On 20 March 2020, lockdown was decreed in Argentina due to the Coronavirus disease 2019 (COVID-19) pandemic.1 We proposed examining the behavior of patients and of dermatologists in relation to their patients undergoing immunomodulating/immunosuppressant treatment.
We performed a cross-sectional study using 2 questionnaires. The first questionnaire, which was aimed at patients with inflammatory skin disease susceptible to immunomodulating/immunosuppressant treatment (psoriasis [Ps], atopic dermatitis [AD], hidradenitis suppurativa [HS], and others), consisted of 5 questions on age, dermatologic disease, current treatment, sources of information regarding COVID-19, and preventive measures. The questionnaire was sent to 1500 patients of the Civil Association for Psoriasis Patients (AEPSO). The second questionnaire, which was aimed at dermatologists, consisted of 12 questions on communication routes and patient care, sources of information, and behavior regarding treatments. The questionnaire was sent to 350 dermatologists of the Argentinian Psoriasis Society (SOARPSO) and the Argentinian Dermatology Society (SAD). Both questionnaires were sent via WhatsApp or e-mail on 19 March 2020. Responses were accepted up to March 27, 2020. Qualitative variables were expressed as absolute numbers and percentages. The STATA (StataCorp, version 14.2) statistical software package was used to perform the statistical analysis. The study complied with the ethical principles of the Helsinki declaration.
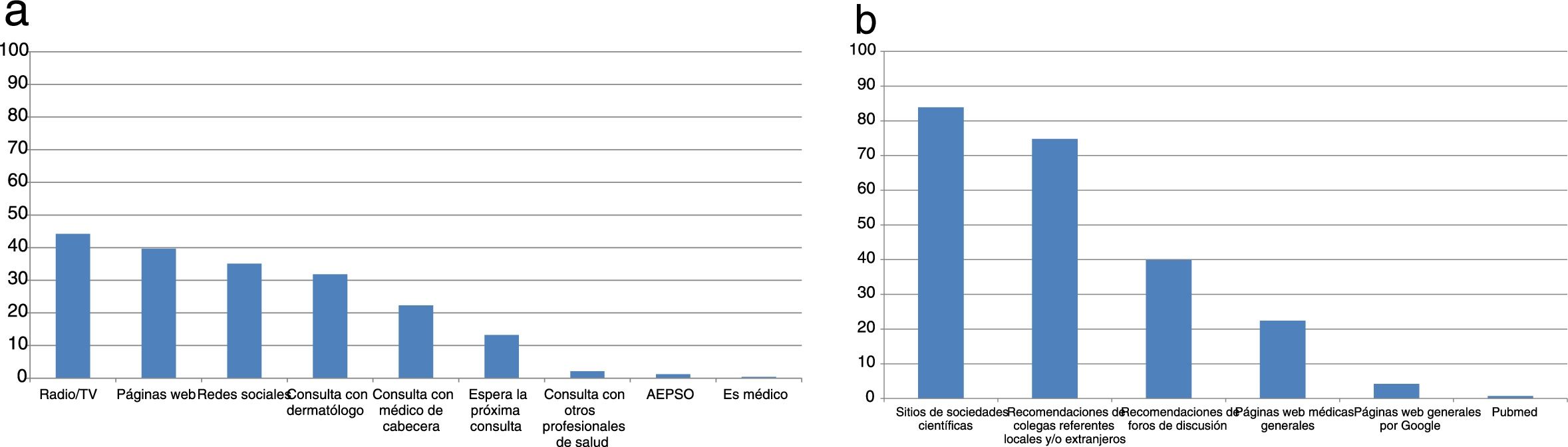
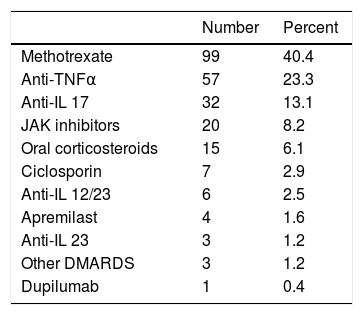
Of the 504 patients who responded, 81.9% had Ps, 8.9% had AD, and 4.2% had HS. A total of 88.6% of patients were between 18 and 60 years old. Forty-nine percent (245) were undergoing immunomodulatory/immunosuppressant treatment (Table 1). The most commonly used sources of information were radio and television (44.2%) and websites (39.7%) (Fig. 1a). The most frequent preventive measures were handwashing (95.1%), use of hand sanitizer (73.1%), and keeping social distance (62.9%). Although 28.2% self-isolated because they belonged to an at-risk group, 62.5% decided to self-isolate prior to the official declaration. Twelve percent of patients suspended immunomodulating/immunosuppressant treatment without consulting their physician.
