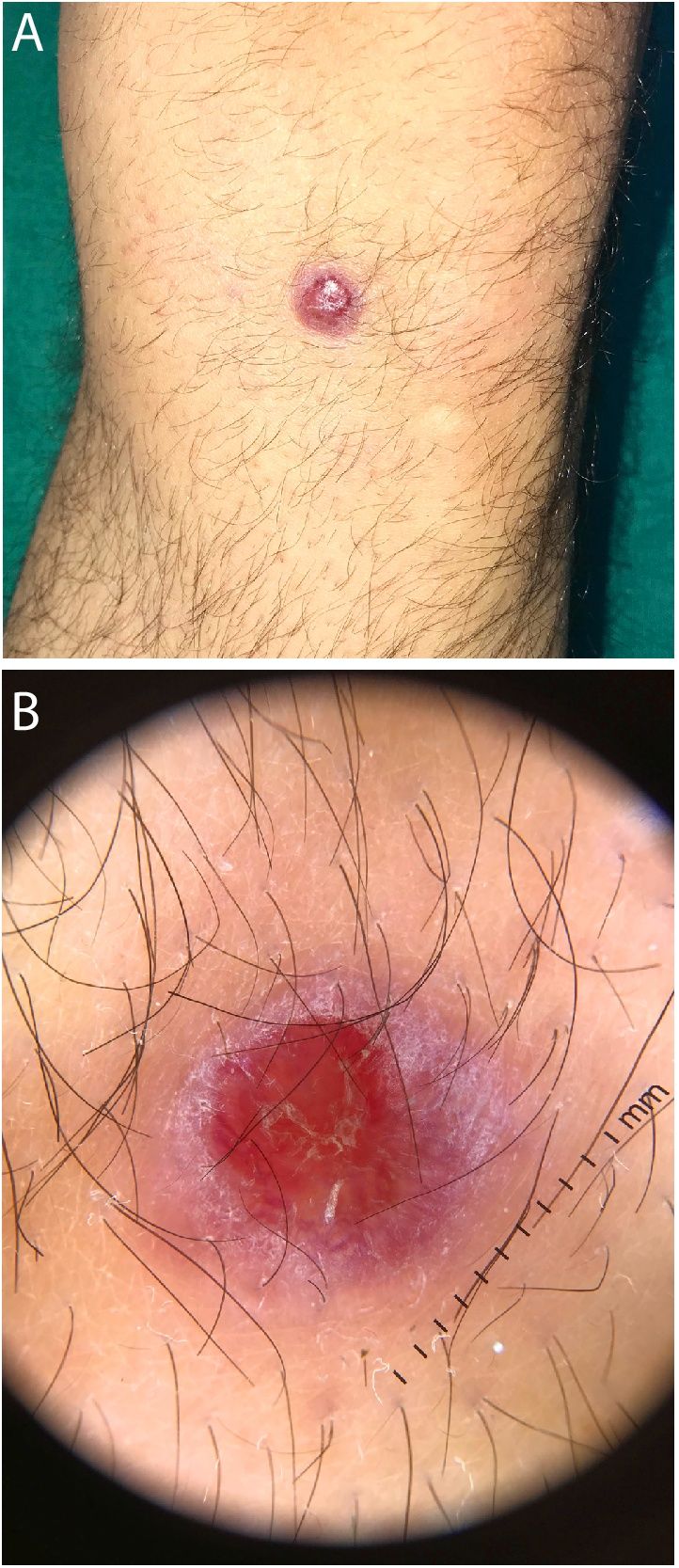
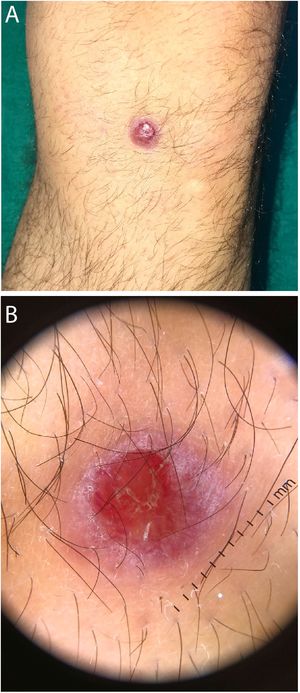
A 29-year-old man visited our department with an asymptomatic lesion located on the left knee. The lesion had appeared a year earlier and had grown slowly and gradually. The patient did not recall having suffered any trauma to the area. Examination revealed a violaceous round lesion with a shiny appearance measuring 1 cm. The lesion presented minimal erosion in the central portion and some peripheral desquamation. It was indurate on palpation but not adhered to the deep layers (Fig. 1A). Dermatoscopy revealed no criteria for a melanocytic lesion but did show vessels with a crown distribution and central erosion with yellowish scales (Fig. 1B). The lesion was excised with a margin of 1 cm of surrounding healthy skin.
