Granulomatous dermatitis has been associated with hematologic disorders, including the myelodysplastic syndromes. We describe the first case of granulomatous dermatitis associated with polycythemia vera, presenting as large erythematous nodules mimicking panniculitis. We also present the seventh case associated with myelodysplasia, with erythematous plaques on the face and neck, similar to a neutrophilic dermatosis. We consider it particularly interesting for dermatologists to be aware of this dermatosis as a nonspecific manifestation of various hematologic disorders. We suggest performing additional tests (complete blood count) to exclude the possibility that the skin manifestations are the initial sign of hematologic disease. Furthermore, we propose using the broader term, granulomatous dermatitis, to refer to these disorders as, although there are more reports of interstitial forms, cases with a more nodular presentation have also been published, and the importance of the diagnosis derives not from the subtype but from the relationship with an underlying disease.
Las dermatitis de patrón granulomatoso se han relacionado con trastornos hematológicos, entre ellos los síndromes mielodisplásicos. En este artículo se describe el primer caso de dermatitis granulomatosa asociado a policitemia vera, en forma de grandes nódulos eritematosos simulando paniculitis, y el séptimo caso asociado a mielodisplasia, con placas eritematosas en cara y cuello que recordaban a una dermatosis neutrofílica. Consideramos de especial interés para el dermatólogo conocer esta dermatosis como manifestación no específica de diferentes trastornos hematológicos, y sugerimos la realización de un estudio complementario (hemograma) en el caso de que la clínica cutánea sea el comienzo. Del mismo modo, proponemos el término más amplio de dermatitis granulomatosas para denominarlas, puesto que, si bien las formas intersticiales son más numerosas en la literatura, también se han publicado casos más nodulares, y la importancia de su diagnóstico no radica en el subtipo sino en su relación con un trastorno subyacente.
Since it was first described in association with rheumatoid arthritis,1 interstitial granulomatous dermatitis (IGD) has been associated with hematologic diseases,2–4 specifically, myelodysplastic syndromes, which account for most cases. Here, we report the first case of noninterstitial granulomatous dermatitis (NIGD) associated with polycythemia vera (PV) and a new case of IGD associated with myelodysplasia.
Case DescriptionsPatient 1The patient was a 72-year-old Spanish woman who had never traveled outside Europe and had a history of PV that was being treated with hydroxyurea and acetylsalicylic acid. She reported the onset of diffuse skin lesions 5 years after diagnosis of her hematologic disease. The lesions consisted of 15-20 erythematous plaques measuring 1-3cm on her back, chest, and the outer surface of both arms. The diagnoses proposed were infection, neutrophilic dermatosis, and lupus tumidus (Fig. 1). The initial biopsy revealed a superficial and deep lymphocytic inflammatory infiltrate around the vessels, follicles, and adnexa, with no mucin deposits. The findings were compatible with a diagnosis of lupus tumidus. The patient refused treatment with hydroxychloroquine. The lesions eventually resolved without treatment, although they did reappear. Eighteen months later, lesions similar to the original lesions and 4 large erythematous painless nodules appeared on both legs, indicating lupus panniculitis. Analysis of a new biopsy specimen showed a superficial and deep perivascular lymphocytic infiltrate composed of mature cells and with no cytologic atypia (CD4+, CD2+, and CD5+ [majority]; CD8+, CD79+, and CD20+ [minority]; occasional CD30+) accompanied by histiocytes (CD68+) and plasma cells. No epidermal or hypodermal abnormalities or mucin were observed. Hydroxyurea and acetylsalicylic acid were suspended despite the low degree of suspected causality, and treatment with doxycycline 100mg/d was prescribed for 2 months, although the lesions did not resolve completely. One year later, the patient experienced a new outbreak of nodules and plaques on the upper and lower limbs. Body hair, sensitivity, and sweating remained unaffected (Fig. 2). Examination of the biopsy revealed a superficial and deep histiocytic inflammatory infiltrate that tended to form interstitial granulomas in some areas and nodular granulomas in others (no fibrinoid necrosis). The granulomas were surrounded by mature lymphocytes (CD4+, CD8–, CD20–, and CD30–) with no cytologic atypia (Fig. 3). No intracytoplasmic histiocytic bodies suggestive of leishmaniasis were observed. Similarly, no exogenous material was visible to the naked eye or under polarized light. The results of Ziehl-Neelsen staining, culture (bacteria, mycobacteria, and fungi), and serology testing (human immunodeficiency virus and syphilis) were negative. The results for acute phase reactants and autoimmunity studies (antinuclear antibodies, anti–native DNA antibodies, anti–extractable nuclear antigen antibodies, and complement [C3 and C4]) were normal. Polymerase chain reaction was not performed to rule out leishmaniasis, since the intermittent lesions resolved with corticosteroids or without treatment. Once the diagnosis of granulomatous dermatitis had been confirmed, the previously discontinued drugs were reintroduced, with no worsening of the patient's condition. At present, the patient is stable with prednisone every 48hours, and, while the infiltration has diminished, it has not resolved.
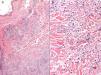
A, Superficial and deep dermal inflammatory infiltrate (hematoxylin-eosin, original magnification, ×4). B, Tendency to form interstitial granulomas in some areas, with a more nodular appearance in others (no fibrinoid necrosis), surrounded by mature lymphocytes without cytologic atypia (hematoxylin-eosin, original magnification, ×10).
