Acral fibromyxoma (AF) is a rare benign tumor of soft tissues1 characterized by a solitary, painless, slow-growing nodule confined to the dermis and subcutaneous tissue. AF has a preference for acral areas, particularly the periungual and subungual regions of fingers and toes. It is more common in middle-aged adult men.2
Only 2 cases of AF-related digital clubbing (DC) have been described in the literature. DC is characterized by a focal enlargement in the terminal segments of the fingers due to the proliferation of connective tissue between the nail matrix and the distal phalanx. For confirmation, it is recommended to measure the profile angle, which should be >180°, and the ratio of the depth of the distal phalanx to the interphalangeal joint, which should be >1.3,4
Enchondromas, osteoid osteomas, myxoid cysts, and myxochondromas have been described as causes of DC, which results from an expansive process of the distal phalanx.3
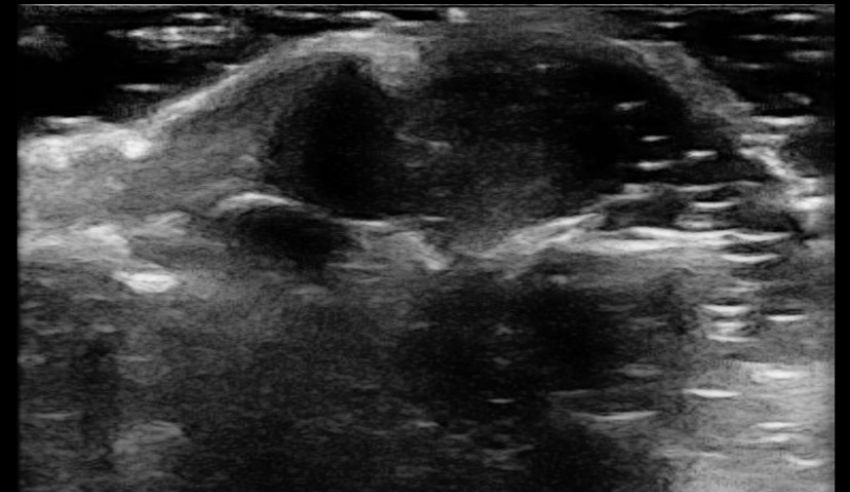
We describe a case of AF-related DC in a middle-aged woman, a 44-year-old woman with a 6-year history of a bulging in the distal portion of her right second finger, without associated symptoms but with esthetic discomfort. Dermatological examination revealed DC of the right second finger with mild subungual erythema (Fig. 1A). High-frequency ultrasound revealed the presence of a circumscribed hypoechoic subungual nodule, avascular on Doppler, with a central area of increased echogenicity and partial posterior acoustic shadowing (Fig. 2).
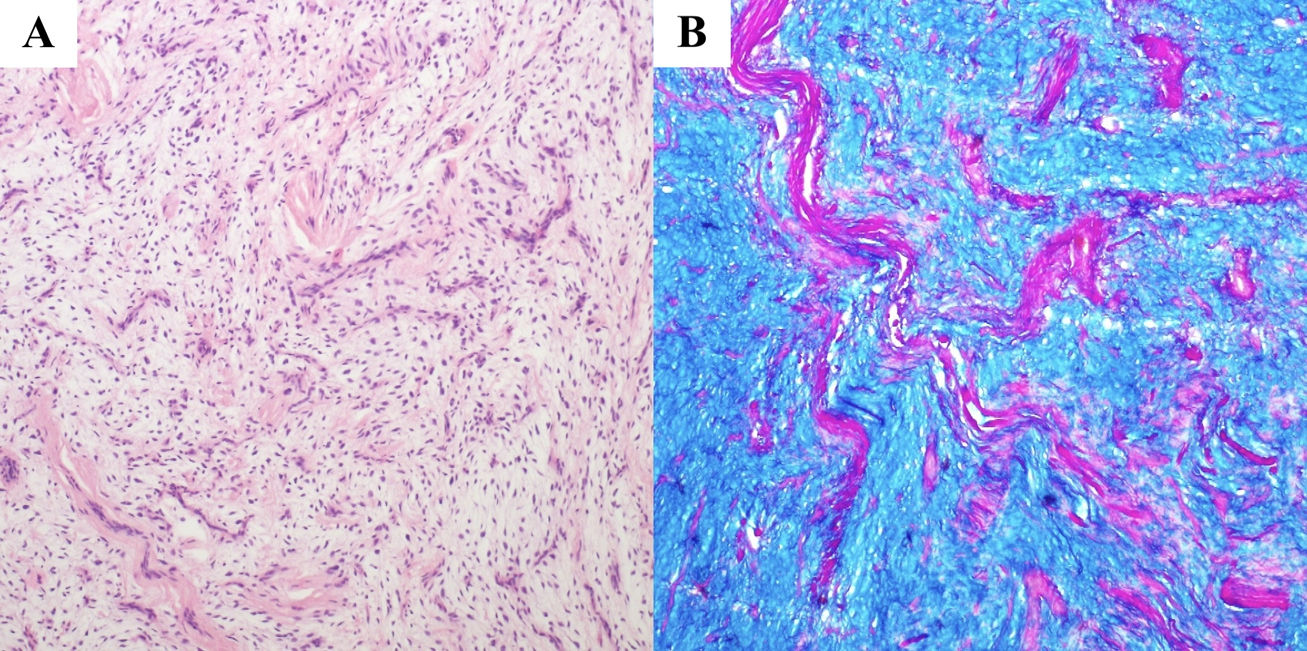
Subungual excision was performed revealing the presence of a benign mesenchymal neoplasm characterized by a proliferation of typical fibroblasts arranged in a disordered manner, within a loose fibrous stroma with a large amount of mucin, confirmed by colloid iron staining, presenting a myxoid appearance (Fig. 3). The superficial chorion revealed the presence of fibroblast proliferation and thickened collagen fibers forming bundles parallel to the epidermis, with proliferated and vertically oriented blood capillaries between them. The surgical margins were not evaluated due to specimen fragmentation. Immunohistochemistry was not performed either.
Four months after the intervention, the patient presented significant clinical improvement (Fig. 1B). Although the patient was advised on the need for reevaluation since surgical margins were not assessed, she declined a surgical procedure.
We report a classic case of AF: an indolent and painless tumor affecting the subungual region. Unlike epidemiology indicating a higher occurrence in men, our patient was a middle-aged woman.
The recognition of AF is challenging due to the wide range of differential diagnoses. Among them, dermatofibrosarcoma protuberans, myxoid neurofibroma, fibrous histiocytoma, acquired digital fibrokeratoma, acral mixed inflammatory fibroblastic sarcoma, sclerosing perineuroma, superficial angiomyxoma, and low-grade fibromyxoid sarcoma, in addition to the above-mentioned causes of DC.2,3
