Primary cutaneous lymphomas are a heterogeneous group of non-Hodgkin's lymphomas, most of them chronic with multiple relapses, which can have an impact on the patient's quality of life. The main aim of the study was to assess the quality of life of patients with cutaneous lymphomas using different validated questionnaires. A total of 32 patients were included in the study (mean age, 64 years; 75% men). A total of 68.8% of lymphomas were mycosis fungoides. Age, number of therapies administered and pruritus were associated with worse quality of life as assessed by the different questionnaires. The use of quality of life-questionnaires may be useful in the holistic evaluation of the patient.
Los linfomas cutáneos primarios son un grupo heterogéneo de linfomas de tipo no Hodgkin, la mayoría de carácter crónico con múltiples recaídas, que pueden provocar una repercusión en la calidad de vida. El objetivo principal del estudio fue evaluar la calidad de vida de los pacientes con linfomas cutáneos mediante el empleo de diferentes cuestionarios validados. Se incluyeron 32 pacientes en el estudio, con una edad media de 64 años, siendo el 75% varones y el 68,8% de los linfomas de tipo micosis fungoide. La edad, el número de tratamientos empleados y el prurito se asociaron a una peor calidad de vida, evaluada por los diferentes cuestionarios. El empleo de cuestionarios de calidad de vida puede ser útil en la evaluación holística del paciente.
Primary cutaneous lymphomas (PCLs) represent a heterogeneous group of non-Hodgkin lymphomas whose first clinical manifestation occurs in the skin without evidence of extracutaneous involvement at the time of diagnosis.1 A total of 75–80% of PCLs are cutaneous T-cell lymphomas (CTCLs), and the remaining 20–25%, cutaneous B-cell lymphomas (CBCLs).2 Of all these, mycosis fungoides (MF) is the most frequent form, which, along with Sézary syndrome (SS), accounts for almost half of all PCLs.3
Currently, there is no curative treatment, so most PCLs run a chronic course with multiple relapses. Furthermore, the visibility of the lesions along with skin involvement such as itching, desquamation, and pain can significantly impact the patients’ quality of life (QOL).4,5 In PCLs, the use of questionnaires to assess QOL has been poorly studied, with existing studies focusing on CTCLs.6–12 Therefore, we initiated this study with the primary endpoint of evaluating QOL in patients with PCLs. Secondarily, we aimed to explore factors associated with poorer QOL and compare QOL between patients with MF, as it is the most frequent type, and other PCLs.
Patients and methodsWe conducted a cross-sectional study with patients diagnosed with any type of PCL, regardless of their severity and treatment level on therapy at the Cutaneous Lymphoma Unit of Hospital Universitario Virgen de las Nieves. The patient inclusion period for the study went from February to May 2024.
Demographic and clinical data (age, sex, type of lymphoma, duration of evolution, etc.) were collected, and the various study questionnaires were completed. Questionnaires related to disease severity were the Modified Severity-Weighted Assessment Tool (mSWAT) and the Itch Severity Scale (ISS). Questionnaires to evaluate quality of life and well-being were Skindex-29, the Dermatology Life Quality Index (DLQI), the Hospital Anxiety and Depression Scale (HADS), and the WHO-5 Well-Being Index questionnaire.
All statistical analyses were performed with the SPSS® package (SPSS for Mac, Version 21.0 Chicago: SPSS Inc.).
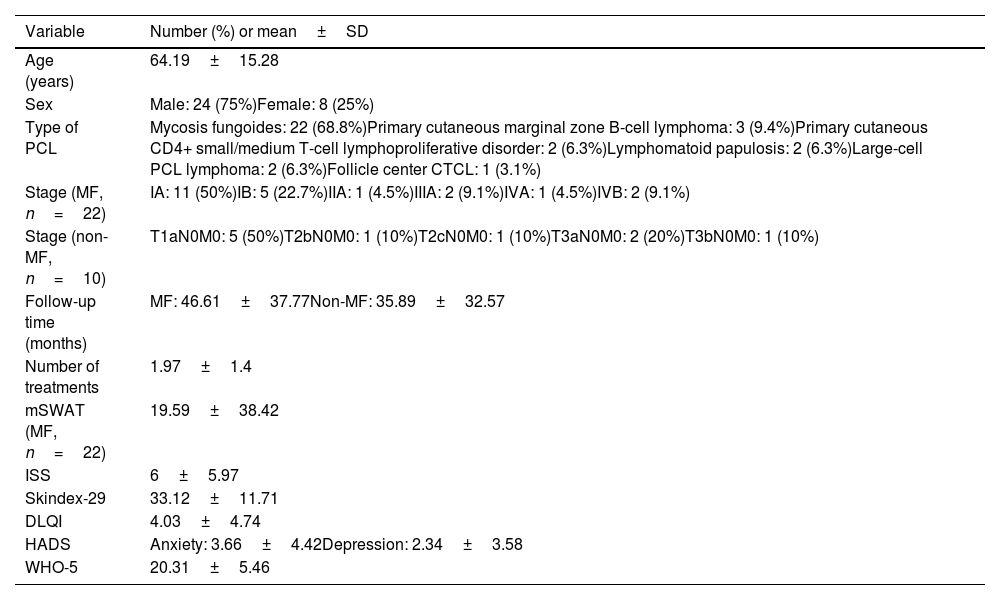
ResultsA total of 32 patients with PCLs were included in the study, with a mean course of the disease of 79.31±79.02 months. The clinical/epidemiological characteristics studied are shown in Table 1.
