Generalized lichen planus (GLP) can be difficult to treat. One alternative for patients who do not respond to common topical and systemic treatments, such as corticosteroids and oral antihistamines, is phototherapy. Narrowband UV-B phototherapy offers several advantages and is currently the main treatment modality. In this study, we present the results corresponding to 10 patients with generalized lichen planus treated with narrowband UV-B phototherapy. We performed a prospective study of adult patients with generalized lichen planus affecting more than 20% of their body surface area. A complete response was observed in 8 patients (80%) and the disease recurred in 2 of these (recurrence rate, 25%). These rates are similar to those reported in the literature reviewed. Narrowband UV-B phototherapy is a widely used alternative to systemic treatments in GLP, but there are very few reports of its results in the literature.
El liquen plano en su forma generalizada (LPG) es en ocasiones difícil de tratar. Cuando fallan los tratamientos tópicos y sistémicos más utilizados como corticoides y antihistamínicos orales la fototerapia se plantea como alternativa. En el momento actual y dadas sus ventajas se utiliza con más frecuencia el ultravioleta B de banda estrecha (UVB-BE). En este trabajo presentamos los resultados en 10 pacientes con LPG tratados con UVB-BE. Para ello realizamos un estudio prospectivo en el que se incluyeron pacientes adultos afectados de LPG en más del 20% de su superficie corporal. Se obtuvo respuesta completa en 8 de los pacientes (80%) con una tasa de recidiva del 25% (2/8). Estos resultados son similares a la literatura revisada. La fototerapia con UVB-BE es ampliamente utilizada como alternativa a los tratamientos sistémicos en el LPG, sin embargo, existen pocos estudios publicados en la literatura sobre sus resultados.
Lichen planus (LP) is a dermatosis of unknown cause that affects between 0.2% and 1% of the population.1 Due to its aesthetic effects and the intense pruritus it causes, disseminated or generalized LP (GLP) requires rapid treatment. The only published guidelines for GLP treatment consider phototherapy (narrowband ultraviolet B [UV-B] and psoralen and ultraviolet A [PUVA] therapies) the treatment of choice for patients that do not respond to topical treatments. The first level of proposed second-line therapies includes the following treatment options: retinoids combined with phototherapy (Re-UV-B, Re-PUVA); methotrexate; systemic corticosteroids; hydroxychloroquine; and dapsone. Proposed second-level therapies include azathioprine, cyclosporine, and mycophenolate.2 We present the results of a series of GLP patients treated with narrowband UV-B phototherapy, compare our findings with those of other authors, and discuss alternative treatment options.
Patients and MethodsA prospective study was carried out between May 2011 and April 2017. Patients eligible for inclusion were adults with GLP diagnosed by biopsy and involvement of >20% of their body surface area (BSA) who had previously failed to respond to an appropriate regimen of oral corticosteroids (0.5–1 mg/kg for at least 3 weeks). All patients provided written informed consent prior to treatment.
Patients were treated with a Waldmann UV7002 phototherapy system (Villingen-Schwenningen, Germany) with an emission range of 310–315 nm and a maximum radiation level of 311 nm. Each patient underwent 3 weekly sessions until improvement was observed. Doses were determined following a phototype protocol.3,4 The only concomitant treatments were topical corticosteroids, oral antihistamines, and emollients. Data on patient age, sex, and affected BSA were collected prior to treatment using Psoriasis Calc, a mobile phone application. Treatment response was classified as follows: complete response (CR), >90% lesion clearance; partial response (PR), 70%–90% clearance; incomplete response (IR), <70% clearance. Patients subsequently underwent periodic check-ups to assess recurrence. The appearance of new lesions was considered a recurrence.
