Progressive cribriform and zosteriform hyperpigmentation (PCZH) is a skin disease first described by Rower et al.1 in 1978. Since then, several cases have been published in Korea but only 3 articles in the dermatology literature in English.2–4
This letter reports the case of a woman with hyperpigmented lesions on the right arm and on the right side of the trunk since childhood. These lesions were consistent with a diagnosis of PCZH.
The woman, aged 54 years, was white and had a personal history of fibromyalgia and asthma. She attended the clinic because of an asymptomatic hyperpigmented lesion on the back that had been present since she was 9 years old. Examination revealed several macular lesions with a homogeneous brown color and well-defined but irregular borders, grouped in a segmental pattern on normal skin on the right flank and arm, and the right side of the back and abdomen. These lesions did not cross the midline of the trunk (Figs. 1 and 2). No café-au-lait spots or neurofibromas were seen on unaffected skin.
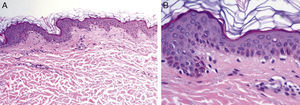
The patient did not recall any rash or prior trauma of the affected area although the lesions did increase in size in the first years after onset. She did not have any extracutaneous abnormalities or a family history of neurofibromatosis or similar skin lesions. A biopsy was taken from the affected area of the back. Histopathology showed an increase in cytoplasmic pigmentation of the cells of the basal epidermal layer (Fig. 3). In view of the clinical and histologic characteristics, a diagnosis of PCZH was made.
Rower et al.1 reported 5 patients with pigmentary abnormalities with certain characteristics in common that constituted the diagnostic criteria for PCZH. These characteristics were uniform and cribriform brown macular hyperpigmentation with a zosteriform distribution; a histologic pattern consistent with a mild increase in melanin pigment in cells of the basal layer and complete absence of nevus cells; no history of rash, injury, or inflammation that could suggest postinflammatory hyperpigmentation; onset after birth with gradual increase in extension; and absence of other cutaneous or internal abnormalities.
In 2012, Cho et al.4 published demographic, clinical, and histopathologic data from 30 Korean patients with PCZH. The authors observed a slight predominance of men, with an age of onset of PCZH between birth and 54 years (77% between 1 and 15 years). Only one individual reported a family history of similar lesions and none had associated extracutaneous congenital abnormalities. In general, the lesions were asymptomatic, cribriform, with a Blaschkoid distribution, and located preferentially on the trunk and limbs with a slight tendency towards right-sided predominance. The affected skin, in comparison with adjacent skin, showed increased pigmentation (more melanin granules) of the basal layer. Nevus cells were not present and there were no significant differences in the number of melanocytes. Likewise, there were no differences in other skin disorders except for cases with pigmentary incontinency. No effective treatment has been reported for PCZH. Terms such as reticulate hyperpigmentation of Iijima5 and reticulate zosteriform hyperpigmentation6 have been used to describe conditions with similar clinical and histopathologic findings.
Differential diagnosis of PCZH includes skin conditions that present with segmental hyperpigmented lesions such as linear and whorled nevoid hypermelanosis,4,5,8 café-au-lait spots,8,9 segmental pigmentation disorders with onset in the first months of life,8,9 and others such as Becker nevus (variant without hypertrichosis).4,8,10 Linear and whorled nevoid hypermelanosis is a diffuse asymmetric hyperpigmentation in lines or swirls along the Blaschko lines. The lesions appear at birth or within the first few weeks of life and then spread or darken during the first 2 years. These lesions are sometimes associated with extracutaneous disorders, particularly of neurologic, cardiac, and musculoskeletal nature.4,7,8 Despite the diffuse pattern, associated congenital abnormalities, and the different age of onset compared to PCZH, the clinical manifestations may sometimes overlap,7 and so some authors consider these conditions as part of spectrum of the same disease.2,3 Café-au-lait spots are usually round or oval, although they can follow a segmental distribution in segmental neurofibromatosis type 1 and have irregular borders in the McCune-Albright and Jaffe-Campanacci syndromes.8,9 Segmental pigmentation abnormalities appear in the first months of life as segmental hypopigmentation or hyperpigmentation, mainly on the trunk. They follow a block-like pattern with sharp confinement at the midline, particularly anteriorly, and can be associated with extracutaneous abnormalities.8,9
In conclusion, the findings in our case are similar to those reported by Cho et al.4 Bearing in mind the absence of associated conditions and the lack of therapeutic options, it is likely that PCZH is in fact more common than the limited number of reports in the literature would have us believe.
Please cite this article as: Monteagudo B, León-Mateos Á, Campo-Cerecedo F, Cabanillas M. Hiperpigmentación zosteriforme y cribiforme progresiva. Actas Dermosifiliogr. 2013;104:824–826.