Reports show that between 25% and 78% of patients with anogenital dermatitis have positive patch test results. Consequently, patch testing would appear to be warranted in patients presenting with eczema in the anogenital region. The objectives of the present study were to identify the most common allergens in patients with perianal eczema and to determine which allergen series are most useful for patch testing in patients with this condition.
Material and methodsWe performed a retrospective review of patch test results in patients with only perianal eczema between 2001 and 2012.
ResultsOf the 37 patients with perianal eczema, 16 had a positive reaction; methylchloroisothiazolinone/methylisothiazolinone was the main allergen involved. With the exception of 1 case of sensitization to gentamicin, all the positive results with present relevance were to allergens from the standard series of the Spanish Contact Dermatitis and Skin Allergy Research Group (GEIDAC) or to the patient's own products.
ConclusionsIn our experience, methylchloroisothiazolinone/methylisothiazolinone is the main allergen involved in perianal eczema, and sensitization often results from using wet wipes. Patch testing in perianal eczema should be based on the GEIDAC standard series and the patient's own products.
La prevalencia de parches positivos en los pacientes afectados por una dermatitis anogenital oscila según las series entre un 25-78%, justificándose por tanto la realización de pruebas epicutáneas ante eczemas de esta localización. Los objetivos del presente estudio son por un lado determinar los alérgenos más frecuentes en los pacientes con eczema perianal y, por otro, establecer las baterías de alérgenos más útiles para el estudio con pruebas epicutáneas de esta afección.
Material y métodosSe han revisado retrospectivamente (años 2001-2012) los resultados obtenidos al estudiar con pruebas epicutáneas a aquellos pacientes que presentaban exclusivamente un eczema perianal.
ResultadosDe los 37 pacientes con esta clínica en 16 se observó alguna reacción positiva, siendo el metil-cloroisotiazolinona/metilisotiazolinona el principal alérgeno implicado. Excepto un caso con sensibilización a gentamicina, todas las positividades con relevancia presente correspondieron a alérgenos de la batería estándar del Grupo Español de Investigación en Dermatitis de Contacto y Alergia Cutánea (GEIDAC) o a productos propios del paciente.
ConclusionesEn nuestra experiencia la metilcloroisotiazolinona/metilisotiazolinona es el principal alérgeno implicado en los eczemas perianales, procediendo esta sensibilización frecuentemente del uso de toallitas higiénicas. El estudio epicutáneo de un eczema perianal deberá realizarse básicamente con la batería estándar y los productos propios.
The term perianal eczema encompasses a series of inflammatory diseases affecting the anal region, of which eczema—of various etiologies—is the most common.1,2 Despite numerous publications on the prevalence of positive patch test results in patients with anogenital dermatitis, the literature contains practically no specific results for patch tests in patients with only perianal eczema.3
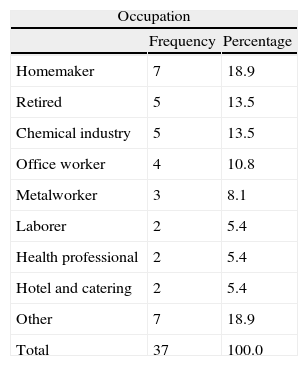
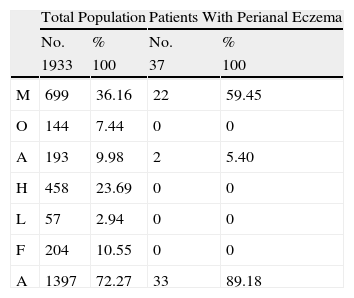
Material and methodsWe performed an observational retrospective study to identify the most common allergens in patients with perianal eczema and to determine which allergen series are most useful for patch testing in patients with this condition. We analyzed the results of patch testing in all patients with perianal eczema studied at the Contact Allergy Unit of the Dermatology Department of Hospital Universitario Araba (Sede Santiago), Vitoria-Gasteiz, Spain between January 2001 and June 2012. During this time, 1933 patients underwent patch testing; 37 had only perianal eczema (1.91%). The mean age of the 37 patients was 56.6 (37-82) years; 22 were men (59.5%) and 15 were women (40.5%). Two patients reported a history of atopic dermatitis and 6 reported other atopic diseases. The most common profession was homemaker (Table 1). Table 2 shows the MOAHLFA index for the total study population and for the patients with only perianal eczema.