The patient was a 74-year-old Spanish man who had never traveled outside Spain. He had been diagnosed with refractory anemia with excess blasts type 1 a year previously and was referred with skin lesions accompanied by arthralgia and no signs of frank arthritis. The lesions were erythematous plaques measuring 2-3cm on his forehead, neck, and cheek. Sensitivity, body hair, and sweating remained unaffected (Fig. 4). Three months earlier he had presented with similar lesions 1 month after the first cycle of therapy with azacytidine; the lesions resolved completely with prednisone at 0.5mg/kg/d. The skin biopsy revealed a superficial, deep, periadnexal perivascular inflammatory infiltrate consisting of mature lymphocytes without atypia accompanied by interstitial histiocytic granulomas (no necrosis) (Fig. 5), scant eosinophils, and multinucleated giant cells. Vacuolar degeneration of the basement membrane and necrotic keratinocytes were observed in specific areas. Standard microscopy and polarized light microscopy revealed no foreign bodies or intracytoplasmic bodies. The results of culture and serology testing for syphilis and human immunodeficiency virus were negative. Immunohistochemistry (CD15 staining) revealed few cells. The results of direct immunofluorescence (IgG, IgM, IgA, C3, and fibrinogen) and Ziehl-Neelsen staining were also negative. The blood workup was remarkable—other than for the patient's myelodysplasia—for levels of C-reactive protein (16.7mg/dL) and the erythrocyte sedimentation rate (88mm). All other parameters—antinuclear antibodies, anti–native DNA antibodies, anti–extractable nuclear antigen antibodies, and complement (C3, and C4)—were normal. As in the previous case, no molecular studies to rule out leishmaniasis were performed. The lesions resolved without treatment after 1 month and did not reappear with subsequent cycles of azacytidine. Three years later, the myelodysplasia has progressed to acute myeloid leukemia.
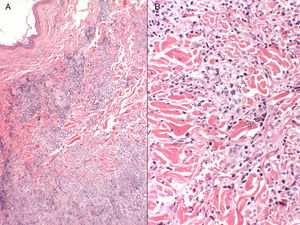
A, Superficial and deep perivascular and periadnexal inflammatory infiltrate (hematoxylin-eosin, original magnification, ×4). B, Inflammatory infiltrate composed of mature lymphocytes and interstitial histiocytic granulomas, without necrosis (hematoxylin-eosin, original magnification, ×20).
In 1993, Vestey et al.5 reported the first 2 cases of granulomatous skin lesions associated with myelodysplastic syndrome; the cases involved diffuse papular eruptions with histology of sarcoidosis in one case and granuloma annulare in the other. Again in 1993, Ackerman1 first reported the pattern of IGD, which in this case was associated with rheumatoid arthritis, as a dermal infiltrate composed mainly of histiocytes distributed interstitially and in palisades around small bundles of degenerated collagen, with scant or no mucin deposits and a limited number of eosinophils and neutrophils. Katz6 was the first to describe a cutaneous granulomatous eruption that differed from granuloma annulare, sarcoidosis, and IGD. The eruption was described as a multinodular, perivascular, and periadnexal histiocytic infiltrate with small lymphocytes and plasma cells. As in patient 2 (see above), this eruption involved medium-sized erythematous nodules (1-5cm) on the face, scalp, and neck. The author described the finding simply as a cutaneous granulomatous eruption. The report was published because of the association between the eruption and myelodysplasia. Aung et al.7 recently used the term NIGD to describe a case associated with myelodysplasia; the case reported by Katz could be included under this term. The case report described a large erythematous plaque covering the patient's arm and mimicking cellulitis, followed by the appearance of 2 linear plaques on the elbow. Cornejo et al.8 performed a joint analysis of biopsy specimens from IGD and NIGD at different stages of development in lesions from the same patient with myelodysplasia; the first corresponded to papular lesions and the second to nodules. It is noteworthy that, in this case, a third biopsy specimen from a more disseminated phase of the patient's skin disease revealed that the granulomatous pattern merged with leukemia cutis (cells with large myeloperoxidase-positive hyperchromatic nuclei). Progression of leukemia was subsequently confirmed in bone marrow.
In addition to the clinical findings of a papular eruption, nodules, and a large plaque mimicking pyodermatitis reported to date, attention should be drawn to the findings of Patsinakidis et al.,9 who reported large urticariform and annular plaques on the thighs, trunk, and arms, with biopsy-proven IGD in the context of myelodysplasia. The most extensive disease was reported by Balin et al.,10 who described histopathologically confirmed IGD in the form of plaques and papules coalescing on the trunk and limbs and covering 80% of the total body surface.
In the first case we report, the biopsy specimens revealed various histopathological patterns developing in parallel, thus demonstrating a histological spectrum within this reactive process.
The cases we report here are the first case in which NIGD is associated with PV and the seventh in which granulomatous dermatitis is associated with myelodysplasia in a broad context (granuloma annulare, sarcoidosis, IGD, and NIGD). We feel that these cases should be brought together under the wider term granulomatous dermatitis, which would include all the subtypes, thus giving precedence to the fact that these granulomas are a reactive or paraneoplastic manifestation of hematologic disorders, such as myelodysplasia and PV. Therefore, at least 1 complete blood count should be performed as part of the extension study in these patients.
Ethical DisclosuresProtection of humans and animalsThe authors declare that no tests were carried out in humans or animals for the purpose of this study.
Confidentiality of dataThe authors declare that no private patient data appear in this article.
Right to privacy and informed consentThe authors obtained informed consent from the patients and/or subjects referred to in this article. This document is held by the corresponding author.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Lozano-Masdemont B, Baniandrés-Rodríguez O, Parra-Blanco V, Suárez-Fernández R. Dermatitis granulomatosa como manifestación cutánea de trastornos hematológicos: primer caso asociado a policitemia vera y un nuevo caso asociado a mielodisplasia. Actas Dermosifiliogr. 2016;107:e27–e32.