Sociodemographic and clinical characteristics of the sample (n=32).
| Variable | Number (%) or mean±SD |
|---|---|
| Age (years) | 64.19±15.28 |
| Sex | Male: 24 (75%)Female: 8 (25%) |
| Type of PCL | Mycosis fungoides: 22 (68.8%)Primary cutaneous marginal zone B-cell lymphoma: 3 (9.4%)Primary cutaneous CD4+ small/medium T-cell lymphoproliferative disorder: 2 (6.3%)Lymphomatoid papulosis: 2 (6.3%)Large-cell PCL lymphoma: 2 (6.3%)Follicle center CTCL: 1 (3.1%) |
| Stage (MF, n=22) | IA: 11 (50%)IB: 5 (22.7%)IIA: 1 (4.5%)IIIA: 2 (9.1%)IVA: 1 (4.5%)IVB: 2 (9.1%) |
| Stage (non-MF, n=10) | T1aN0M0: 5 (50%)T2bN0M0: 1 (10%)T2cN0M0: 1 (10%)T3aN0M0: 2 (20%)T3bN0M0: 1 (10%) |
| Follow-up time (months) | MF: 46.61±37.77Non-MF: 35.89±32.57 |
| Number of treatments | 1.97±1.4 |
| mSWAT (MF, n=22) | 19.59±38.42 |
| ISS | 6±5.97 |
| Skindex-29 | 33.12±11.71 |
| DLQI | 4.03±4.74 |
| HADS | Anxiety: 3.66±4.42Depression: 2.34±3.58 |
| WHO-5 | 20.31±5.46 |
SD, standard deviation; DLQI, Dermatology Life Quality Index; HADS, Hospital Anxiety and Depression Scale; ISS, Itch Severity Scale; CTCL, cutaneous T-cell lymphoma; PCL, primary cutaneous lymphomas; MF, mycosis fungoides; mSWAT, Modified Severity-Weighted Assessment Tool.
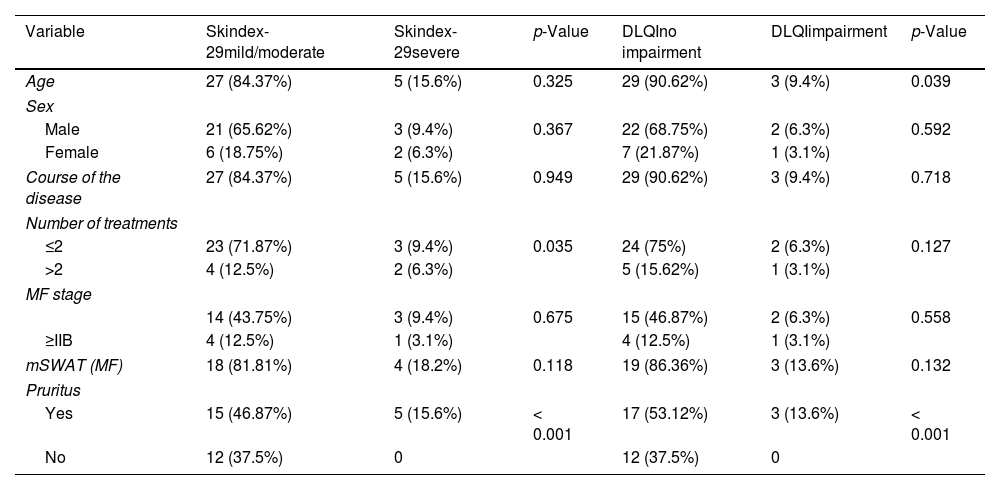
Bivariate analysis was performed to identify factors associated with a poorer quality of life (Table 2). Older age was associated with a higher DLQI score (p=0.039). A higher Skindex-29 score was found in patients with a greater number of previous treatments (p=0.035). Finally, the presence of pruritus was statistically significantly associated with higher scores on Skindex-29 (p<0.001), DLQI (p<0.001), WHO-5 (p=0.003), and HADS, in both the anxiety (p=0.007) and the depression subscales (p=0.010). No statistically significant findings were found for the rest of the variables.