MOAHLFA Index of the Study Group and of the Group of Patients With Only Perianal Eczema.
| Total Population | Patients With Perianal Eczema | |||
| No. | % | No. | % | |
| 1933 | 100 | 37 | 100 | |
| M | 699 | 36.16 | 22 | 59.45 |
| O | 144 | 7.44 | 0 | 0 |
| A | 193 | 9.98 | 2 | 5.40 |
| H | 458 | 23.69 | 0 | 0 |
| L | 57 | 2.94 | 0 | 0 |
| F | 204 | 10.55 | 0 | 0 |
| A | 1397 | 72.27 | 33 | 89.18 |
Abbreviations: M, male; O, occupation (occupational disease); A, atopy (patients with atopic eczema); H, hand (patients with hand eczema); L, leg (patients with leg eczema); F, face (patients with facial eczema); A, age >40 years.
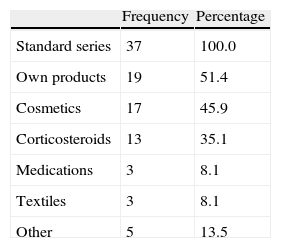
All patients underwent patch testing with the standard series of the Spanish Contact Dermatitis and Skin Allergy Research Group (GEIDAC) (True Test, MEKOS Laboratories ApS and additional allergens from Chemotechnique Diagnostics) and, depending on the clinical history, with specific test series and the patients’ own products (Table 3). It is noteworthy that only 1 test series was used in 3 patients with perianal eczema, whereas 3 series were used in 48.6%. Readings were taken at 48 and 96hours according to the recommendations of the International Contact Dermatitis Research Group.4 The relevance of positive results was established after checking the clinical history to ascertain whether the eczema had improved or resolved after avoidance of the allergens involved.
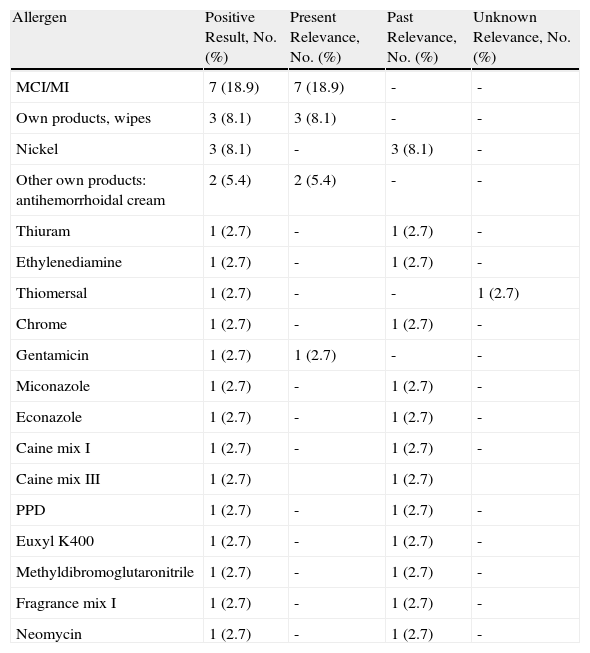
ResultsOf the 37 patients with perianal eczema, 16 had a positive reaction (43.24%), and relevance was present in 10 cases (27.02%) (Table 4). The most common positive allergen with present relevance was methylchloroisothiazolinone/methylisothiazolinone (MCI/MI) (n=7) followed by the patients’ own products (n=5; 3 by wet wipes and 2 by topical antihemorrhoidal products). The 3 patients with positive reactions to the wet wipes had positive patch test results to MCI/MI, which was shown to be a component of the wipes. Of the 2 cases of eczema caused by topical antihemorrhoidal products, one was caused by a commercial cream (Proctolog) and the other by a cream prepared by a naturopath. The patient who was allergic to the commercial cream also had positive results with caine mix I (procaine 1%, dibucaine 2.5%) and caine mix III (benzocaine 5%, dibucaine 2.5%, tetracaine 2.5%): relevance was interpreted as past, since none of these allergens are ingredients of the product. The other patient with a positive result to antihemorrhoidal cream did not report any associated positive reactions.