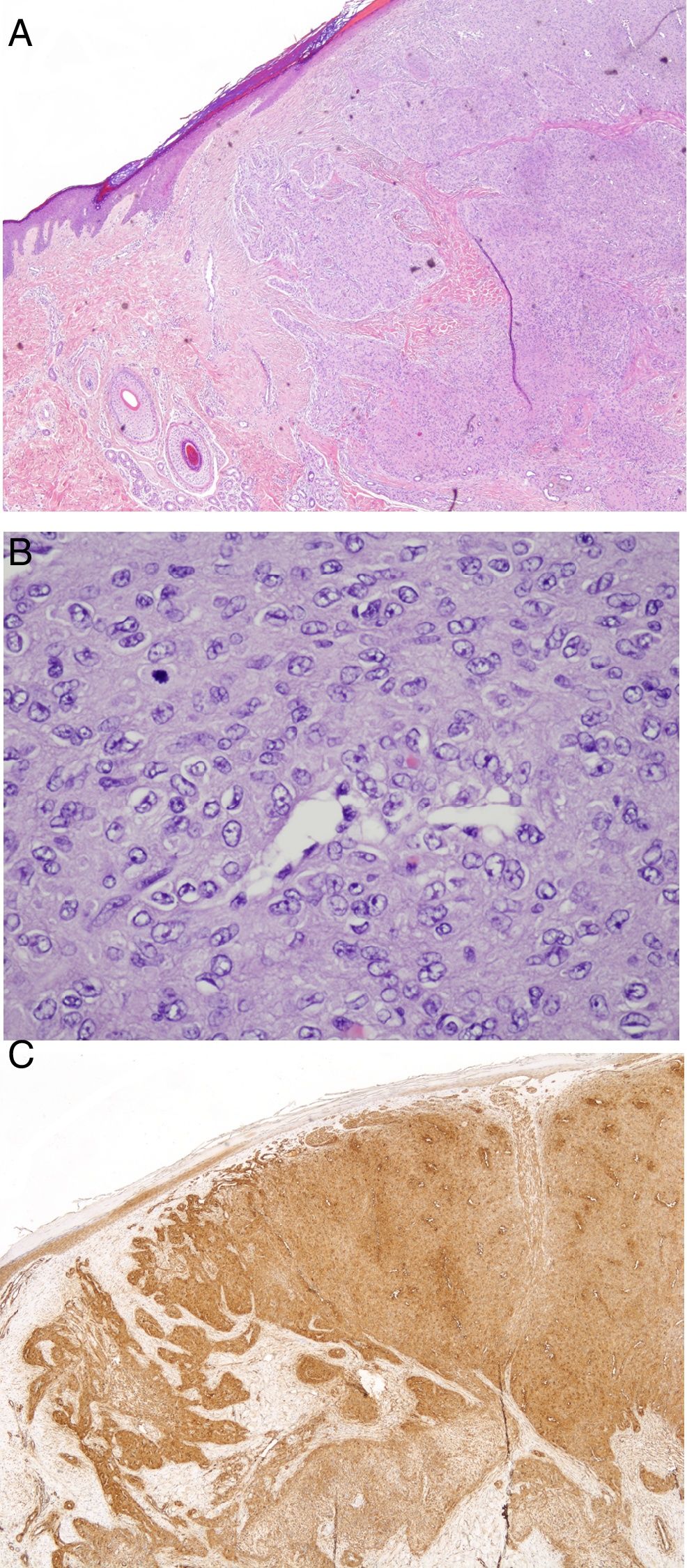
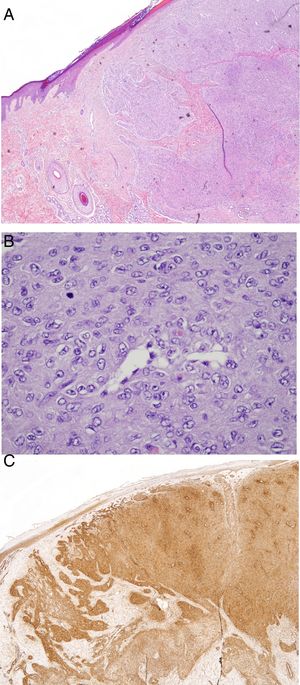
Pathology revealed a dermal tumor lesion with a diameter of 9 mm, composed of oval cells organized in a concentric distribution around the small-caliber vessels (Fig. 2A and B). The lesion presented a pattern of expansive growth, without necrosis or cell pleomorphism, but with high mitotic activity (46 mitosis/50 high-magnification fields; proliferative index [Ki-67], 5%). Immune staining was positive for smooth-muscle actin (Fig. 2C) and specific muscle, caldesmon, vimentin, and collagen IV, and negative for CD31, CD34, S100 protein, and AE1/AE3. Abnormal expression of INI-1 was not found.
Six months after excision, the patient continued without clinical signs of local recurrence.
What is the diagnosis?
DiagnosisMyopericytoma.
CommentsMyopericytoma, formerly known as adult cutaneous myofibroma, is a mesenchymal tumor that derives from the perivascular myoid cells, the muscle cells that surround the blood vessels.1 It is considered to be a benign, slow-growing tumor. It typically presents in adult males as a solitary lesion measuring less than 2 cm. It affects the dermis and subcutaneous cell tissue in the form of painless nodules, most frequently on the lower extremities.2,3 In patients with HIV infection, the location tends to be atypical (tongue, vocal cords, liver, brain) and is often multifocal. Onset may be preceded by trauma.3,4
Diagnosis is histologic and imaging tests (ultrasound, CT, NMRI) show poor sensitivity.3