Analysis of factors associated with higher scores in Skindex-29, DLQI, HADS, and WHO-5.
| Variable | Skindex-29mild/moderate | Skindex-29severe | p-Value | DLQIno impairment | DLQIimpairment | p-Value |
|---|---|---|---|---|---|---|
| Age | 27 (84.37%) | 5 (15.6%) | 0.325 | 29 (90.62%) | 3 (9.4%) | 0.039 |
| Sex | ||||||
| Male | 21 (65.62%) | 3 (9.4%) | 0.367 | 22 (68.75%) | 2 (6.3%) | 0.592 |
| Female | 6 (18.75%) | 2 (6.3%) | 7 (21.87%) | 1 (3.1%) | ||
| Course of the disease | 27 (84.37%) | 5 (15.6%) | 0.949 | 29 (90.62%) | 3 (9.4%) | 0.718 |
| Number of treatments | ||||||
| ≤2 | 23 (71.87%) | 3 (9.4%) | 0.035 | 24 (75%) | 2 (6.3%) | 0.127 |
| >2 | 4 (12.5%) | 2 (6.3%) | 5 (15.62%) | 1 (3.1%) | ||
| MF stage | ||||||
| 14 (43.75%) | 3 (9.4%) | 0.675 | 15 (46.87%) | 2 (6.3%) | 0.558 | |
| ≥IIB | 4 (12.5%) | 1 (3.1%) | 4 (12.5%) | 1 (3.1%) | ||
| mSWAT (MF) | 18 (81.81%) | 4 (18.2%) | 0.118 | 19 (86.36%) | 3 (13.6%) | 0.132 |
| Pruritus | ||||||
| Yes | 15 (46.87%) | 5 (15.6%) | < 0.001 | 17 (53.12%) | 3 (13.6%) | < 0.001 |
| No | 12 (37.5%) | 0 | 12 (37.5%) | 0 | ||
| Variables | HADS | p-value | WHO-5 | p-value | |||||
|---|---|---|---|---|---|---|---|---|---|
| Anxiety (A) | Depression (D) | No impairment (>13) | No impairment (≤13) | ||||||
| <10 | ≥10 | <10 | ≥10 | A | D | ||||
| Age | 27 (84.3%) | 5 (15.6%) | 30 (93.7%) | 2 (6.3%) | 0.195 | 0.554 | 28 (87.5%) | 4 (12.5%) | 0.271 |
| Sex | |||||||||
| Male | 22 (68.7%) | 2 (6.3%) | 23 (71.8%) | 1 (3.1%) | 0.085 | 0.444 | 21 (65.6%) | 3 (9.4%) | 0.746 |
| Female | 5 (15.6%) | 3 (9.4%) | 7 (21.8%) | 1 (3.1%) | 7 (21.8%) | 1 (3.1%) | |||
| Course of the disease | 27 (84.3%) | 5 (15.6%) | 30 (93.7%) | 2 (6.3%) | 0.798 | 0.661 | 28 (87.5%) | 4 (12.5%) | 0.570 |
| Number of treatments received | |||||||||
| ≤2 | 22 (68.7%) | 4 (12.5%) | 24 (75%) | 2 (6.3%) | 0.098 | 0.532 | 23 (71.6%) | 3 (9.4%) | 0.424 |
| >2 | 5 (15.6%) | 1 (3.1%) | 6 (18.7%) | 0 | 5 (15.6%) | 1 (3.1%) | |||
| MF Stage | |||||||||
| 14 (63.6%) | 3 (13.6%) | 15 (68.2%) | 2 (9%) | 0.675 | 0.589 | 14 (63.6%) | 3 (13.6%) | 0.675 | |
| ≥IIB | 4 (18.2%) | 1 (4.5%) | 5 (22.7%) | 0 | 4 (18.2%) | 1 (4.5%) | |||
| mSWAT MF | 18 (81.8%) | 4 (18.2%) | 20 (90.9%) | 2 (9%) | 0.195 | 0.554 | 18 (81.8%) | 4 (18.2%) | 0.484 |
| Pruritus | |||||||||
| Yes | 15 (46.8%) | 5 (15.6%) | 18 (56.2%) | 2 (6.3%) | 0.007 | 0.010 | 16 (50%) | 4 (12.5%) | 0.003 |
| No | 12 (37.5%) | 0 | 12 (37.5%) | 0 | 12 (37.5%) | 0 | |||
Scores on the Skindex-29 were classified as mild/moderate (<44) or severe (≥44). For the DLQI, scores indicated no impact on quality of life (<11) or impact (≥11). On the HADS, scores were categorized as unlikely case (<10) or likely case (≥10) of anxiety/depression. Finally, for the WHO-5, scores suggested no impact on well-being (<13) or impact (≥13).