Positive Results Obtained and Their Relevance in Patients With Perianal Eczema.
| Allergen | Positive Result, No. (%) | Present Relevance, No. (%) | Past Relevance, No. (%) | Unknown Relevance, No. (%) |
| MCI/MI | 7 (18.9) | 7 (18.9) | - | - |
| Own products, wipes | 3 (8.1) | 3 (8.1) | - | - |
| Nickel | 3 (8.1) | - | 3 (8.1) | - |
| Other own products: antihemorrhoidal cream | 2 (5.4) | 2 (5.4) | - | - |
| Thiuram | 1 (2.7) | - | 1 (2.7) | - |
| Ethylenediamine | 1 (2.7) | - | 1 (2.7) | - |
| Thiomersal | 1 (2.7) | - | - | 1 (2.7) |
| Chrome | 1 (2.7) | - | 1 (2.7) | - |
| Gentamicin | 1 (2.7) | 1 (2.7) | - | - |
| Miconazole | 1 (2.7) | - | 1 (2.7) | - |
| Econazole | 1 (2.7) | - | 1 (2.7) | - |
| Caine mix I | 1 (2.7) | - | 1 (2.7) | - |
| Caine mix III | 1 (2.7) | 1 (2.7) | ||
| PPD | 1 (2.7) | - | 1 (2.7) | - |
| Euxyl K400 | 1 (2.7) | - | 1 (2.7) | - |
| Methyldibromoglutaronitrile | 1 (2.7) | - | 1 (2.7) | - |
| Fragrance mix I | 1 (2.7) | - | 1 (2.7) | - |
| Neomycin | 1 (2.7) | - | 1 (2.7) | - |
Abbreviations: MCI/MI, methylchloroisothiazolinone/methylisothiazolinone; PPD, paraphenylenediamine.
The patients became sensitized to MCI/MI by using wet wipes in 4 cases and other cosmetic products in 3 cases. Of the 4 patients who were allergic to MCI/MI and sensitized by wet wipes, 3 underwent patch testing with their own wipe. The remaining patient did not have wipes but was able to provide a container on which MCI/MM was stated to be a component.
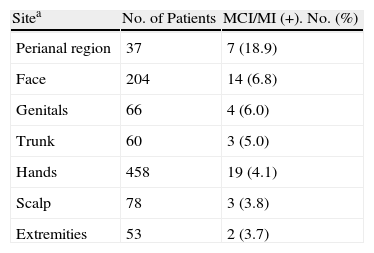
The prevalence of sensitization to MCI/MI in patients with perianal involvement (18.9%) was much higher than that obtained for all the patients who underwent testing (3.8%) and that recorded at the other anatomical sites (Table 5).
Number of Positive Results and Percentage for MCI/MI by Anatomical Site, January 2001 to June 2012.
| Sitea | No. of Patients | MCI/MI (+). No. (%) |
| Perianal region | 37 | 7 (18.9) |
| Face | 204 | 14 (6.8) |
| Genitals | 66 | 4 (6.0) |
| Trunk | 60 | 3 (5.0) |
| Hands | 458 | 19 (4.1) |
| Scalp | 78 | 3 (3.8) |
| Extremities | 53 | 2 (3.7) |
Abbreviation: MCI/MI, methylchloroisothiazolinone/methylisothiazolinone.
aSites less frequently sensitized by MCI/MI have been omitted, as have patients in whom several sites were affected simultaneously.
