subepidermal hypoechoic structure with poorly defined margins and deep irregular hypoechoic extensions suggestive of infiltration. B, Histologic image of the lesion (hematoxylin-eosin, original magnification ×10) showing the presence of an inflamed infundibular cyst adjacent to the lesion that was incorrectly interpreted as tumor infiltration in the skin ultrasound.
Special mention should be made of case 2, in which HRUS made it possible to diagnose superficial BCC that was not confirmed with punch biopsy or excisional biopsy.
DiscussionOverall diagnostic agreement for punch and excisional biopsy obtained in the present study (50%) is even lower than that recorded in the literature, where the rate ranges between 52% and 89% depending on the series.2 If the cases that were incorrectly classified by punch biopsy (4/8) are analyzed separately, it can be seen that they were all invasive variants previously classified as superficial. The findings in several extensive case series show that up to 21% of BCCs that had initially been diagnosed as superficial by punch biopsy were later shown to be infiltrative after analysis of the excised tissue.3 Consequently, approximately 1 in every 5 BCCs diagnosed in the clinic as superficial or noninvasive using punch biopsy is in fact an invasive form.
Incisional biopsy, therefore, hampers differentiation between aggressive and nonaggressive forms.4 Even though agreement with excisional biopsy is considered relatively good in BCCs of a single histologic type, the rate falls considerably in mixed cases (from 83% to 37%, respectively),2 and it is difficult to detect the most aggressive type, since a high percentage of BCCs (between 18% and up to more than 50%, depending on the series) are, in fact, mixed subtypes.5,6 In clinical practice, underestimation of aggressive variants leads to prescription of inappropriate therapy and, therefore, health care spending and emotional cost for the patient.6
Our results for incorrect classification of invasiveness with punch biopsy are higher than those reported in the literature, and this difference is easily explained by the type of BCC studied (recurrent or persistent). Moreover, the difference could account for the failure of the nonaggressive treatments administered, as suggested by several authors who consider incorrect histologic classification one of the main reasons for recurrence in patients who receive noninvasive treatments such as topical imiquimod or photodynamic therapy.2
HRUS could help to ensure correct histologic classification of BCC, as suggested in recent studies that attempted to define ultrasound patterns that differentiate between subtypes.8,9,15
In our series, the ultrasound patterns obtained are consistent with those described in the literature, although intralesional hyperechoic spots were not detected. When false negatives and false positives are analyzed separately, we see that in case 8 (false negative), invasive disease may have gone undetected because of the intense perilesional fibrosis masking the infiltration (Fig. 3). With respect to the false positive results obtained, the false infiltration detected in case 1 could be attributed to the underlying inflammatory infiltrate with intense perilesional fibrosis; furthermore, in case 4, the incorrect interpretation of infiltration was attributed to the presence of an adjacent inflamed infundibular cyst, a finding that has been reported elsewhere.8 Finally, case 2 is an example of a residual tumor that was erroneously diagnosed. HRUS revealed marked elastosis in the perilesional skin, which is observed as a flattened subepidermal hypoechoic band and could have been the reason why the residual tumor was incorrectly interpreted.
Detailed analysis of false negatives and false positives is essential in ultrasound assessment of lesions, since correct identification during the ultrasound examination would have improved the sensitivity of the test. In fact, recent studies8,18 report 2 rare ultrasound artifacts: the so-called angled border, which is formed by an inflammatory infiltrate underlying the tumor, and the “blurry” border, which is produced by hypertrophy of the sebaceous glands adjacent to the tumor (finding in case 4).
The main limitations of our study are its small sample size, the lack of an assessment of tumor vessels using Doppler ultrasound (which could have increased the diagnostic sensitivity of the skin ultrasound), and the need for a solid grounding in the technique before users are able to detect this type of lesion.
In conclusion, HRUS could prove useful in the detection of residual BCC after nonsurgical treatment, thus making it possible to guide punch biopsy at the sites most suspected of being invaded. The technique could therefore be helpful in appropriate planning of therapy to treat this type of tumor. However, studies with larger sample sizes are necessary to confirm these preliminary findings and to establish sensitivity, specificity, positive predictive values, and negative predictive values for the technique.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Ethical DisclosuresProtection of persons and animals:The authors declare that this research did not involve experiments performed on humans or animals.
Confidentiality of dataThe authors declare that they have followed their hospital's protocol on the publication of data concerning patients and that all patients included in the study have received sufficient information and have given their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare that no private patient data are disclosed in this article.
Please cite this article as: Hernández-Ibáñez C, Aguilar-Bernier M, Fúnez-Liébana R, del Boz J, Blázquez N, de Troya M. Utilidad de la ecografía cutánea en el diagnóstico de invasividad del carcinoma basocelular recurrente tras tratamiento no quirúrgico. Actas Dermosifiliogr. 2014;105:935–939.