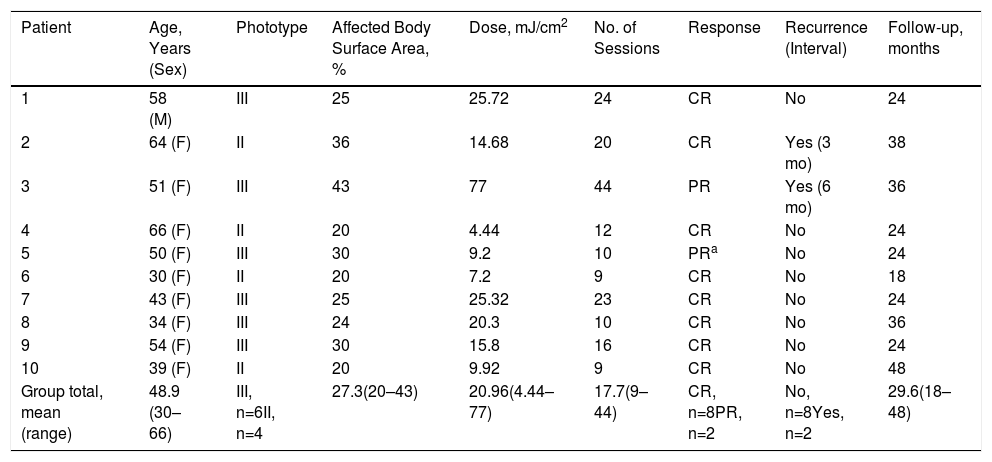
ResultsThe study population consisted of 10 patients (9 women and 1 man) with a mean age of 48.9 years (range, 30–66 years) (Table 1). Most were classified as phototype III. The mean BSA on beginning treatment was 27.3% (range, 20%–43%). Patients underwent a mean of 17.7 sessions (range, 9–44) and received a mean dose of 20.96J/cm2 (range, 4.44–77.00 J/cm2). Eight patients achieved CR and the remaining 2 achieved PR. One of the patients who achieved PR discontinued treatment, but nonetheless continued to improve without recurrences.
Patient Characteristics and Treatment Outcomes
| Patient | Age, Years (Sex) | Phototype | Affected Body Surface Area, % | Dose, mJ/cm2 | No. of Sessions | Response | Recurrence (Interval) | Follow-up, months |
|---|---|---|---|---|---|---|---|---|
| 1 | 58 (M) | III | 25 | 25.72 | 24 | CR | No | 24 |
| 2 | 64 (F) | II | 36 | 14.68 | 20 | CR | Yes (3 mo) | 38 |
| 3 | 51 (F) | III | 43 | 77 | 44 | PR | Yes (6 mo) | 36 |
| 4 | 66 (F) | II | 20 | 4.44 | 12 | CR | No | 24 |
| 5 | 50 (F) | III | 30 | 9.2 | 10 | PRa | No | 24 |
| 6 | 30 (F) | II | 20 | 7.2 | 9 | CR | No | 18 |
| 7 | 43 (F) | III | 25 | 25.32 | 23 | CR | No | 24 |
| 8 | 34 (F) | III | 24 | 20.3 | 10 | CR | No | 36 |
| 9 | 54 (F) | III | 30 | 15.8 | 16 | CR | No | 24 |
| 10 | 39 (F) | II | 20 | 9.92 | 9 | CR | No | 48 |
| Group total, mean (range) | 48.9 (30–66) | III, n=6II, n=4 | 27.3(20–43) | 20.96(4.44–77) | 17.7(9–44) | CR, n=8PR, n=2 | No, n=8Yes, n=2 | 29.6(18–48) |
Abbreviations: CR, complete response; PR, partial response.
None of the patients had diseases associated with LP. The entire integument was affected in all cases, except for one patient in whom involvement was limited to the trunk and arms. All patients reported onset of dermatosis during the preceding 6 months, except for Patient 3, who had experienced recurrent outbreaks over 9 years. Surprisingly, this patient required many more phototherapy sessions than the others in order to achieve CR. No major adverse effects were observed. Most patients experienced occasional itching or erythema that did not require discontinuation of treatment.