Immunomodulating/Immunosuppressant Treatments.
| Number | Percent | |
|---|---|---|
| Methotrexate | 99 | 40.4 |
| Anti-TNFα | 57 | 23.3 |
| Anti-IL 17 | 32 | 13.1 |
| JAK inhibitors | 20 | 8.2 |
| Oral corticosteroids | 15 | 6.1 |
| Ciclosporin | 7 | 2.9 |
| Anti-IL 12/23 | 6 | 2.5 |
| Apremilast | 4 | 1.6 |
| Anti-IL 23 | 3 | 1.2 |
| Other DMARDS | 3 | 1.2 |
| Dupilumab | 1 | 0.4 |
Abbreviations: Anti-TNFɑ indicates tumor necrosis factor ɑ inhibitor; anti-IL 12/23, interleukin 12 and 23 inhibitor; anti-IL 17, interleukin 17 inhibitor; anti-IL 23, interleukin 23 inhibitor; DMARDS, disease-modifying antirheumatic drugs; JAK inhibitor, Janus kinase enzyme inhibitor.
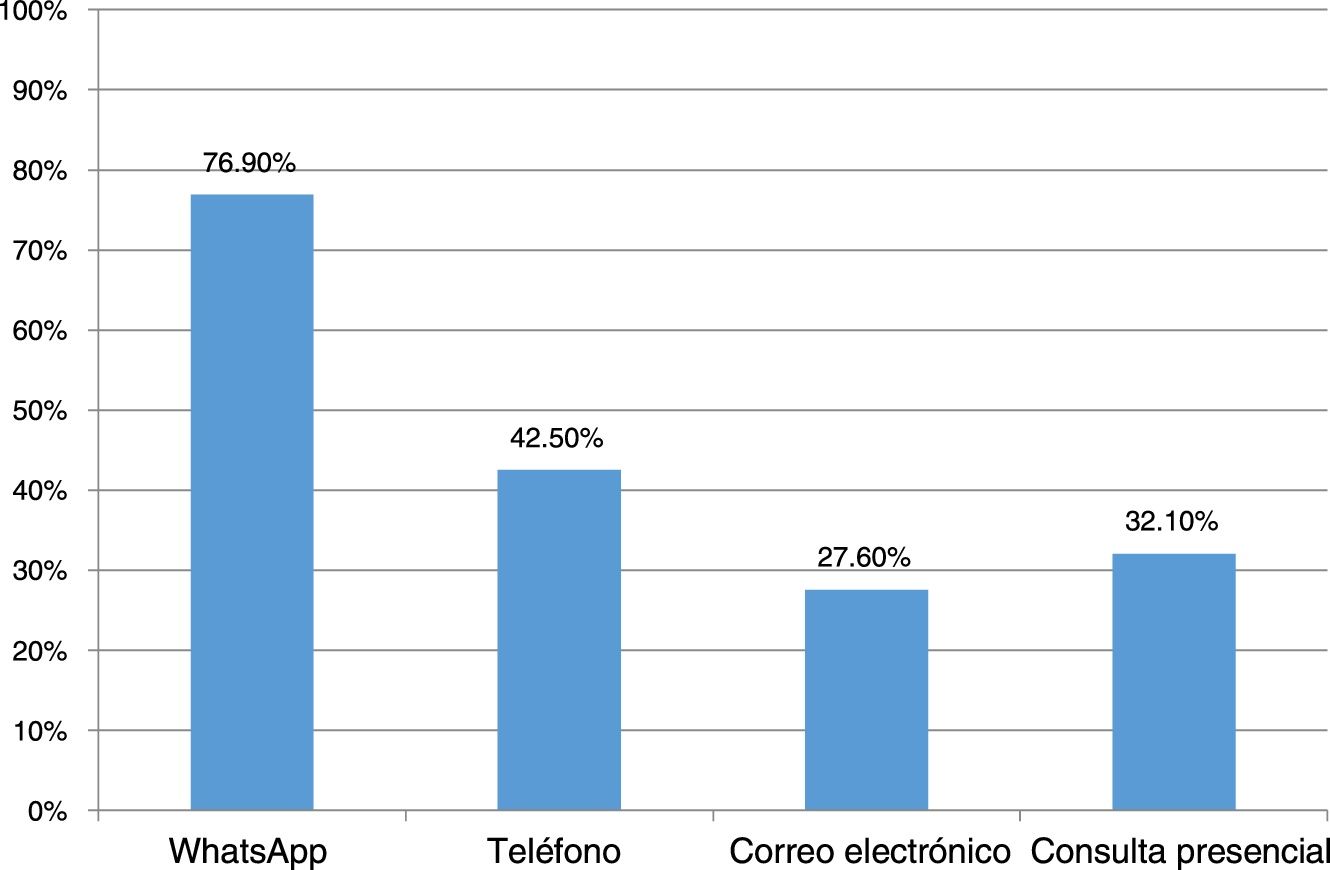
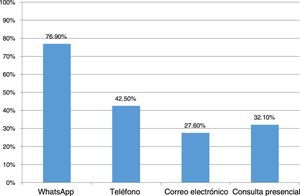
Responses to the survey were received from 146 dermatologists. In terms of sources of information, 83.9% consulted the websites of scientific societies and 74.8% followed the recommendations of noted colleagues (Fig. 1B). A total of 86% of the dermatologists were consulted by their patients for queries relating to COVID-19 (Fig. 2). In terms of in-person care, half of respondents suspended all visits, one-fifth spaced the visits out, and one-third saw only emergencies. Half of the physicians used electronic means for handling consultations (WhatsApp or e-mail). Although only 13% used telemedicine, 100% felt that it would be of use at this time. With regard to conventional immunomodulating/immunosuppressant treatment, 64.9% evaluated each case individually to define continuity, 25.7% only reinforced alarm guidelines, and 8.8% made no changes. In terms of biologic treatments, 78.8%, 17.4%, and 2.3% took the same measures, respectively. One dermatologist suspended conventional treatments and 2 suspended biologic agents.
Our study examined the behavior of patients and dermatologists at the start of the pandemic in Argentina. The fact that most patients had self-isolated before the health care authority issued the indication appears to be intuitively reasonable. However, future studies must determine its plausibility, as isolation may be impracticable in a context of poverty, overcrowding, and cessation of income.