The entity is made up of oval or fusiform eosinophils of myoid appearance that present a concentric perivascular growth pattern (in the form of a sleeve) around vessels of varying size.3 Features suggesting a poorer prognosis include infiltration of the subcutaneous cellular tissue, atypia, mitosis, necrosis, and nuclear pleomorphism.5 The entity is characteristically positive for smooth-muscle actin, specific-muscle actin, vimentin, and caldesmon, and negative for CD34 (endothelial cells) and desmin.2–4
Its characteristics require a differential diagnosis with the following tumors: glomic tumor (perivascular cuboid epithelioid cells with no concentric pattern), angioleiomyoma (deeper lesions, muscle walls thickened with fibrosis, positive for desmin), solitary myoma (biphasic growth pattern), angiomyolipoma (positive for S100), and hemangiopericytoma (staghorn vascular pattern, positive for CD34).1
Treatment consists of broad surgical resection, although no guidelines exist that indicate the necessary margin width. Given the benign course of the disease, prognosis is good. Local recurrence is rare if the resection is complete and cases of metastasis are exceptional.3,6
We report the case of a 29-year-old man with a myopericytoma on the left knee, which is atypical due to its mitotically active nature. It is important to follow up these patients because, despite the good prognosis of this entity, characteristics such as infiltration of the subcutaneous cellular tissue, atypia, mitosis, necrosis, or nuclear pleomorphism increase the risk of recurrence.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: García Castro R, Dominguez Luis F, Santos-Briz Terrón A. Miopericitoma mitóticamente activo. Actas Dermosifiliogr. 2021;112:59–60.