DiscussionAlthough considered the first line of treatment by some authors, there are few reports describing the use of phototherapy to treat GLP.2 Narrowband UV-B phototherapy offers certain advantages over PUVA phototherapy: patients do not require pretreatment with oxsoralen, which is sometimes contraindicated, nor do they remain photosensitized for several hours after treatment. Both modalities offer similar good outcomes.3,4 However, the use of narrowband UV-B phototherapy has increased in recent years owing to its greater ease of administration. The mechanism of action of narrowband UV-B phototherapy in GLP is unknown.1,2
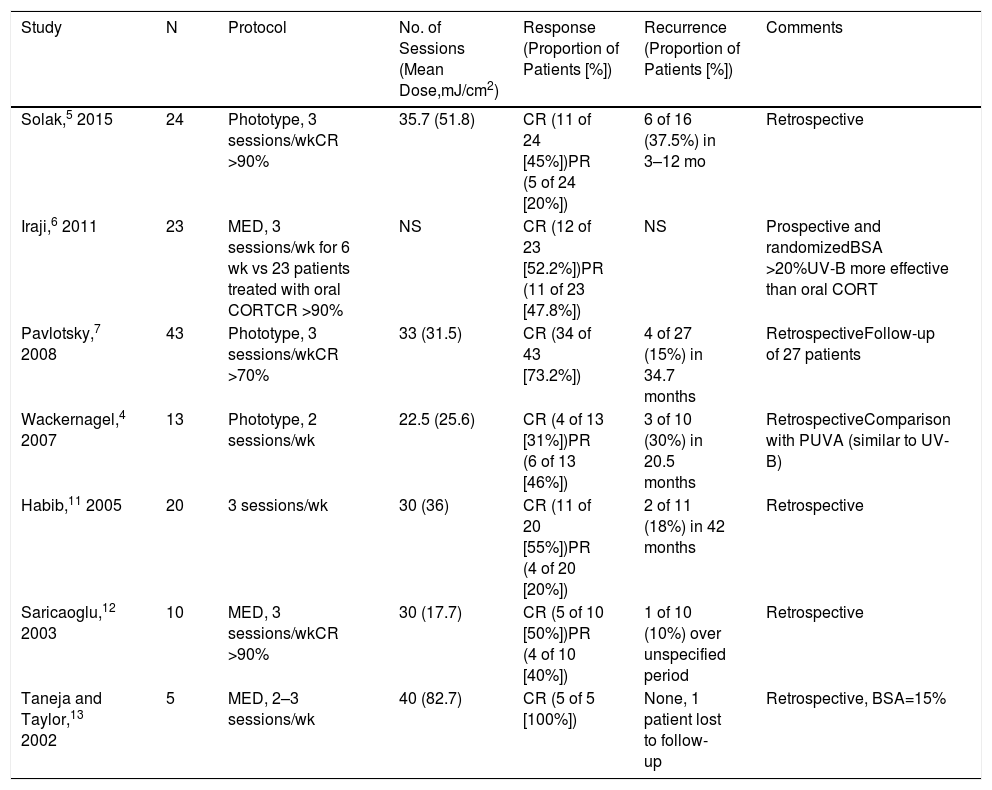
Due to the scarcity of articles on GLP treatment it is difficult to compare the efficacy of currently available therapies. In normal clinical practice, and in several published research studies,5–7 systemic corticosteroids are the most commonly used treatment in patients that do not respond to topical treatments or present with generalized GLP. Despite the availability of phototherapy, all of our patients had received at least one cycle of oral corticosteroid treatment. Remission rates of up to 83% have been reported in GLP patients that received corticosteroid therapy, which is a more comfortable and traditional form of treatment.8 While the efficacy of corticosteroids is indisputable, it has not been demonstrated in clinical trials, and supporting evidence is limited.2 A randomized clinical trial conducted by Iraji and coworkers6 compared the efficacy of oral corticosteroids (n=23) with that of narrowband UV-B phototherapy (n=23) in patients with GLP (Table 2). Despite the longer than usual corticosteroid treatment period (0.3 mg/kg for 6 weeks), the authors concluded that UV-B phototherapy was more effective. Evidence supports the use of acitretin as an alternative treatment option for GLP. Acitretin is recommended based mainly on the results of a randomized study of 28 patients treated with a dose of 30 mg/day9: 64% of patients responded favorably, although papules persisted in most patients. Acitretin is contraindicated in patients with hyperlipidemia or liver disease and in women of childbearing age. Moreover, its use entails periodic testing not required in patients treated with oral corticosteroids or narrowband UV-B phototherapy.
