The external nose is a sun-exposed area with a high incidence of skin tumors. These tumors are treated surgically in the majority of cases. The nasal ala, composed of mucosa, cartilage, and skin, is an anatomically complex structure and its reconstruction is thus also complex.1 During reconstruction of defects of the ala we must take into account the size and thickness of the defect, the color and texture of the surrounding skin, symmetry with the contralateral ala, and the condition of the perilesional tissues. We must also evaluate the characteristics of possible donor sites and the patient's past history. The main objective is to preserve the valve function and the cosmetic appearance of the external nose.
We describe the case of a 77-year-old woman with a complex past history. She presented biopsy-confirmed recurrence of basal cell carcinoma on the right nasal ala.
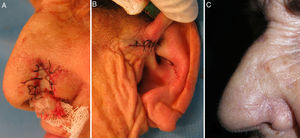
The tumor recurrence (Fig. 1A) was treated using Mohs micrographic surgery (Fig. 1B), with complete excision being achieved in a single stage. This surgery left a full-thickness defect of the nasal ala measuring 0.8×1cm, affecting the free border of the ala.
To repair the defect we decided to use a composite chondrocutaneous graft from the base of the helix. In this situation, the ideal donor site is the auricle of the ear not only for color and texture, but also because the anterior region of the helix permits simple graft extraction and direct closure.2 The graft obtained presents cartilage between 2 skin surfaces. The cartilage provides mechanical stability and form to the graft and to the nasal ala, preventing collapse of the graft with respiratory movements.3 Additionally, the cartilage prevents scar retraction and secondarily preserves valve function.
In our patient, we first designed and excised a V-shaped en bloc graft from the base of the helix, 1mm larger than the defect (Fig. 1C).4 The resulting defect in the helix was closed using interrupted sutures (Fig. 2B).
To fix the graft to the receptor site, we first sutured the tissue to the internal surface of the nasal ala using an absorbable 5/0 suture. The graft was then immobilized using a nasal pack. Finally, the skin of the external surface was sutured with 5/0 silk (Fig. 2A).3
The use of a composite graft from the auricle of the ear to reconstruct the external nose was first described by Konig5 in 1902. Its main advantages are that surgery can be performed in a single stage, with an en bloc graft, allowing the procedure to be completed in a single operation.
Factors that can reduce chondrocutaneous graft survival include smoking, alteration of the vascular supply by previous radiotherapy, the presence of scars, diabetes, and severe arteriosclerosis. Large grafts have high metabolic demands, reducing their likelihood of survival. Previous reports have therefore recommended a maximum diameter of 10mm for chondrocutaneous grafts.3,4,6 However, good results have been reported with grafts up to 10×18mm.7 Ideally, the center of the graft should be at no more than 5mm from the blood supply.
Complications that can arise after extraction of the graft include asymmetry or contracture of the auricle of the ear, deformity, and a hypertrophic or hypo- or hyperpigmented scar.
This chondrocutaneous graft makes it possible to perform reconstruction of the 3 layers of the nasal ala in a single operation, preserving function and cosmetic appearance (Fig. 2C). It is a good option for defects with a diameter up to 1cm.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Kueder-Pajares T, Prada-García C, Sanchez-Sambucety P, Rodriguez-Prieto MA. Reconstrucción del ala nasal mediante injerto condrocutáneo. Actas Dermosifiliogr. 2017;108:488–490.