Cutis laxa is a congenital or acquired connective tissue disorder characterized by extracellular matrix and elastic fiber defects. It manifests clinically as sagging skin, giving an appearance of premature aging. Blepharochalasis is an acquired form of cutis laxa that affects the periorbital region. It normally starts in childhood or adolescence and is characterized by recurrent episodes of painless eyelid swelling. Repeated acute attacks lead to elastin fiber degradation and sagging skin in the periorbital region that can interfere with vision. The pathogenesis of blepharochalasis or blepharoptosis is still unclear, although a role has been proposed for immunopathogenic mechanisms that result in elastin fiber degradation.1,2 Grassegger et al.1 and Schaeppi et al.2 reported immunoglobulin A (IgA) deposits around blood vessels and sweat glands and in the papillary dermis. The second group of authors also found IgA deposits in elastic fibers around hair follicles. Histopathology shows disperse fragmented, granular elastic fibres in the reticular dermis.
The differential diagnosis in blepharochalasis should include inflammatory diseases (contact dermatitis, angioedema, blepharitis, and hereditary angioedema), tumors (retrobulbar tumor or lacrimal gland tumor/cyst), systemic diseases (thyroid and kidney disease), other extracellular matrix diseases (Ehlers-Danlos syndrome, elastic pseudoxanthoma, mid-dermal elastolysis, anetodermia, and postinflammatory elastolysis), and even physiologic aging. The condition can also form part of syndromes, such as Ascher syndrome, which is characterized by blepharochalasis, double lip, and nontoxic goiter.
The treatment for blepharochalasis is reconstructive surgery with cosmetic and therapeutic intent, but recurrence is common.3
In this article, we describe the case of a young man with blepharochalasis as a clinical presentation of acquired cutis laxa.
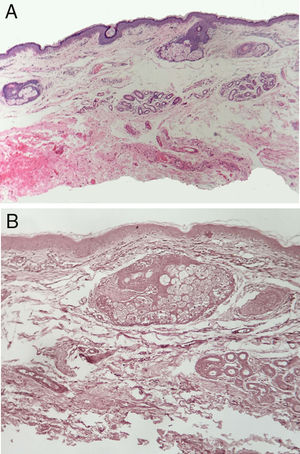
A 24-year-old man presented with looseness of the upper eyelids that had become progressively worse over 8 years. The sagging was such that it had caused considerable cosmetic damage. The patient reported that he had experienced several episodes of eyelid swelling over a period of more than 2 years before his eyelids began to sag. He had not received any treatment and reported no other problems. Skin examination showed loose skin on both upper eyelids (more pronounced on the right) and partial occlusion of the eyelashes. The skin in the upper eyelid region was atrophic and had a violaceous color (Fig. 1). Vision was not affected by the blepharoptis. The patient confirmed that the condition had not been treated medically. Biopsy of the eyelids (with hematoxylin-eosin staining) showed just slight swelling of the upper dermis. Orcein staining showed absence of elastic fibers (Fig. 2). IgA was positive in the dermal vessel walls. Computed tomography of the orbits, a chest X-ray, and laboratory tests were all normal. The patient underwent upper blepharoplasty (Fig. 3) and the cosmetic and functional results during follow-up were excellent. He reported that his field of vision had improved, particularly the upper field as his eyes were no longer covered by the sagging eyelids.
Blepharochalasis is an uncommon clinical presentation of cutis laxa characterized by painless episodes of bilateral edema.4 The condition is generally self-limiting and does not respond to antihistamines or corticosteroids. During the quiescent stage of disease and following several acute attacks, it progresses to cause bilateral loss of periorbital skin.5 There may be violaceous coloring on the upper eyelids.6 In our patient, this coloring led to consideration of dermatomyositis in the differential diagnosis.
The pathophysiology of blepharochalasis remains elusive. Inflammatory episodes are believed to give rise to elastic fiber degradation due to elastolysis triggered by increased elastase activity or impaired elastase inhibitor function.3 Systemic manifestations have not been observed in the vast majority of cases.7 In line with previously described findings, IgA deposits, which probably have a pathogenic role, were observed in the blood vessel walls.1
Proposed triggers include stress, fever, and upper respiratory tract infections, among others.3 A more specific immune mechanism associated with elastin and collagen degradation by metalloproteases may also be involved .1
The recommended treatment is blepharoplasty with cosmetic or therapeutic intent. Ideally, surgery should be performed during the quiescent disease stage.8 Unlike most connective tissue diseases, cutis laxa does not usually interfere with postoperative recovery.9 Patient follow-up is necessary, however, given the risk of recurrence.10
Blepharochalasis must be contemplated in the differential diagnosis of skin disorders that affect the periorbital region. Correct diagnosis is important for ensuring adequate treatment and follow-up.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Dantas SG, Trope BM, de Magalhães TC, Azulay DR, Quintella DC, Ramos-e-Silva M. Blefarocalasia: una presentación rara de cutis laxo. Actas Dermosifiliogr. 2019;110:327–329.