DLQI, Dermatology Life Quality Index; HADS, Hospital Anxiety and Depression Scale; MF, mycosis fungoides; mSWAT, Modified Severity-Weighted Assessment Tool.
Bivariate analysis was performed to compare quality of life between patients with MF, as it is the most frequent type, and other PCLs. The prevalence of pruritus in patients with mycosis fungoides was 75%, while in the group of other cutaneous lymphomas it was 41.7%; of the total patients with pruritus, only 1 had B-cell lymphoma, being the remaining 19 T-cell lymphomas. Nonetheless, no statistically significant differences were found. No statistically significant differences were found either between MF and other PCLs in the different quality of life questionnaires used.
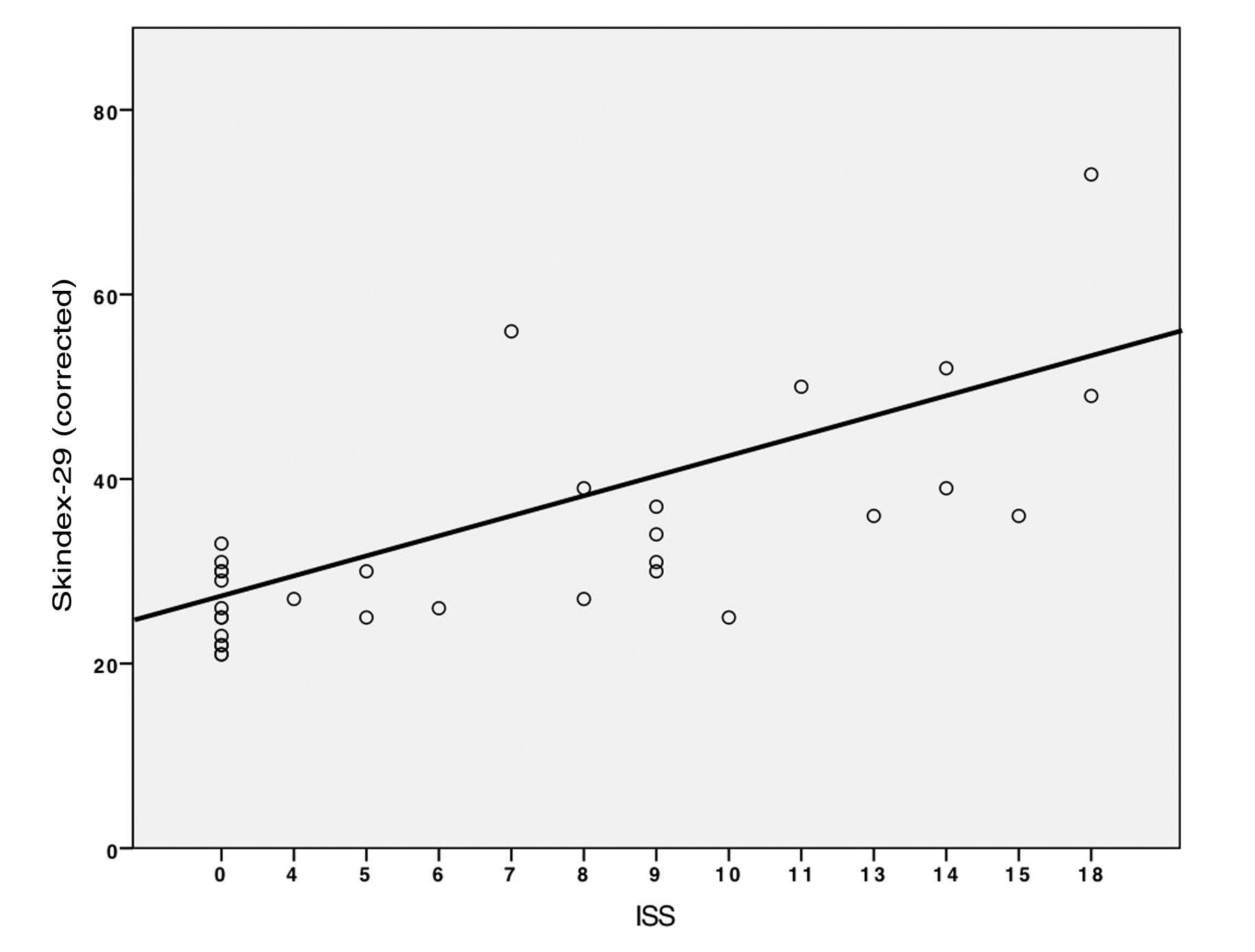
Finally, the relationship between Skindex-29 and ISS scores was analyzed using linear regression (Fig. 1). It was observed that for every increase in the ISS score, Skindex-29 increased by 1.14 points (p<0.001; R=0.721).
