A 43-year-old man from Brazil with no past history of interest consulted for pruritic skin lesions in sun-exposed areas that had appeared 3 weeks earlier. After 6 months they had spread and were accompanied by asthenia, arthralgia, and plaques of alopecia.
Physical ExaminationThe initial lesions consisted of edematous, erythematous plaques on the neckline, left preauricular area, lower left eyelid, and scalp (Fig. 1A). The condition progressed with the appearance of plaques of alopecia, oral ulcers, erythema and edema on both lower eyelids, and flagellate erythema on the back (Fig. 1B), as well as palmar papules, ulcers on the fingertips, and scaling and hyperkeratotic plaques on the sides of the fingers (Fig. 1C). Erythematous and hyperkeratotic plaques were observed on the elbows, knees, and both metacarpophalangeal and interphalangeal joints.
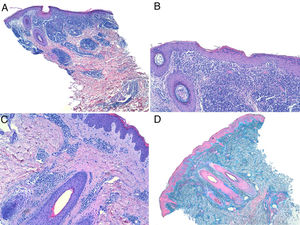
HistopathologyHistology (hematoxylin–eosin) of a 4-mm punch biopsy of a facial plaque showed an epidermis with orthokeratotic hyperkeratosis, vacuolation of the basal layer with few necrotic keratinocytes, and a superficial and deep perivascular and peradnexal lymphohistiocytic inflammatory infiltrate in the dermis (Fig. 2A–C). Mucin staining (Alcian blue) showed deposits in the dermis (Fig. 2D).
Additional TestsLaboratory tests revealed the presence of speckled cytoplasmic (titer, 1:80) and nucleolar (titer, 1:80) antinuclear antibody (ANA) and positivity for anti-MDA5 antibody (Ab). Creatine kinase and aldolase values were within the normal range. Combined positron emission tomography and computed tomography (PET–CT) findings and the results of respiratory function tests were normal.
What is your diagnosis?
DiagnosisAnti-MDA5-positive dermatomyositis (DM).
Clinical Course and TreatmentThe initial presumptive diagnosis was lupus tumidus. Based on the course of the cutaneous signs, the systemic manifestations, and the positive result for anti-MDA5 Ab, the diagnosis was switched to anti-MDA5-positive DM. The patient was treated with a topical corticosteroid, oral prednisone (1mg/kg/d), mycophenolate mofetil (2g/d), and topical 0.2% nitroglycerin for digital ulcers. Due to a poor response of the skin lesions, monthly intravenous immunoglobulin (Ig) was added to the treatment regimen, and mycophenolate mofetil was subsequently switched to off-label tofacitinib (5mg/12h). The patient showed almost complete resolution of the lesions 2 months after completing 6 cycles of intravenous Ig, which coincided with completion of 5 months of tofacitinib treatment (Fig. 3).
CommentDM is an idiopathic inflammatory myopathy with pathological changes that can be indistinguishable from lupus erythematosus. Recognition of the characteristic skin lesions can be the key to diagnosis.1
Patients with anti-MDA5-positive DM present with characteristic mucocutaneous signs, some due to underlying occlusive vasculopathy. Notable signs include painful oral ulcers, panniculitis, diffuse alopecia, painful skin ulcers that can progress to ischemia and necrosis, mechanic's hands, and often painful palmar papules (reverse Gottron sign). These patients have a lower incidence of myositis2,3,5 and a worse prognosis.3–5 The most important systemic manifestation is interstitial lung disease (prevalence 42%–100%), which frequently evolves to a rapidly progressive and sometimes fatal form. Therefore, respiratory function tests, lung diffusion capacity tests, and high-resolution computed tomography should be performed in all patients with DM and a positive anti-MDA5 Ab result.6 Other potential systemic manifestations include pneumomediastinum, edema of the hands, arthralgia and arthritis,4 fever, and asthenia.2 Affected patients appear to have a reduced risk of malignancy, although it is recommended that they undergo the same screening for neoplasia applied to all other DM patients.2
The differential diagnosis of early skin lesions includes lupus tumidus, Jessner lymphocytic infiltrate, and arthropod bites. Erythematous scaling plaques on extensor surfaces (Gottron sign) can be mistaken for psoriasis. Flagellate erythema can appear in DM, but has also been characteristically described in shiitake dermatitis, cancer patients treated with bleomycin, and adult-onset Still's disease.
Once associated neoplasia has been ruled out, the mainstay of DM treatment is high-dose systemic corticosteroids combined with immunosuppressants. The severity of cutaneous and systemic involvement, together with the presence of anti-MDA5 Ab, determines the intensity of treatment.6
In conclusion, we describe a clinical case with initial lesions suggestive of lupus tumidus that evolved to DM with characteristic features. The presence of anti-MDA5 Ab was key to establishing diagnosis.
Conflicts of InterestThe authors declare that they have no conflicts of interest.