We did not observe positive results with present relevance to other preservatives, caines, balsam of Peru, or perfumes. Except for sensitization to gentamicin, all the positive results with present relevance were with allergens from the standard GEIDAC series or the patient's own products. The confirmed diagnoses were perianal irritant contact dermatitis in 25 patients (67.5%), perianal allergic contact dermatitis in 10 patients (27%), and mixed irritant and allergic contact dermatitis in 2 patients (5.4%).
DiscussionSeveral authors have warned about the worrying increase in sensitization to MCI/MI during the last few years, probably owing to increased use of MI in the cosmetic industry and the high authorized concentration of this preservative.5,6 Our experience is consistent with this observation, since the number of positive patch test results to MCI/MI has grown from 1.02% of all positive results in 2002 to 6.47% in 2012 (unpublished data).
The possibility of allergic contact dermatitis in the anogenital region caused by the MCI/MI in wet wipes has been reported in several publications.6–8 However, the results of patch testing in series of patients with anogenital dermatitis are disparate and do not point to MCI/MI as the main allergen. Bauer et al.3 recently reported their results after studying 1031 patients with anogenital skin complaints. In the 531 patients with perianal involvement, the most common positive allergens were bufexamac, fragrance mixes I and II, and methyldibromo glutaronitrile. Similarly, the North American Contact Dermatitis Group did not mention MCI/MI as one the main allergens involved in anogenital dermatitis. This group found that the statistically significantly most frequent allergens affecting the anogenital area were cinnamic aldehyde, dibucaine, benzocaine, hydrocortisone 17-butyrate, and budesonide.1 Other authors have also pointed to topical medications, especially, anesthetic drugs and corticosteroids, as the most common allergens at this site, given the widespread use of topical preparations with this composition by patients with anal pruritus and hemorrhoids.3,9–11 In our series, only 1 patient had a positive patch test result with topical anesthesia, and no patients had a positive result to topical corticosteroids. The patient who had positive patch test results with topical anesthetics (caine mixes I and III) was the same one who had a positive allergic response to the commercial antihemorrhoidal cream (Proctolog), which does not contain anesthetics. The patient in question had previously used other antihemorrhoidal products, which led to sensitization (past relevance).
Vermaat et al.12 reported that various spices and condiments were involved in anogenital allergic contact dermatitis and proposed that patients should be studied with the standard European series and additional series containing spices and condiments. In contrast with the findings of other studies,13 the authors stated that a negative result with balsam of Peru and colophony does not rule out sensitization to spices and condiments. None of the patients in our series had a positive reaction to balsam of Peru or colophony.
Our results are more consistent with those of Kränke et al., 14 who concluded that patch tests in this type of patient are only useful if the patient's own products are tested. Only 1 of the 37 patients in our series had a positive result with present relevance (gentamicin), which would not have been diagnosed using the standard GEIDAC series or the patient's own products.
An unusual finding in our study was that none of the patients with perianal eczema who were sensitized to MCI/MI in wet wipes had hand eczema, considering that the hands necessarily came into contact with the wipes. As is the case with other allergens (paraben paradox), this is probably because the patients became sensitized and then developed allergic eczema due to contact with MCI/MI on previously inflamed perianal skin but not on the skin of the hands.
In conclusion, we recommend performing patch tests in patients of this type with the standard GEIDAC series and the patient's own products, since the main allergen involved in our series was the MCI/MI present in wet wipes. It will be necessary to analyze larger patient series, both to determine with greater statistical significance the most common positive allergens in persons affected by this condition in our setting and to establish the possible implication of allergens that are generally not tested, especially spices and condiments.
Ethical DisclosuresProtection of persons and animals:The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed their hospital's protocol on the publication of data concerning patients and that all patients included in the study have received sufficient information and have given their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare that no private patient data are disclosed in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: González-Pérez R, Sánchez-Martínez L, Piqueres Zubiaurrre T, Urtaran Ibarzábal A, Soloeta Arechavala R. Pruebas epicutáneas en pacientes con eczema perianal. Actas Dermosifiliogr. 2014;105:694–698.