Dowling-Degos disease (DDD) or reticular pigmented anomaly of the flexures is a rare autosomal dominant genodermatosis with variable penetrance.1–3 It mainly affects young women and is characterized by acquired reticular hyperpigmentation of the large skin folds. We present a case of DDD associated with hidradenitis suppurativa (HS) in a 43-year-old Spanish woman. Physical examination revealed brownish macules of 5-10mm diameter, with an irregular morphology, homogeneous pigmentation, and a reticular pattern, situated predominantly in the posterior cervical region (Fig. 1A) and inguinal and intergluteal folds (Fig.1B). In addition, she presented active HS lesions in both axillas (Fig. 2), as well as depressed pinpoint perioral scars suggestive of acne. The patient stated that her mother, 2 maternal uncles, and 1 of her sisters had similar lesions.
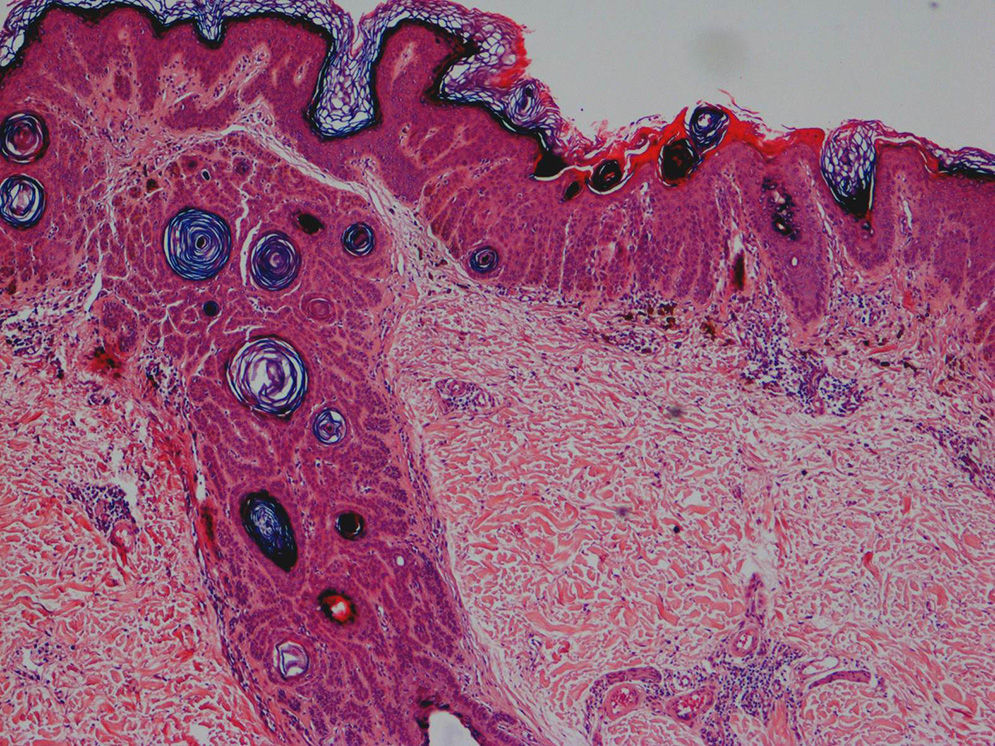
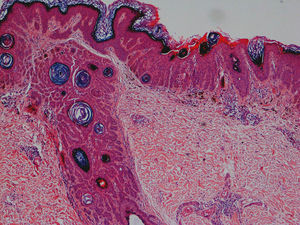
The dermatopathology study of a perianal skin lesion revealed basal hyperpigmentation, thin elongated digiform rete ridges, and suprapapillary thinning, as well as dermal melanophages and a mild perivascular lymphohistiocytic infiltrate (Fig. 3).
Based on these data, we made a diagnosis of DDD with associated HS. We offered topical therapy as the first option, but this was rejected by the patient. The disease has shown no significant change after more than 5years of follow-up.
