Pseudoxanthoma elasticum-like papillary dermal elastolysis (PXE-PDE) is a clinical-pathologic entity characterized by skin lesions similar to those of PXE itself in addition to the absence or marked loss of elastic fibers in the papillary dermis.1 We report a new case of PXE-PDE, focusing on its pathogenesis and clinical, pathologic, and dermatoscopic features. We also review the literature.
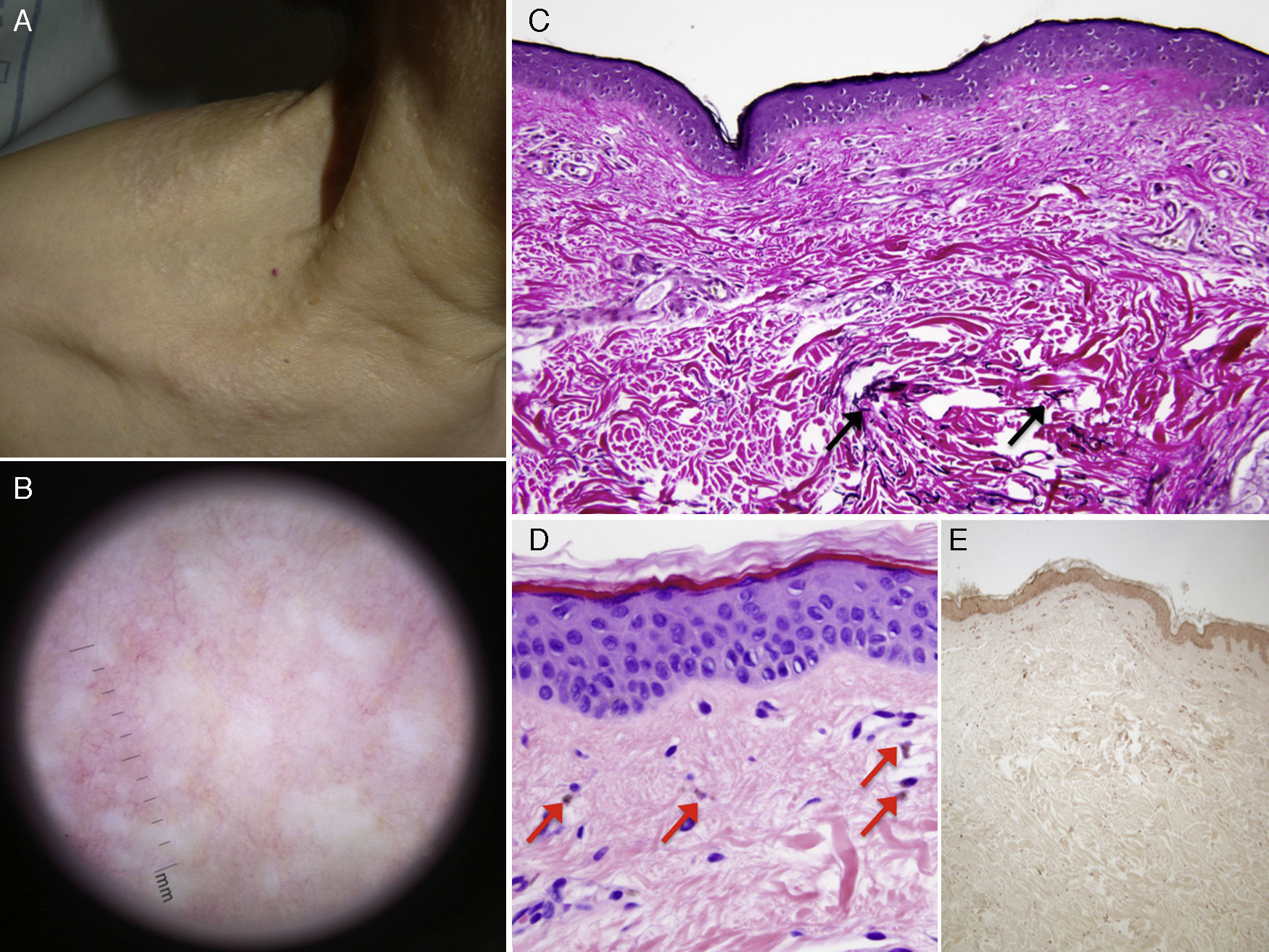
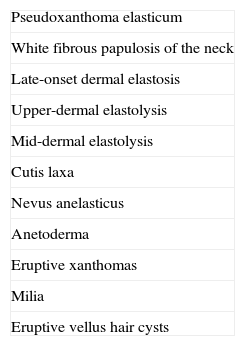
The patient was a 74-year-old woman with a history of chronic bronchiectasis since childhood, aortic insufficiency, and age-related macular degeneration. She presented with asymptomatic lesions on the neck and axillas that had appeared 4 months earlier. Physical examination revealed millimetric, nonfollicular, flesh-colored papules converging to form cobblestone-like plaques arranged symmetrically over the cervical, clavicular, and axillary regions (Fig. 1A). She reported no history of trauma, prolonged sun exposure, or use of topical treatments, and no relevant family history. Dermoscopy showed multiple areas of flesh-colored lesions, which tended to converge, and multiple branching vessels (Fig. 1B). Cardiology and ophthalmology evaluations yielded only findings related to underlying diseases. Hematoxylin and eosin staining revealed no specific findings, but orcein staining demonstrated nearly complete loss of elastic fibers; loss was confined to the papillary dermis (Fig. 1C). Papillary dermal telangiectasia and occasional dermal melanophages were also evident (Fig. 1D). Von Kossa staining was negative (Fig. 1E).