The classic histopathology of these tumors shows a dermal and sometimes subcutaneous proliferation of spindle or stellate cells within a myxoid, myxocollagenous, or collagenous matrix with prominent microvasculature and a mast cell infiltrate.3,5 Mild nuclear atypia and mitotic figures may be observed. Tumor is typically well-circumscribed but not encapsulated.2 Immunohistochemical analysis reveals the expression of CD34 in tumor cells and sometimes epithelial membrane antigen and smooth muscle actin, although those markers are not specific.2
Radiographic findings are nonspecific, but AF appears as a non-calcified soft tissue mass centered on the distal phalanx of the affected finger often associated with erosive or lytic lesions due to the tumor mass effect.2,6 Plain radiography is useful while studying this entity as it provides information on soft tissue mineralization and bone changes, aiding in the exclusion of differential diagnoses with malignancy and subungual exostosis.6
Data on high-frequency ultrasound findings in AF in the literature is scarce. Although it does not provide specific data for diagnosis, this examination modality provides information about the size of the tumor, its location, and internal characteristics.6 Doppler ultrasound can help delineate vascular lesions such as glomus tumors and hemangiomas from non-vascular lesions such as inclusion cysts.6
In our report, the ultrasound image revealed the presence of an avascular hypoechoic lesion with posterior shadowing, raising a differential diagnosis with inclusion cysts.
On magnetic resonance imaging, AF appears as a cystic lesion with hypointensity on T1-weighted sequences and hyperintensity on T2-weighted sequences.
The natural course of AF is benign, and the treatment of choice is surgical excision with adequate margins.2,5 There are few reports of recurrence after complete excision.6 Although there are no reports of malignancy, it is worth noting the few examples reported of increased cytological atypia that raise the possibility of malignant transformation.6,7 Short-term 6-month-to-1-year follow-up is needed due to the slow growth nature of AF and the potential for recurrence.2
AF needs to be better understood and recognized due to its rarity. We should always suspect this entity in cases of painless, slow-growing acral tumors. Proper identification, treatment, and follow-up are essential due to the risk, albeit low, of malignancy and recurrence.
ConsentsConsent for the publication of all patient photographs and medical information was provided by the authors at the time of article submission to the journal stating that all patients gave consent for their photographs and medical information to be published in print and online and with the understanding that this information may be publicly available.
FundingNone.
Conflicts of interestThe authors have no conflicts of interest to declare. This manuscript has not been presented elsewhere.