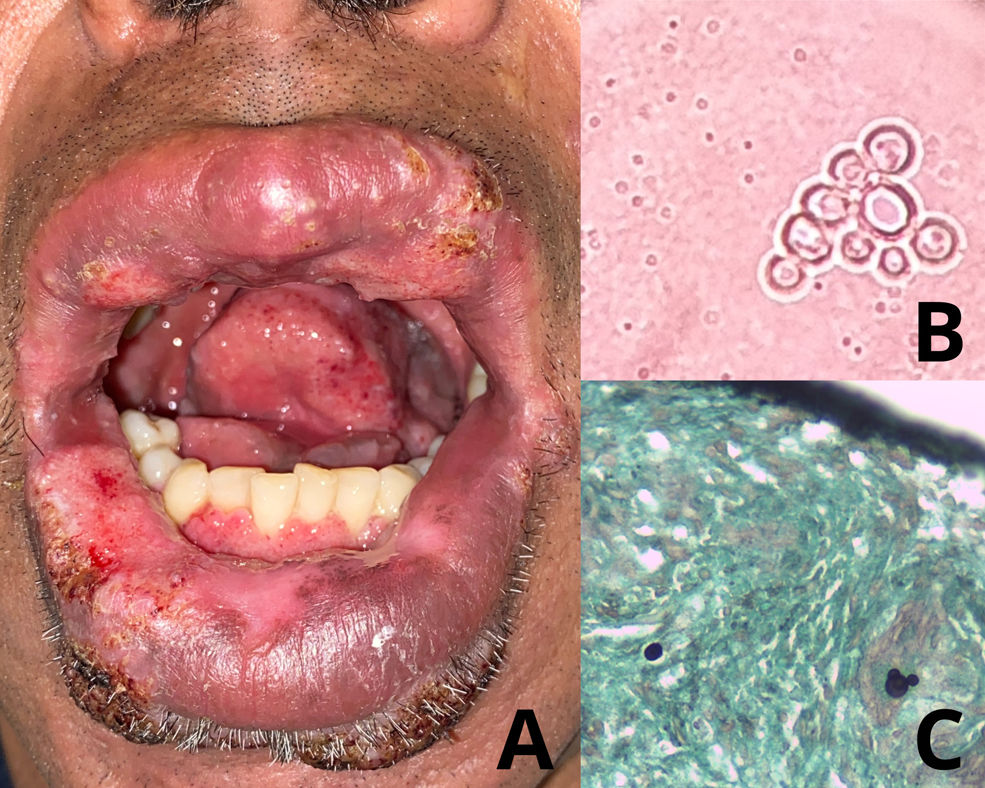
A 49-year-old Bolivian man, with no relevant personal medical history, presented with a >8-month history of oral lesions. On physical examination, he exhibited macrocheilia and multiple painful ulcers, with hemorrhagic punctate on their surface, affecting the oral and labial mucosa (Fig. 1A). Presumptive diagnoses included paracoccidioidomycosis, periorificial tuberculosis, mucocutaneous leishmaniasis, and chronic disseminated histoplasmosis. Direct examination revealed yeasts with multiple peripheral budding in a “pilot wheel” pattern (Fig. 1B). Histopathological study showed a chronic granulomatous inflammatory process with multinucleated giant cells. PAS and Grocott stains turned out positive for yeast-like elements with the same morphology as seen in the direct examination (Fig. 1C). A chest computed tomography scan revealed subpleural micronodular images with a bilateral centrilobular distribution and ground-glass pattern. Serologies and cultures were positive for Paracoccidioides brasiliensis.
What is your diagnosis?
DiagnosisMultifocal chronic paracoccidioidomycosis.
CommentsBased on the results of the direct observation, serologies, mycological culture, histopathology, and pulmonary involvement, a diagnosis of multifocal chronic paracoccidioidomycosis was established. Itraconazole 200mg/day was administered for 12 months, leading to complete remission of the mucocutaneous lesions.
Paracoccidioidomycosis is a fungal disease endemic to Latin American countries. Its etiological agent is the dimorphic fungus of the genus Paracoccidioides, and it can progress to a systemic granulomatous disease with visceral involvement.1–4 Natural infection occurs in both humans and animals and is acquired via the respiratory tract after inhaling airborne fungal conidia.1–3
Paracoccidioidomycosis manifests in 2 main clinical forms that are epidemiologically distinct. The acute/subacute form commonly affects children and young adults, presenting with ulcerated acneiform papules and scrofuloderma-like lesions, with a disseminated distribution. The chronic form is more common among adult men and manifests with lesions in the oral mucosa, respiratory tract, and lungs. This form of the disease appears months or years after infection and has been associated with certain risk factors. However, our patient did not present any of them. Clinically, it can manifest as painful ulcers with a granulomatous base and bleeding points on their surface, known as moriform stomatitis, and infiltration of the lips giving them a “tapir mouth” appearance.1–4
We must differentiate this entity from other diseases affecting the oral mucosa. The main differential diagnosis is squamous cell carcinoma, which is characterized by dysplasia and atypical mitoses on histopathological study. Mucocutaneous leishmaniasis and syphilis should also be considered. When there is pulmonary involvement, other causes of chronic granulomatous infections common in Latin America, such as tuberculosis and histoplasmosis, should be ruled out. Usually, the differential diagnosis is achieved through direct examination, culture, and PCR.1,5
Direct observation reveals large yeasts (4–40μm) with a characteristic morphology of multiple budding around the mother cell. This allows for early initiation of treatment while awaiting culture results. Biopsy frequently shows epidermal ulceration or pseudoepitheliomatous hyperplasia with a granulomatous inflammatory infiltrate in the dermis. PAS and Grocott stains allow visualization of double-walled yeasts arranged in a “pilot wheel” pattern.1–4
Treatment for mild and moderate forms involves a 12-month regimen of itraconazole at a dose of 200mg/day orally. In cases of severe or disseminated infection, liposomal amphotericin B is used at a dose of 3–5mg/kg/day IV for 2–4 weeks, followed by oral itraconazole.1
Conflicts of interestThe authors declare no conflict of interest.