A 71-year-old Colombian man presented to our dermatology service, in Cali, Colombia, with a history of 3-weeks of intermittent fever and painful progressive skin ulcers located on upper and lower limbs. Without any other relevant clinical information.
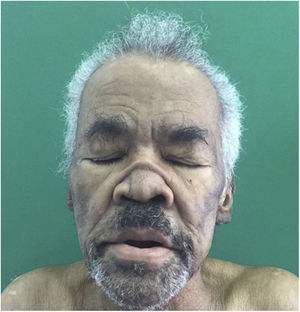
Physical ExaminationPhysical examination revealed a “saddle” nose, madarosis, pinna edema (Fig. 1), and extensive ulcers withnecrotic aspect and reticular pattern in all extremities (Fig. 2). Neurologic exam revealed a left foot drop, with polyneuritis.
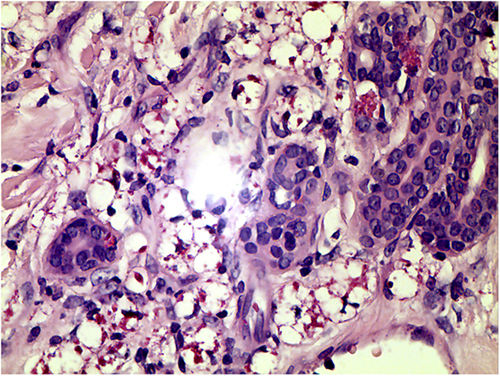
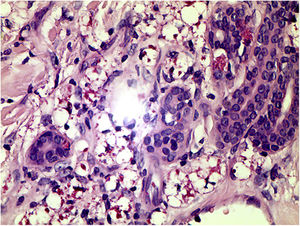
HistophatologySkin biopsy showed granulomas with small-vessel vasculitis and Fite-Faraco stain revealed in the nerve fillets and vessels the presence of numerous acid-fast bacilli (AFB) (Fig. 3)
Additional TestsSlit-skin smear examination (earlobe, elbows and nose) was positive for AFB, bacterial index (BI): 2.5.
What Is Your Diagnosis?DiagnosisLucio's phenomenon
Clinical Course And TreatmentThe patient was treated with multibacillary multidrug therapy (MDT/MB: Rifampicin, Clofazimine, Dapsone), and corticosteroids 8-week with improvement of the lesions
with persistent neurological deficit.
DiscussionLeprosy or Hansen's disease is a chronic and debilitating infectious disease caused by Mycobacterium leprae; In the world the prevalence of leprosy has declined considerably since the introduction of multidrug therapy in 1982, in Colombia there are reported about 400 new cases per year.1 The clinical expression of the disease depends on the host's immune response.2
LP is a rare and severe leprosy reactional episode in patients with diffuse lepromatous leprosy. Is characterized by the presence of painful erythematous macules that evolve to ulcers which heal leaving pearly scars, may be accompanied by polyneuritis, arthralgia and systemic compromise, constituting an medical emergency.3
In our patient, the histopathologic findings showed mainly vasodilatation and thickening of the wall vessels of the superficial and deep plexus of the dermis, proliferation of endothelial cells and occasionally intraluminal clots leading to dermoepidermal necrosis. The Fite-Faroco stain was positive for the present of bacilli inside the vessels and around and in the endothelium of the wall vessels.
Other fidings that had been described are small and medium-sized arteries vasculitis, with their walls involved by clusters of globi, distortion of the structure of the vessel wall, narrowing, and obliteration of their lumen.4 LP is a distinctive type of granulomatous and necrotizing panvasculitis; the involved vessels are mostly medium- sized arteries, their occlusion leads to ischemic necrosis of the whole skin, with detachment of the epidermis.4
Micobacterium leprae was considered the only infectious agent causing leprosy, however a report of two cases of Mexican patients with LP in which the etiological agent was sequenced, revealed a variability of approximately 7.4% in comparison with M. Leprae reference genome, informing a new species, M. lepromatosis This finding have been confirmed in later genetic studies.5
Within the differential diagnosis, it is important to take into account the catastrophic manifestations of autoimmune diseases such as the antiphospholipid syndrome and systemic vasculitis, which can occur with cutaneous ulcers.3 There is no standard treatment for LP, and a therapy based-on corticosteroids to modulate the immune response was used, as in other immunologic reactions leprosy: type 1 reaction (reversal reaction) and ocasionally in type 2 reaction (erythema nodosum leprosum).6
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Castillo-Loaiza S, Díaz CJ, Cardenas LF. Úlceras progresivas localizadas en las extremidades. Actas Dermosifiliogr. 2019;110:495–496.