This is the first pandemic to occur during the rise of information and communication technology, where the variety of easily accessible digital media and resources can generate a paradoxical effect of disinformation and inappropriate behavior. Hence the importance of the active role of dermatologists and scientific societies in the dissemination of appropriate information.2–4
Furthermore, the fact that both dermatologists and patients prefer virtual means of communication for visits highlights the need for mass implementation of telemedicine during the pandemic.5
We highlight the fact that the initial reflex of the dermatologists was not to systematically suspend immunomodulating/immunosuppressant treatment but to evaluate the risk-benefit relationship in each case.6–10 Mass suspension could lead to severe episodes requiring hospitalization at a time of relative scarcity of beds.
A strength of this study is that we believe it to be the first survey to examine the perspective of patients with dermatologic diseases undergoing immunomodulating/immunosuppressant treatment and that of dermatologists in the context of the COVID-19 pandemic. As limiting factors, we acknowledge selection and comprehension bias and missing data.
In conclusion, understanding the sources of information of patients and physicians in the event of a pandemic may be useful for improving communication strategies. Furthermore, due to the imposed social isolation, telemedicine is poised to be an essential tool for sustaining patient care.5
Conflicts of InterestThe authors declare that they have no conflicts of interest.
The authors would like to thank Silvia Fernández Barrio, chair of AEPSO, for her help with the dissemination of the survey.
Please cite this article as: Zimman S, Cura MJ, Lun PC, Echeverría CM, Mazzuoccol LD, Luna PC, Mazzuoccolo LD. Impacto de la pandemia COVID-19 en los tratamientos inmunomoduladores e inmunosupresores en dermatología: actitudes de los pacientes y los dermatólogos en Argentina. Actas Dermosifiliogr. 2020. https://doi.org/10.1016/j.ad.2020.04.004