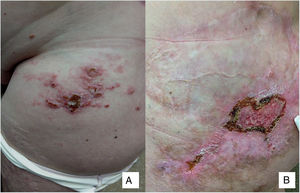
A 58-year-old woman was referred to the Oncology Department for skin lesions with a metameric distribution on the left thigh and groin. The lesions had first appeared 3 months earlier and, in her opinion, were initially similar to herpes zoster. For the previous 3 years, the patient had been in follow-up because of eccrine porocarcinoma. Physical examination revealed confluent erythematous nodules and papules on the groin and anterior aspect of the left thigh (Fig. 1A and B).
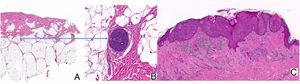
Histopathology confirmed the presumptive clinical diagnosis of cutaneous metastasis of eccrine porocarcinoma. Abundant cellular atypia was observed, as were desmoplastic stroma and large tumor nests composed of epidermal cells that invaded the papillary and reticular dermis and, focally, the hypodermis, leaving areas of central necrosis and forming ducts with eccrine differentiation (Fig. 2A). Similarly, we observed abundant foci of lymphatic invasion (Fig. 2B) and numerous areas with epidermotropism (Fig. 2C). The extension study, which was based on positron emission tomography-computed tomography, revealed the presence of hypermetabolic foci and enlarged para-aortic lymph nodes in the left common iliac region and external region and right groin.
A, Hematoxylin-eosin, original magnification, ×2. Tumor nests in the epidermis invading the papillary and reticular dermis and, focally, the hypodermis. B, Hematoxylin-eosin, original magnification, ×20. Note the lymphatic vessel with metastasis in the hypodermis. C, Hematoxylin-eosin, original magnification, ×15. Nests of tumor cells infiltrating the epidermis.
Assessment of the previous clinical history revealed that the patient had undergone conventional surgery twice with safety margins of 2 cm and surgical margins that were histologically free of neoplasm. However, the lesions had recurred, together with metastatic enlarged inguinal lymph nodes; therefore, she underwent a third procedure with Mohs surgery (free margins) and inguinal lymphadenectomy (metastasis in 6 of 12 nodes isolated). Furthermore, she had received palliative radiotherapy, as well as various cycles of chemotherapy with docetaxel 75 mg/m2, then with paclitaxel 175 mg/m2, and finally with capecitabine 1250 mg/m2; the first 2 were suspended owing to lack of efficacy, and the third, which was the most effective, was suspended owing to digestive intolerance.
After histological confirmation of the new recurrence, the Medical Oncology Department decided to restart capecitabine at 1000 mg/m2. This was well tolerated and enabled a progression-free interval of only 4 months. The result of massive sequencing of BRAF, epidermal growth factor receptor, and hormone receptors for evaluation of potential therapeutic targets was negative. Therefore, treatment was started with doxorubicin 50 mg/m2, leading to a partial initial response in the skin and lymph nodes. Disease progressed once again after 8 cycles of treatment, with the appearance of skin lesions that extended to the abdomen, vulva, and right thigh. Positron emission tomography-computed tomography revealed lesions in the retroperitoneal and axillary regions. At the time of the last check-up, the patient was receiving treatment in the Palliative Care and Pain Unit.
Eccrine porocarcinoma is an uncommon malignant tumor (0.005%-0.01%)1 that originates in the acrosyringium of the eccrine sweat glands. It is more common in elderly persons, with a higher incidence in men,2,3 and predominantly affects the lower limbs, head, and neck.3–5 It usually appears de novo or, in 18% of cases, from an eccrine poroma.4,6
Prognosis is based on histopathology. The differential diagnosis is with squamous cell carcinoma based on immunohistochemical markers, mainly carcinoembryonic antigen (+), epithelial membrane antigen (+), and cytokeratin 19 (+).7 The infiltrative growth pattern and the pagetoid pattern indicate an increased risk of locoregional recurrence,4 as reported in the present case.
The zosteriform or metameric distribution has received little attention,6 and the lesions in the case published mimicked those of seborrheic keratosis.
Tumor cells invade the epidermis owing to their epidermotropic character, although they also invade the deep dermis and hypodermis, thus favoring dissemination to the lymphatic system and bloodstream.8 The presence of more than 14 mitoses per field, lymphovascular invasion, and/or tumor thickness > 7 mm are associated with a greater risk of metastasis.4 The risk of locoregional recurrence is 20%, and this is associated with a mortality rate of 65%.4 Distant metastasis (lung, bone marrow, bone, and muscle) is less frequent, although in this case mortality is as high as 80%.3
Gómez-Zubiaur et al2 proposed an interesting therapeutic algorithm. If there is a high risk of locoregional recurrence after initial removal of the lesion via conventional surgery, Mohs surgery is recommended. However, if a risk factor for metastasis is present, then it is recommended to perform a selective sentinel node biopsy and then to decide on appropriate action based on the results. Prophylactic lymphadenectomy is controversial. Mohs surgery has only exceptionally proven insufficient for disease control, as previously published9 and as observed in the present case.
Treatment of metastatic disease requires a multidisciplinary approach. Various cycles of chemotherapy based on taxanes and carboplatin combined with epirubicin, docetaxel, or paclitaxel and interferon a have proven relatively successful. Electrochemotherapy is also worthy of evaluation.10
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We are grateful to the pathologist Dr. José Aneiros Fernández from Hospital Universitario San Cecilio, Granada, Spain for his contribution to the present case report.
Please cite this article as: Cuenca-Barrales C, Navarro-Triviño FJ, Espadafor-López B, Arias-Santiago SA, Ruiz-Vilaverde R. Metástasis zosteriformes de porocarcinoma ecrino. Actas Dermosifiliogr. 2020;111:276–278.