Summary of Published Studies on the Treatment of Generalized Lichen Planus with Narrowband Ultraviolet B Phototherapy
| Study | N | Protocol | No. of Sessions (Mean Dose,mJ/cm2) | Response (Proportion of Patients [%]) | Recurrence (Proportion of Patients [%]) | Comments |
|---|---|---|---|---|---|---|
| Solak,5 2015 | 24 | Phototype, 3 sessions/wkCR >90% | 35.7 (51.8) | CR (11 of 24 [45%])PR (5 of 24 [20%]) | 6 of 16 (37.5%) in 3–12 mo | Retrospective |
| Iraji,6 2011 | 23 | MED, 3 sessions/wk for 6 wk vs 23 patients treated with oral CORTCR >90% | NS | CR (12 of 23 [52.2%])PR (11 of 23 [47.8%]) | NS | Prospective and randomizedBSA >20%UV-B more effective than oral CORT |
| Pavlotsky,7 2008 | 43 | Phototype, 3 sessions/wkCR >70% | 33 (31.5) | CR (34 of 43 [73.2%]) | 4 of 27 (15%) in 34.7 months | RetrospectiveFollow-up of 27 patients |
| Wackernagel,4 2007 | 13 | Phototype, 2 sessions/wk | 22.5 (25.6) | CR (4 of 13 [31%])PR (6 of 13 [46%]) | 3 of 10 (30%) in 20.5 months | RetrospectiveComparison with PUVA (similar to UV-B) |
| Habib,11 2005 | 20 | 3 sessions/wk | 30 (36) | CR (11 of 20 [55%])PR (4 of 20 [20%]) | 2 of 11 (18%) in 42 months | Retrospective |
| Saricaoglu,12 2003 | 10 | MED, 3 sessions/wkCR >90% | 30 (17.7) | CR (5 of 10 [50%])PR (4 of 10 [40%]) | 1 of 10 (10%) over unspecified period | Retrospective |
| Taneja and Taylor,13 2002 | 5 | MED, 2–3 sessions/wk | 40 (82.7) | CR (5 of 5 [100%]) | None, 1 patient lost to follow-up | Retrospective, BSA=15% |
Abbreviations: BSA, body surface area; CORT, corticoid; CR, complete response; MED, mean erythematous dose; NS, not specified; PR, partial response; UV-B, narrowband ultraviolet B phototherapy.
Our study population had GLP with extensive involvement (mean BSA, 27.3%). A mean dose of 20.93 mJ/cm2 and a mean number of 17 sessions were required to achieve a response, which was complete in 8 (80%) patients and partial in 2 (20%). These findings are in line with those of previous studies4–7,10–13 in which CR was achieved in 31% to 100% of patients and PR in 20% to 47.8% of patients. However, closer reading of the published studies (Table 2) reveals considerable variation in both the dose administered (mean, 20–40 J/cm2) and the response rate (31%–100%), indicating a lack of uniformity. This variability, which may be due to the absence of established protocols or clinical variability among the patients studied, makes it difficult to draw conclusions. In our patient group, the mean dose required for lesion clearance was 20.93 J/cm2, which is lower than the corresponding dose reported for moderate psoriasis14 and closer to that reported for guttate psoriasis,15 a clinical form that resembles GLP and is characterized by the presence of disseminated papules. While some patients responded to accumulated doses of approximately 10 mJ/cm2, it is unlikely that this can be attributed to spontaneous improvement of GLP: 17 sessions correspond to approximately 1.5 months of treatment, and spontaneous improvement of GLP requires approximately 15 months.4
Recurrence rates reported in the literature (10%–37.5%) are somewhat more homogeneous, and in line with those observed in the present study (20%). Recurrences tended to occur between 3 and 6 months after treatment. To date, no predictors of medium-term response have been described for UV-B phototherapy in GLP patients.5–7 However, response rates are significantly higher than those reported for other treatment options2,6 and similar to those described for phototherapy in patients with other dermatoses.14
In our group of GLP patients narrowband UV-B phototherapy produced a good response and was well tolerated. Nonetheless, evidence supporting treatment of GLP with narrowband UV-B phototherapy, and other treatment modalities, is limited to a handful of studies with small groups of patients. While it is difficult to develop a treatment protocol for GLP, narrowband UV-B phototherapy is among the first-choice treatment options. More studies of this uncommon dermatosis will be required in order to draw reliable conclusions.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Fernández-Guarino M, Aboín S, Barchino L, Arsuaga C, Lázaro Ochaita P. Liquen plano generalizado tratado con ultravioleta B de banda estrecha: resultados en 10 pacientes y revisión de la literatura. Actas Dermosifiliogr. 2019;110:490–493.