Frontal fibrosing alopecia (FFA) is a scarring disease in which the hairline recedes and the eyebrows can be affected. Usually seen in postmenopausal women, FFA is much less common in men.
ObjectiveTo describe the clinical characteristics of FFA in a case series of men and compare this series to those reported in the literature.
Material and methodsMen with FFA being treated in our dermatology department from January 2010 to December 2015 were included prospectively for this descriptive study. We collected patient information and clinical and treatment characteristics.
ResultsTwelve men (mean age, 75 years) were recruited. Alopecia was the reason for seeking medical care in only 4 cases. The hairline had receded 3cm on average. Half the patients had facial papules, and 83% had androgenetic alopecia or hair loss on eyebrows or extremities. Follicular hyperkeratosis and erythema were present in 66%, and only 25% of the men reported pruritus. The most commonly prescribed treatments were topical: corticosteroids in 8 patients (66%) and minoxidil in 4 (33%).
ConclusionsFacial papules, androgenetic alopecia, and loss of body hair are more often observed in men with FFA than in women. The men in this series were older on average than in other FFA case series in the literature, possibly accounting for the higher prevalence of associated androgenetic alopecia and the fact that most of these men were seeking care for conditions other than hair loss.
La alopecia frontal fibrosante (AFF) es una alopecia cicatricial caracterizada por el retroceso de la línea de implantación del pelo, asociada a alopecia de cejas. Habitualmente afecta a mujeres en edad posmenopáusica, siendo mucho menos prevalente en varones.
ObjetivoDescribir las características clínicas de la AFF en los hombres estudiados y compararlos con los datos recogidos en la literatura.
Material y métodosSe realizó un estudio descriptivo de los varones diagnosticados de AFF en nuestro Servicio, desde enero del 2010 hasta diciembre del 2015. Se recogieron los datos demográficos, las características clínicas y los tratamientos realizados.
ResultadosSe reclutó a 12 pacientes. La edad media fue de 75 años. La alopecia fue el motivo de consulta únicamente en 4 pacientes. El retroceso medio de la línea de implantación del pelo fue de 3cm. Las pápulas faciales estaban presentes en el 50% de los hombres, el 83% presentaba alopecia de cejas, extremidades y alopecia androgenética (AGA). El eritema y la hiperqueratosis folicular se veían en el 66% de los casos y solo el 25% refería prurito. El tratamiento más frecuentemente utilizado consistió en corticoide tópico en 8 pacientes (66%), asociado a minoxidil tópico en 4 de ellos (33%).
ConclusionesSegún los datos obtenidos en nuestra serie, las pápulas faciales, la AGA y la afectación del vello corporal son más frecuentes en los hombres con AFF que en las mujeres. Por otra parte, a diferencia de los casos de AFF en varones descritos en la literatura, la edad media es mayor en nuestra serie, lo que podría explicar la mayor incidencia de AGA asociada y que la mayoría consulte por otro motivo.
Scarring alopecias are a set of conditions that lead to permanent hair loss due to the destruction of follicular stem cells.1,2
Frontal fibrosing alopecia (FFA) was described by Kossard3 in 1994 as a particular type of scarring alopecia affecting menopausal women.4 It is characterized by a receding frontotemporal hairline associated with varying degrees of eyebrow alopecia, facial papules, and occasionally hair loss in the axillas and on the pubis and extremities.5,6 There is a tendency to consider FFA a form of follicular lichen planus (FLP) that selects the frontotemporal hairline. The association between these 2 diagnoses is debated, however, because FFA usually affects older women and presents with a distinct pattern of hair loss; moreover, lichen planus patches are rarely present in other integumentary structures in individuals with FFA and histologic features differ slightly from those of FLP.7,8
Since the first description of FFA, hundreds of patients—usually women—have been described.9 Male FFA appears to be rare and only occasional cases have appeared in the literature.9–23 We think FFA in men may be more common than realized based on publications, however, because this condition can overlap or be confused with other types of baldness, especially androgenetic alopecia (AGA), for which men who have reached a certain age do not usually consult a physician if they consider it to be a normal part of the aging process.