A, Millimetric nonfollicular papules, light brownish in color, converge to form plaques with a cobblestone pattern. B, Light-brownish areas tending to converge; multiple linear and branching vessels can be seen. C, Nearly total absence of elastic fibers in the papillary dermis; in contrast, elastic fibers (black arrows) can be seen in the reticular dermis (orcein, original magnification ×100). D, Melanophages (red arrows) dispersed in the papillary dermis (hematoxilin-eosin ×400). E, Von Kossa staining revealed no calcifications of elastic fibers (original magnification ×100).
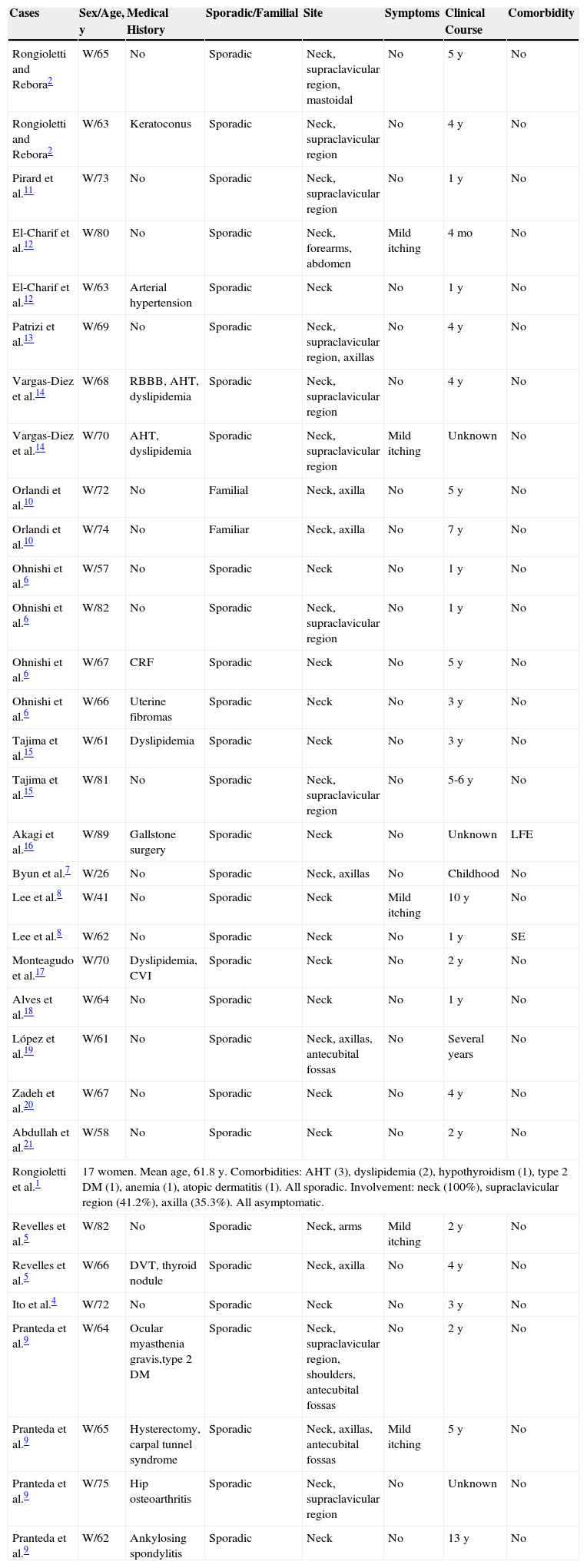
PXE-PDE is a rare condition of multifactorial etiopathogenesis that was described by Rongioletti and Rebora2 in 1992. Approximately 50 cases affecting women in their 50s or older have been published (Table 1).
