Mammillary fistula, or Zuska disease, was first described in 19511 as the appearance of small, painful inflammatory nodules in the area of the areola that generally progress to recurrent abscesses, sinuses, and fistulas. Atkins2 subsequently coined the term mammillary fistula to refer to this entity, which accounts for 1%-2% of all symptomatic mammary conditions. Mammillary fistula is difficult to treat, is associated with long-term morbidity, and has a considerable impact on patient quality of life.3
A 23-year-old woman (smoker) was being followed at the Breast Pathology Unit (BPU) of our hospital for recurrent flares of mastitis affecting the left breast that had first appeared 9 months previously. The clinical response to several cycles of oral antibiotics was favorable, although the inflammatory symptoms reappeared, with disabling pain, inflammatory changes, and suppuration a few weeks after each cycle. Consequently, she had consulted on at least 10 occasions at the BPU and the emergency department, as well as with her primary care physician. Before a wedge resection of the milk ducts was performed, the BPU referred the patient for a dermatologic assessment.
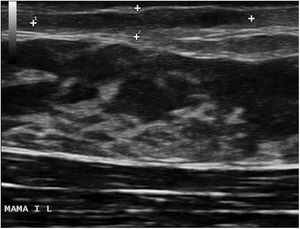
The physical examination revealed an elongated and erythematous indurated area in the area of the areola of the left breast that was painful to touch (Fig. 1). Ultrasound revealed a longitudinal hypoechoic band-like image (15 × 2.4 × 6 mm) in the superficial dermis (Doppler negative) compatible with a fistulous tract (Fig. 2). Based on these findings, the patient was diagnosed with mammillary fistula and prescribed treatment with intralesional triamcinolone, which led to clinical and ultrasound resolution of the lesion. No recurrences were observed during the following 6 months (Fig. 3).
For many years, mammillary fistula was thought to result from obstruction of a distal milk duct by squamous metaplasia, with keratinization and/or epidermalization of the duct. However, it was recently proposed that mammillary fistula originates in a hair follicle, where the initial event is occlusion of the follicle because of hyperkeratinization. This leads to dilatation and rupture of the duct, with release of secretions into the subcutaneous cell tissue and, therefore, an inflammatory reaction, secondary bacterial infection, and, finally, formation of abscesses with drainage of sinus tracts and fistulas in the area of the areola.3 In this case, the squamous metaplasia identified in the biopsy specimens would represent the response of the tissue to a chronic inflammatory process, thus indicating that it is a result of inflammation and not the cause thereof. Based on this theory, the cause of mammillary fistula would be similar to that of the various components of follicular occlusion syndrome, such as hidradenitis suppurativa, pilonidal cysts, dissecting cellulitis of the scalp, and acne conglobata.
Mammillary fistula behaves in much the same way as hidradenitis suppurativa, with a chronic, recurrent course characterized by flares of inflammatory activity and the formation of fistulas. Both conditions affect women aged 20 to 50 years, are closely related to smoking, and have a considerable impact on quality of life. Diagnosis in each of these conditions is based on clinical findings; ultrasound provides more accurate information for diagnosis. Hidradenitis suppurativa may appear at various sites, whereas mammillary fistula always affects the areola and nipple. Management is similar in both cases and includes antibiotics, anti-inflammatory agents, and surgery. The presence of both mammillary fistula and hidradenitis suppurativa in the same patient supports the notion that mammillary fistula may be yet another manifestation of hidradenitis suppurativa.4–6
In summary, mammillary fistula is probably underdiagnosed and relatively unknown by dermatologists and gynecologists. It should be suspected in the presence of recurrent abscesses of the areola. This entity shares clinical and—probably—etiological-pathogenic characteristics with hidradenitis suppurativa. Intralesional corticosteroids should be taken into consideration for treatment.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Sánchez-Pujol MJ, Álvarez-Chinchilla P, Docampo-Simón A, Pascual Ramírez JC. Fístula mamilar como una posible manifestación de una hidradenitis supurativa. Actas Dermosifiliogr. 2020;111:278–280.