We analyzed a prospectively recruited series of 12 men with FFA, one of the largest series published to date. We aim to describe the clinical and epidemiologic characteristics in the series and compare them to the largest series of FFA in women as well as to descriptions in men to date.
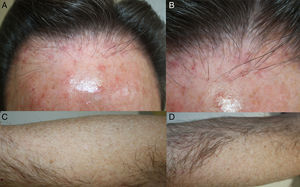
Material and MethodsWe conducted a prospective, descriptive, observational study of men with FFA diagnosed in the dermatology department of Hospital Universitario Donostia over a 5-year period between 2010 and 2015. Twelve patients were recruited (Table 1). Variables studied were age, time since onset of symptoms, the patient's reason for consulting a dermatologist, form of presentation (location; pruritus; erythema; perifollicular hyperkeratosis; alopecia in other areas of the skin; and presence of lichen planus patches on skin, nails or mucosal surfaces), trichoscopy, histology, presence of AGA, other concurrent diseases, treatments received, and response to treatments. We ordered a blood work-up that included analysis of thyroid hormones, antithyroid antibodies, and antinuclear antibodies for all patients. The inclusion criteria were as follows: 1) clinical: receding hairline (forehead or temple), with a band of paler skin with the appearance of scarring and absence of follicles, sometimes associated with eyebrow hair loss, erythema, and/or perifollicular hyperkeratosis; 2) trichoscopic: absence of follicles, white patches (scarring), and perifollicular erythema hyperkeratosis; and 3) histologic: lymphocytic inflammatory infiltrate usually located around the follicular infundibulum and isthmus, presence of apoptotic cells in the external root sheath, infundibular dilation and hypergranulosis, and residual fibrous tracts around the follicles. The exclusion criterion was the inability to distinguish between FFA or FLP, especially in patients with very advanced AGA in whom the hairline could not be evaluated. When the clinical diagnosis was in doubt (5 patients), it was confirmed histologically. The degree the hairline had receded was estimated at the forehead, temples, and nape of the neck by measuring the width of the band of bald, pale, atrophied skin without follicles.
Clinical Features of FFA in This 12-Patient Series.
| Patient No. | Age, y | Time Since Onset, y | Loss at Forehead | Loss at Temples | Loss at Nape | Eyebrow Alopecia | Loss on Limbs | Pruritus | Perifollicular Erythema | Perifollicular Hyperkeratosis | AGA (Hamilton Grade) | Reason for Visit |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 74 | 1 | 2cm | 1cm | No | No | Yes | Yes | + | + | Yes (II) | Scalp pruritus |
| 2 | 71 | 2 | ND | 4cm | 2cm | Yes | Yes | No | + | + | Yes (VI) | Alopecia |
| 3 | 77 | 5 | ≈ 5cm | 4cm | No | Yes | Yes | No | – | – | Yes (III) | Actinic keratosis |
| 4 | 82 | ? | 4cm | 3cm | No | Yes | Yes | No | – | – | No | Melanoma |
| 5 | 85 | 10? | ≈ 2cm | 2cm | No | Yes | Yes | No | – | – | Yes (V) | Actinic keratosis |
| 6 | 83 | ? | ND | 3cm | No | Yes | Yes | No | + | + | Yes (VI) | Basal cell carcinoma |
| 7 | 63 | 3 | ND | 4cm | No | Yes | Yes | No | + | + | Yes (VI) | Alopecia |
| 8 | 78 | 2 | ≈ 2cm | 2cm | No | Yes | Yes | Yes | + | + | Yes (VI) | Scalp pruritus |
| 9 | 80 | 4 | ND | 6cm | No | Yes | Yes | No | – | + | Yes (VII) | Basal cell carcinoma |
| 10 | 70 | 2 | ND | 3cm | No | Yes | No | No | + | + | Yes (VI) | Alopecia |
| 11 | 77 | 2 | ND | 4cm | No | Yes | No | No | + | + | Yes (VII) | Alopecia |
| 12 | 68 | 1 | 2cm | 0cm | No | No | Yes | Yes | + | – | No | Scalp pruritus |
| Seriesa | 75 | 2.5 | 3cm | 3cm | 8% | 83% | 83% | 25% | 66% | 66% | 83% | Alopecia: 33% |
Abbreviations: AGA, androgenetic alopecia; ND, not determined (underlying AGA prevented measurement of the receding band);?, patient unsure or unable to specify.