Reports of Cases of Pseudoxanthoma Elasticum-like Papillary Dermal Elastolysis.
| Cases | Sex/Age, y | Medical History | Sporadic/Familial | Site | Symptoms | Clinical Course | Comorbidity |
|---|---|---|---|---|---|---|---|
| Rongioletti and Rebora2 | W/65 | No | Sporadic | Neck, supraclavicular region, mastoidal | No | 5 y | No |
| Rongioletti and Rebora2 | W/63 | Keratoconus | Sporadic | Neck, supraclavicular region | No | 4 y | No |
| Pirard et al.11 | W/73 | No | Sporadic | Neck, supraclavicular region | No | 1 y | No |
| El-Charif et al.12 | W/80 | No | Sporadic | Neck, forearms, abdomen | Mild itching | 4 mo | No |
| El-Charif et al.12 | W/63 | Arterial hypertension | Sporadic | Neck | No | 1 y | No |
| Patrizi et al.13 | W/69 | No | Sporadic | Neck, supraclavicular region, axillas | No | 4 y | No |
| Vargas-Diez et al.14 | W/68 | RBBB, AHT, dyslipidemia | Sporadic | Neck, supraclavicular region | No | 4 y | No |
| Vargas-Diez et al.14 | W/70 | AHT, dyslipidemia | Sporadic | Neck, supraclavicular region | Mild itching | Unknown | No |
| Orlandi et al.10 | W/72 | No | Familial | Neck, axilla | No | 5 y | No |
| Orlandi et al.10 | W/74 | No | Familiar | Neck, axilla | No | 7 y | No |
| Ohnishi et al.6 | W/57 | No | Sporadic | Neck | No | 1 y | No |
| Ohnishi et al.6 | W/82 | No | Sporadic | Neck, supraclavicular region | No | 1 y | No |
| Ohnishi et al.6 | W/67 | CRF | Sporadic | Neck | No | 5 y | No |
| Ohnishi et al.6 | W/66 | Uterine fibromas | Sporadic | Neck | No | 3 y | No |
| Tajima et al.15 | W/61 | Dyslipidemia | Sporadic | Neck | No | 3 y | No |
| Tajima et al.15 | W/81 | No | Sporadic | Neck, supraclavicular region | No | 5-6 y | No |
| Akagi et al.16 | W/89 | Gallstone surgery | Sporadic | Neck | No | Unknown | LFE |
| Byun et al.7 | W/26 | No | Sporadic | Neck, axillas | No | Childhood | No |
| Lee et al.8 | W/41 | No | Sporadic | Neck | Mild itching | 10 y | No |
| Lee et al.8 | W/62 | No | Sporadic | Neck | No | 1 y | SE |
| Monteagudo et al.17 | W/70 | Dyslipidemia, CVI | Sporadic | Neck | No | 2 y | No |
| Alves et al.18 | W/64 | No | Sporadic | Neck | No | 1 y | No |
| López et al.19 | W/61 | No | Sporadic | Neck, axillas, antecubital fossas | No | Several years | No |
| Zadeh et al.20 | W/67 | No | Sporadic | Neck | No | 4 y | No |
| Abdullah et al.21 | W/58 | No | Sporadic | Neck | No | 2 y | No |
| Rongioletti et al.1 | 17 women. Mean age, 61.8 y. Comorbidities: AHT (3), dyslipidemia (2), hypothyroidism (1), type 2 DM (1), anemia (1), atopic dermatitis (1). All sporadic. Involvement: neck (100%), supraclavicular region (41.2%), axilla (35.3%). All asymptomatic. | ||||||
| Revelles et al.5 | W/82 | No | Sporadic | Neck, arms | Mild itching | 2 y | No |
| Revelles et al.5 | W/66 | DVT, thyroid nodule | Sporadic | Neck, axilla | No | 4 y | No |
| Ito et al.4 | W/72 | No | Sporadic | Neck | No | 3 y | No |
| Pranteda et al.9 | W/64 | Ocular myasthenia gravis,type 2 DM | Sporadic | Neck, supraclavicular region, shoulders, antecubital fossas | No | 2 y | No |
| Pranteda et al.9 | W/65 | Hysterectomy, carpal tunnel syndrome | Sporadic | Neck, axillas, antecubital fossas | Mild itching | 5 y | No |
| Pranteda et al.9 | W/75 | Hip osteoarthritis | Sporadic | Neck, supraclavicular region | No | Unknown | No |
| Pranteda et al.9 | W/62 | Ankylosing spondylitis | Sporadic | Neck | No | 13 y | No |
Abbreviations: AHT, arterial hypertension; CRF, chronic renal failure; CVI, chronic venous insufficiency; DM, diabetes mellitus; DVT, deep vein thrombosis; LFE, linear focal elastosis; RBBB, right bundle-branch block; SE, solar elastosis.