DDD is a rare autosomal dominant genodermatosis that was first described by Behçet in 1932 as a variant of acanthosis nigricans of the axillas. Since then a number of cases of DDD have been reported, and there have been further revelations about its etiology, pathogenesis, and treatment.
DDD usually develops after puberty and tends to have a progressive course.2,3 It is characterized clinically by brownish hyperpigmented macules that adopt a reticular pattern. These macules are situated in the skin flexures (submammary, axillas, groin), cervical region, trunk, and anterior surface of the thighs and upper arms. The presence of pinpoint papules with keratin plugs simulating comedones is also common in the palmar, axillary, cervical, perioral, and gluteal regions. Furthermore, depressed perioral scars can develop,2,3 as was observed in our case.
Dermatologic histopathology is characteristic, showing interconnected hyperpigmented epidermal proliferations projecting in a filiform pattern into the dermis. This is called the “antler-like” pattern. Basal-layer melanocytes are present in normal numbers. Epidermal hyperplasia may be observed in the hair follicles, extending into the dermis, with the formation of plugs and follicular dilation. The other histologic feature is a mild perivascular lymphohistiocytic infiltrate. The key feature that differentiates DDD from other disorders of keratinization is the combination of hyperpigmented proliferations derived both from the epidermis and from the follicular wall.
The etiology and pathogenesis of DDD involve mutations that have been shown to produce haploinsufficiency of the keratin-5 gene (KRT5) on chromosome12q.3 Keratin-5 is an essential element of the basal keratinocyte cytoskeleton, together with keratin-14. Keratin-5 dysfunction leads to alterations in organelle transport and in epidermal differentiation. In addition, a study in 2013 identified a mutation in chromosome20 in a family with generalized DDD.4 The heterozygous deletion of gene POFUT1 leads to decreased expression of keratin5 and other proteins (Notch1-2, Hes1) in keratinocytes.
DDD has been associated with certain skin diseases, in particular multiple keratoacanthomas,5 epidermoid cysts,5 and squamous cell carcinoma.6 An important association is with HS, as found in our patient, though few cases have been reported in the literature.1,2,5,7–9 HS is a multifactorial disease that most commonly affects young people and is characterized by recurrent skin-fold abscesses and fistulas that leave scars. One etiologic and pathogenic factor that has been observed is a defect of epithelial proliferation in the external sheath, leading to follicular occlusion, described as a possible common origin for all these disorders.5,7,9
DDD must be differentiated from other genodermatoses with reticular pigmentation2,3: Galli-Galli disease,10 reticulate acropigmentation of Kitamura, Haber syndrome, and reticulate acropigmentation of Dohi. It has recently been agreed that all these reticular pigmentary diseases are variants of a single entity.5 Other important diseases in the differential diagnosis include acanthosis nigricans, Naegeli-Franceschetti-Jadassohn syndrome, and confluent and reticulate papillomatosis (Gougerot-Carteaud syndrome).
There is no completely effective treatment for DDD. Topical hydroquinone, retinoids, and corticosteroids, oral isotretinoin, and some lasers have been used with variable results. Topical adapalene and tazarotene have been the most successful of the treatments used. This derives from their anti-inflammatory properties as well as their modulating action on gene expression and on keratinocyte differentiation and proliferation. Several types of laser, in particular carbon dioxide and erbium-doped yttrium aluminium garnet (Er:YAG) lasers, have been shown to be useful in reducing or eliminating the hyperpigmentation.
In conclusion, we have presented a case of DDD associated with HS, a previously reported but rare association. The lesions are progressive and recurrent. Topical and oral retinoids are a safe and accessible treatment option, though not particularly effective. It is important to maintain long-term follow-up in these patients due to the possible association with skin tumors.
Please cite this article as: Arjona-Aguilera C, Linares-Barrios M, Albarrán-Planelles C, Jiménez-Gallo D. Enfermedad de Dowling-Degos: caso clínico asociado a hidradenitis supurativa. Actas Dermosifiliogr. 2015;106:337–338.