A 52-year old patient with no relevant past medical history presented with an asymptomatic, slow-growing, homogenous nodular lesion on the lower lip that had appeared 10 years earlier. The patient was unable to relate the onset of the lesion to any event and had received no previous treatment.
Physical ExaminationThe patient had a well-defined pinkish-red nodule with superficial telangiectasia; the lesion infiltrated the full thickness of the lip, was painless on palpation, and measured 1.5cm in diameter (Fig. 1).
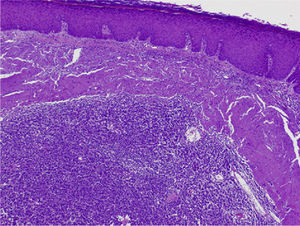
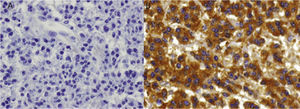
HistopathologyHematoxylin-eosin staining revealed the presence of lymphoid cell proliferation, consisting mainly of plasma cells in different stages of maturation, with involvement of striated muscle tissue (Fig. 2) and deposition of amorphous, homogeneous, eosinophilic, Congo red–positive material compatible with amyloid fibrils. Immunohistochemistry revealed κ light chain restriction but was negative for λ light chain and for CD20 (Fig. 3 A and B).
Additional TestsThe staging workup included laboratory tests (complete blood count, biochemistry, β2-microglobulin, and protein electrophoresis), myelogram, bone marrow biopsy, 24-hour urinary light chain excretion, bone marrow blood count, and bone marrow flow cytometry. The results of all studies were normal.
What Is Your Diagnosis?
DiagnosisPrimary cutaneous plasmacytoma.
Clinical Course and TreatmentThe lesion was excised and the patient is attending periodic check-ups with no recurrence.
CommentMalignant plasma cell tumors are usually systemic (multiple myeloma) and less often localized (solitary plasmacytoma). Localized tumors include solitary plasmacytomas of bone and extramedullary plasmacytomas. In 60% to 80% of cases extramedullary plasmacytomas are located in the upper respiratory tract. Primary skin lesions are very rare.1 Primary cutaneous plasmacytoma is included in the 2005 classification of the European Organization for Research and Treatment of Cancer (EORTC) among the marginal zone B-cell lymphomas,2 and originates from the clonal proliferation of immunoglobulin-secreting plasma cells in the absence of underlying multiple myeloma.1,3–5 It was first described by Stout and Frerichs in 19494 and accounts for 4% of extramedullary plasmacytomas.5
Mean age at diagnosis is 60 years, with a male-female ratio of 4:1.1,4,6 Clinically it presents as a slow-growing papule, plaque, or erythematous-violaceous nodule3,5 usually located on the trunk or in the facial region.3 It can take the form of a solitary tumor (62%) or may involve multiple sites (38%).6 Histopathology shows a nonepidermotropic dermal infiltrate of plasma cells at different stages of maturation. Immunohistochemistry is usually positive for CD79a, CD38, and CD138 and negative for CD20 and leukocyte common antigen; monotypic expression of immunoglobulin light chains is common.4,5 Since amyloid deposits are more often associated with secondary plasmacytomas, their presence should raise suspicion of an extracutaneous origin.1,2 Diagnosis is based on clinical, histopathologic, and immunohistochemical findings, and multiple myeloma must be ruled out by laboratory, radiologic, and bone marrow studies.6 Differential diagnosis is mainly with secondary cutaneous plasmacytoma, mucosal extramedullary plasmacytoma with secondary skin involvement, other primary B-cell lymphomas, and infectious diseases with significant infiltration of plasma cells, such as syphilis and Lyme disease.4 Solitary plasmacytoma progresses to multiple myeloma in one third of cases3 and cases with multiple or large lesions have the worst prognosis.1–4
The treatment for solitary tumors is surgery, which may be combined with radiation therapy and intralesional corticosteroid therapy.1,4.5 Chemotherapy should be considered when multiple lesions are present.2
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Prada-García C, et al. Nódulo de crecimiento progresivo localizado en el labio inferior. Actas Dermosifiliogr.2012;103:325-6.