Hydroxyurea (HU) is an anticancer agent that inhibits DNA synthesis through its action on the enzyme ribonucleotide reductase.1 It is used in chronic myeloproliferative diseases such as polycythemia vera, chronic myeloid leukemia, and essential thrombocytosis, although it has also been prescribed to patients with refractory psoriasis.2
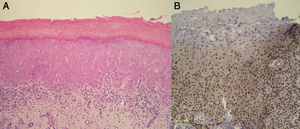
We present the case of a 76-year-old woman diagnosed with idiopathic myelofibrosis and on treatment with HU since 2004. Four years after starting treatment with HU, the patient consulted for desquamating erythematous plaques over the interphalangeal joints, periorbital erythema, and erythematous papular lesions in the frontal (Fig. 1A) and retroauricular (Fig. 1B) regions. In addition, she had a painful ulcer of approximately 3cm diameter over the medial malleolus; the ulcer had a whitish base and was surrounded by atrophic erythematous skin. She did not report muscle weakness or dysphagia. Laboratory tests including muscle enzymes, acute phase reactants, and autoantibodies were normal. A biopsy taken from the dorsum of the hand revealed an acanthotic epidermis with hyperkeratosis, dyskeratosis, and vacuolization of the basal layer, associated with a lichenoid inflammatory infiltrate at the dermoepidermal interface. Additionally, the epidermis showed keratinocyte disorganization and atypia with large nuclei (Fig. 2A). On immunohistochemistry there was intense expression of p53 in the dysplastic keratinocytes (Fig. 2B). These clinical and pathologic findings were consistent with a dermatomyositis (DM) like rash and squamous dysplasia associated with treatment with HU. It was decided to change the treatment to anagrelide, and a clear improvement of the skin lesions was observed at 10 months (Fig. 3). The patient remains on periodic follow-up in dermatology.
Patients on long-term therapy with HU can develop various side effects, including a wide variety of mucocutaneous manifestations, which appear in 10% to 35% of patients. The most common skin changes are facial erythema, hyperpigmentation, xerosis, alopecia, skin atrophy, melanonychia, and ulcers on the lower limbs. Other less frequent adverse effects are DM-like rash and nonmelanoma skin cancer (NMSC).3 DM-like rash resembles true DM both clinically and histologically. It presents as desquamating erythematous papules or plaques on the dorsum of the hands, typically associated with facial erythema and pronounced xerosis of the skin. Patients rarely report other accompanying symptoms and there are usually no significant alterations of laboratory tests. Histologically, a lichenoid inflammatory infiltrate is found at the dermoepidermal interface, with vacuolization of the basal layer, dyskeratosis, and, rarely, mucin deposition.4 Chronic ulcerative lesions may also be present, particularly in areas susceptible to trauma, such as the malleolar region, the dorsum of the foot, and the heel. These ulcers are typically very painful and resolve spontaneously after withdrawal of the HU.5
It is also known that HU is associated with the appearance of squamous cell carcinoma, which arises after a latency period of 2 to 13 years. These tumors are usually aggressive, and the treatment must be withdrawn.6 In 2004, Sánchez-Palacios and Guitart7 proposed the term HU-related squamous dysplasia as a precancerous precursor condition of NMSC, and they identified the expression of p53 in the basal layer of the epidermis, demonstrating that this is a premalignant condition. Recently, Kalajian et al.3 also described a case of DM-like rash in which focal p53 expression was detected in the basal layer of the epidermis. Those authors suggested that DM-like manifestations should be considered a premalignant entity that requires periodic follow-up and the withdrawal of treatment with HU.
In our case the patient presented skin lesions clinically and histologically compatible with DM, but the biopsy revealed the presence of dysplastic keratinocytes with intense expression of p53. We therefore considered that this was an HU-induced DM-like rash presenting simultaneously with HU-induced squamous dysplasia; both of these clinical manifestations have an underlying phototoxic mechanism. It should also be noted that the lesions resolved completely after the withdrawal of treatment; this would support the implication of HU in the skin manifestations.
In conclusion, HU is a drug associated with marked skin toxicity. In patients who present lesions clinically and histologically consistent with DM-like rash, the treatment must be withdrawn and close follow-up initiated because of the risk of appearance of potentially aggressive carcinomas.
Please cite this article as: de Unamuno-Bustos B, Ballester-Sánchez R, Sabater Marco V, Vilata-Corell JJ. Erupción dermatomiositis-like asociada al tratamiento con hidroxiurea: ¿una entidad premaligna?. Actas Dermosifiliogr. 2014;105:876–878.