DiscussionIn this study, several factors associated with a poorer quality of life in patients with PCLs were found, such as age, the number of previous treatments received, or the presence of pruritus. The variety of questionnaires used in the literature to assess QOL in PCL patients complicates the comparison of obtained data, in addition to the fact that most studies focus on QOL in CTCL patients,6–14 with very few including all types of PCLs.5,15,16 Despite this, we observed that older patients had a higher DLQI score, and thus a greater impact on their QOL, which is consistent with former studies.5,6,16 Other factors classically associated with poorer QOL in PCL patients such as female sex, Black patients, advanced disease stages, SS, psychiatric comorbidity, or type of treatment4,7 were not found in our study, probably due to the inclusion of all PCL types (not just MF/SS); the small sample size; and the absence of patients with SS or from different ethnic/racial groups.
On the other hand, the study found more cases of severe Skindex-29 in patients with >2 previous treatments. It has been reported that treatment with corticosteroids or interferon is associated with a poorer QOL,5 mainly due to its association with anxiety and depression. However, the association between the number of previous treatments and severe cases in Skindex-29 has not been described in the literature to this date. This association can be interpreted as patients who have been treated with >2 treatments having a worse QOL, since for them the use of different therapeutic measures has not been effective, and therefore their impairment is greater as clinical control of the disease has not been achieved. This is, therefore, an important piece of data to consider in the clinical and therapeutic management of these patients.
Although our study found no association between QOL and HADS, the results show that probably up to 5 patients could have been diagnosed with anxiety, and up to 2 with depression. This fact is of great importance, as numerous studies emphasize the impact on PCL patients not only physically, but also emotionally, economically, and functionally, which negatively influences their QOL.9–11 A recently published study shows the cost of treatment and care for PCL patients in Spain,17 reflecting the economic component of the disease, especially in countries where patients bear the costs.
The main finding of our study is that the presence of pruritus is associated with higher scores on Skindex-29, DLQI, WHO-5, and HADS, in both the anxiety and depression subscales. Furthermore, a positive association was observed between ISS and Skindex-29 values. Pruritus was therefore the most debilitating symptom and the one most associated with a decrease in QOL as measured by the different questionnaires in the study, which is consistent with current studies,4,5,18 where pruritus is described by patients as the most frequent symptom and the one that most affected their daily lives, interfering with sleep and being associated with a great impact on QOL. This symptom is common in PCLs, but it is more frequent in CTCLs, where worsening pruritus is associated with disease progression, relapse, or infection, making its therapeutic management especially important to improve patients’ QOL.19 In accordance with published literature, in our study, pruritus affected CTCL patients more, with only 1 patient with CBCL complaining of this symptom, so in this group, the impact on their QOL could be due to different causes.
Finally, no differences in QOL were found between MF and other PCLs across the different questionnaires used. We believe this is due to the underrepresentation of non-MF PCLs in the sample. Some studies suggest that CTCLs have worse QOL vs CBCLs15; even so, this is an understudied area where more research is needed to clarify this issue.
The main limitations of the study were its cross-sectional design, which means that causal associations cannot be established due to lack of follow-up; the small sample size, with a small proportion of non-MF PCLs; and the lack of a control group.
In conclusion, our study demonstrates that patients with PCLs experience an impact on their QOL, with pruritus being the most limiting factor in this regard. Since all that has been stated previously, and considering the chronic nature of this disease, along with the lack of a curative treatment, and the impact on QOL suffered by patients, the development of a specific questionnaire for PCLs remains of paramount importance.
Ethical considerationsThis study was approved by the Provincial Ethics Committee for Research of Granada, in full compliance with the Declaration of Helsinki. Informed consent was obtained from participants, either verbally or in writing. The confidentiality of participant data was rigorously preserved, with an anonymous database used for analysis.
FundingNone declared.
Conflicts of interestNone declared.