Patient characteristics and findings are summarized in Table 1.
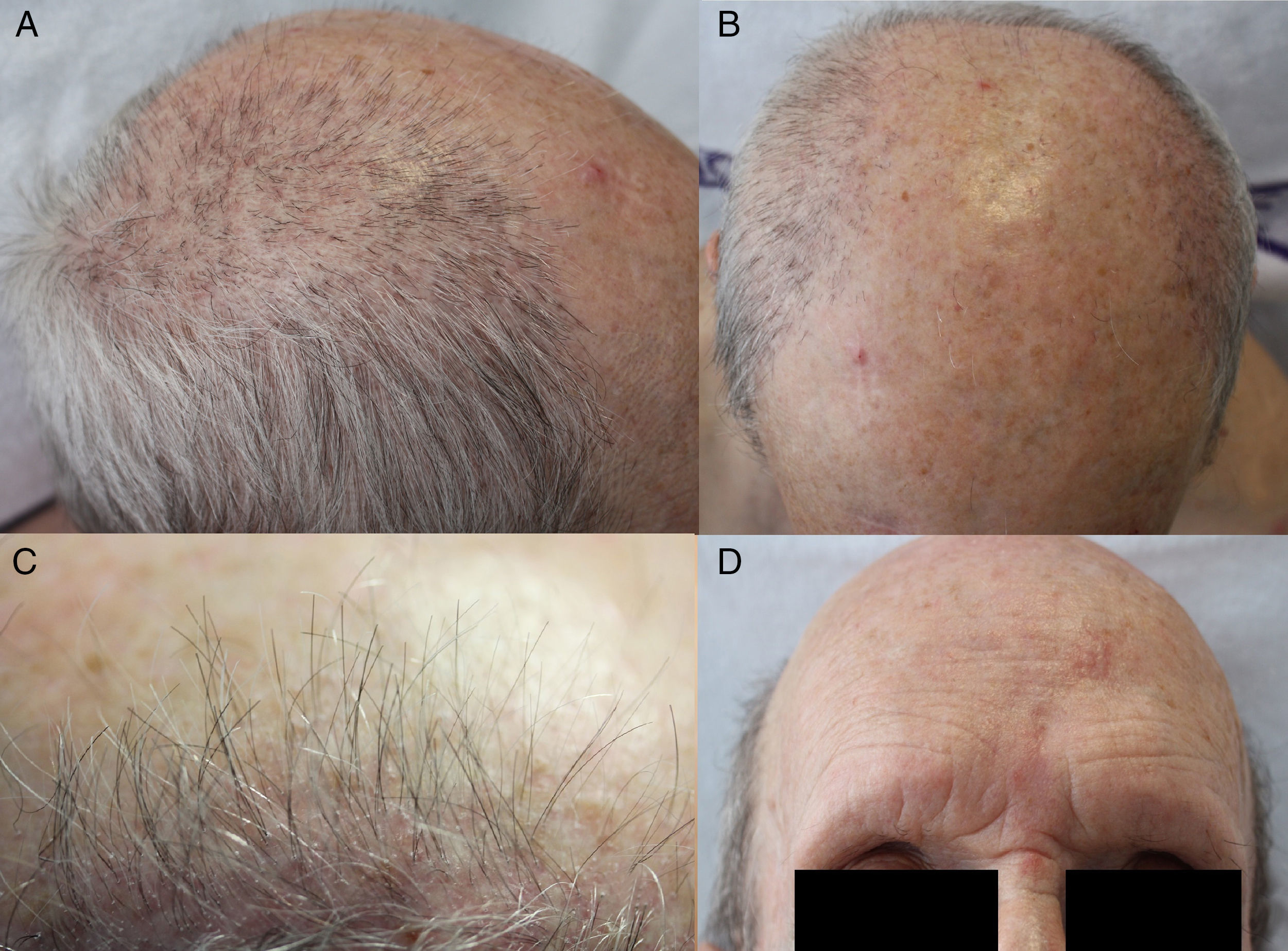