This condition is characterized by millimetric, nonfollicular papules that tend to converge to form cobblestone-like plaques. Their distribution is symmetrical around the neck and in the area over the clavicle, and to a lesser degree in the axillas and antecubital fossas, and on the abdomen.1 The changes are asymptomatic and do not require treatment.
Unlike PXE, PXE-PDE has no associated systemic manifestations, although comorbidity typical of the patient's age (such as arterial hypertension, dyslipidemia, or diabetes mellitus) may be present.1 In our patient, the outstanding comorbidity was chronic bronchiectasis, a diagnosis that has not previously been reported in association with PXE-PDE, although it was present in one reported case of PXE.3 However, the involvement of elastic fibers in the pathogenesis of all 3 of these conditions seems to point to a common mechanism.
Dermoscopy reveals areas of light brownish colored papules, which tend to converge; multiple lineal and branched vessels are also observed.4
PXE-PDE is one of the so-called invisible dermatoses and diagnosis requires specific staining for elastic fibers (e.g., with Van Gieson or orcein stains)1 or serum testing with monoclonal antibodies against amyloid P component.5 Partial or total loss of elastic fibers in the papillary dermis below a normal or slightly atrophic epidermis will be evident.1,5 A finding of melanophages dispersed in the papillary dermis, as we saw in our patient, is useful for diagnosis.1 The calcified elastic fibers evident on Von Kossa staining in PXE are not found in PXE-PDE.1,5
Immunohistochemistry has demonstrated that the primary defect in these patients is the absence of elastin rather than fibrillin-1 (which is absent in control patients of advanced age as well as in patients with PXE-PDE).6
The etiology and pathogenesis of PXE-PDE is still being debated. Rongioletti and Rebora2 grouped PXE-PDE among the age-related elastic fiber syndromes; however, 2 cases have since been reported in young women7 and the syndrome has been found exclusively in women. A role for ultraviolet radiation, which has been discussed, is controversial given that skin not exposed to sunlight is sometimes involved, a history of overexposure to sunlight is not typically present, other skin lesions related to actinic damage are not observed in this context, and solar elastosis has only been reported in 1 case.1,5,8 Another hypothesis holds that PXE-PDE is the result of abnormal elastic fiber formation, given the observation of immature fibers in the upper reticular dermis or evidence of activated fibroblastomas.1,5 Pranteda et al.9 demonstrated that glucocorticoids may be involved in the pathogenesis of PXE-PDE, given their ability to reduce the expression of the elastin gene and its mRNA in human fibroblast cultures.9
Even though PXE-PDE is an acquired condition, the case of 2 sisters10 and the absence of cases in males suggests a genetic, hereditary, or hormonal factor that has not yet been identified.
Other elastolytic diseases (Table 2), particularly PXE, must be ruled out. PXE is hereditary, manifests after the second decade of life, is associated with systemic complications, particularly cardiovascular and ophthalmologic signs, and morbidity and mortality are high.
Differential Diagnosis of Pseudoxanthoma Elasticum-like Papillary Dermal Elastolysis.
| Pseudoxanthoma elasticum |
| White fibrous papulosis of the neck |
| Late-onset dermal elastosis |
| Upper-dermal elastolysis |
| Mid-dermal elastolysis |
| Cutis laxa |
| Nevus anelasticus |
| Anetoderma |
| Eruptive xanthomas |
| Milia |
| Eruptive vellus hair cysts |
In summary, PXE-PDE is essentially an acquired condition that is multifactorial, involving both genetic and environmental factors. Because it is asymptomatic, proper diagnosis is the priority, particularly for ruling out PXE so that patients can avoid unnecessary diagnostic and therapeutic procedures.
Please cite this article as: Vázquez-Osorio I, Rosón E, Suárez-Peñaranda JM, Vázquez-Veiga H. Elastólisis de la dermis papilar similar a pseudoxantoma elástico. Actas Dermosifiliogr. 2015;106:333–336.