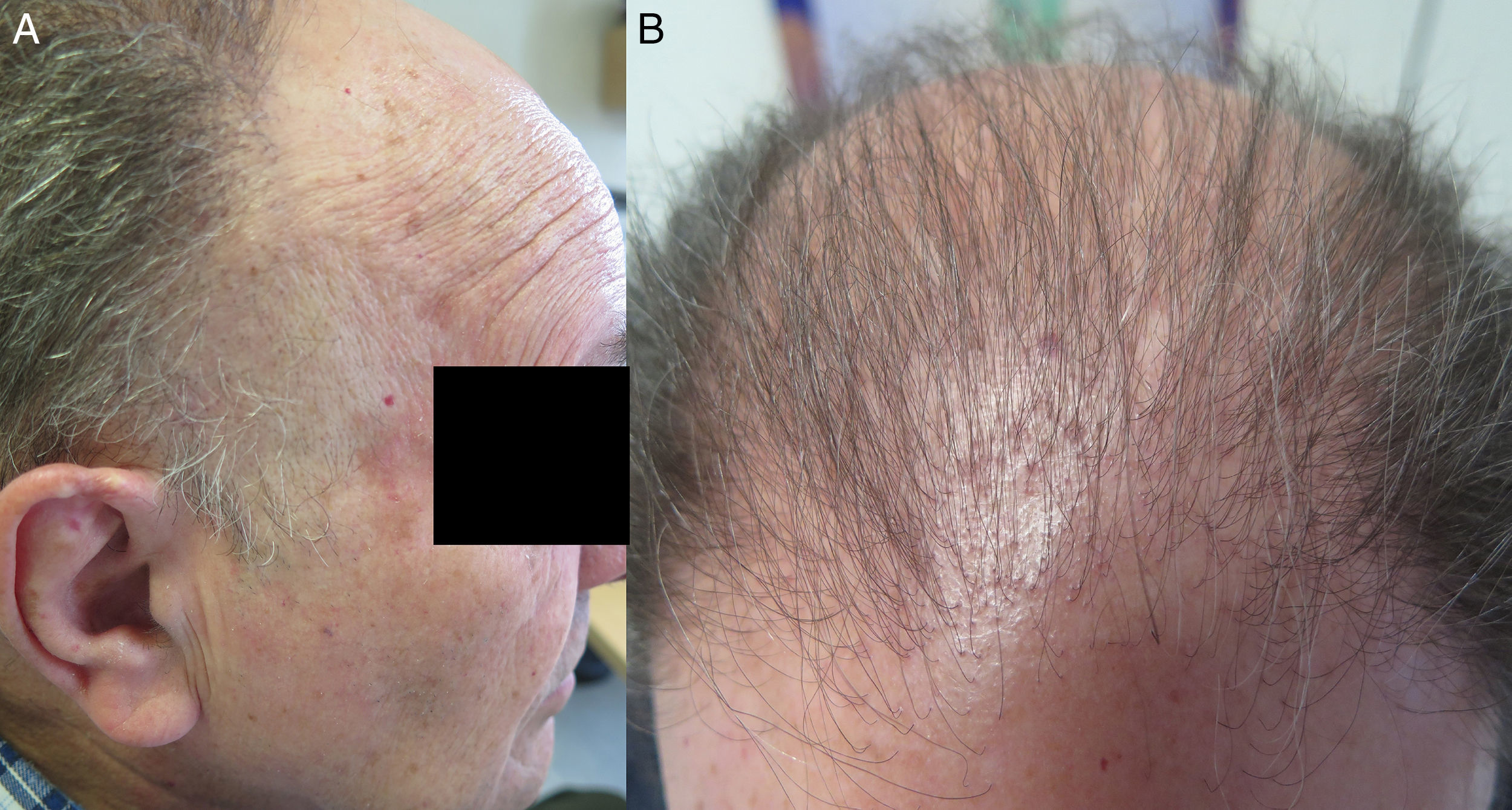
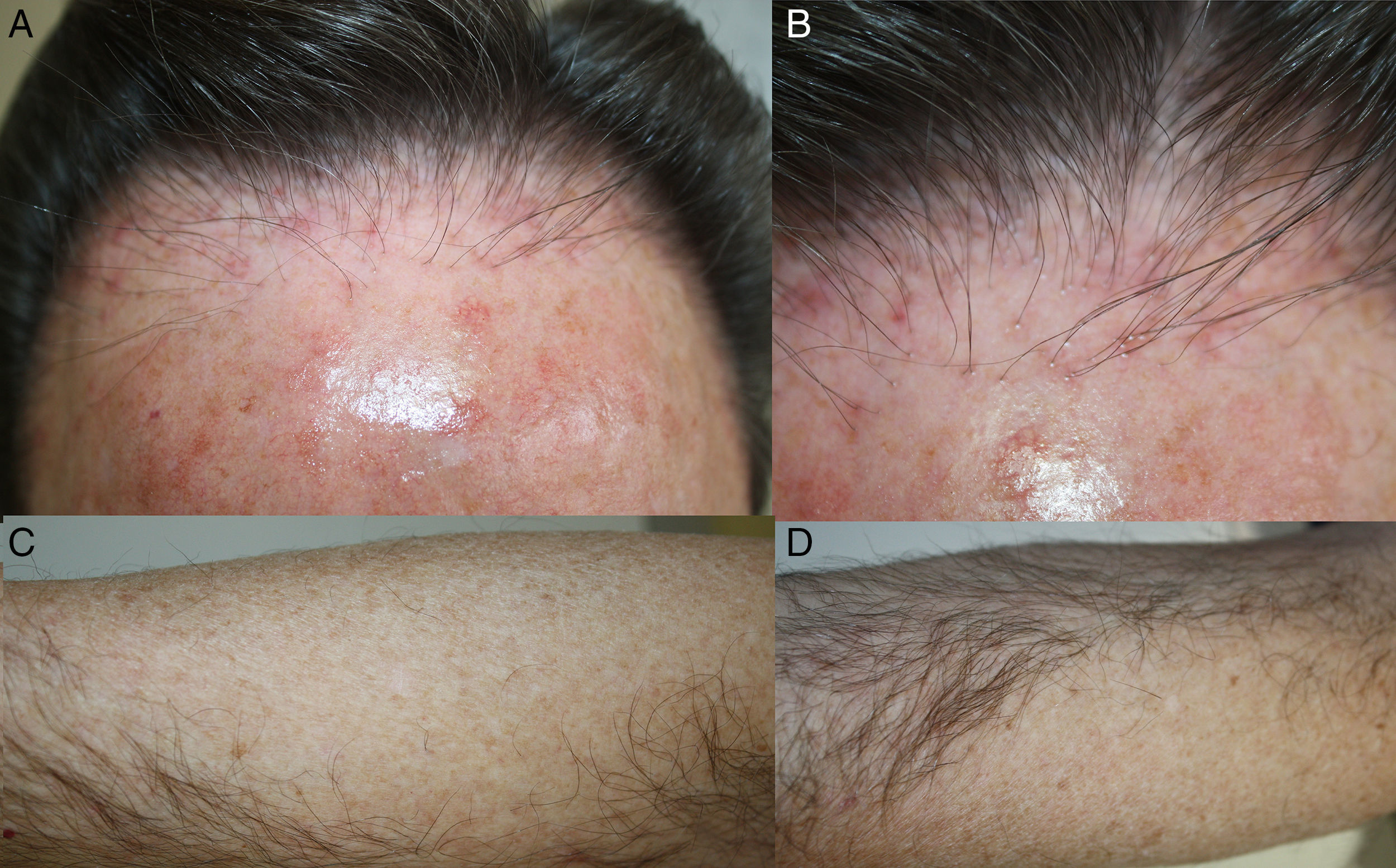
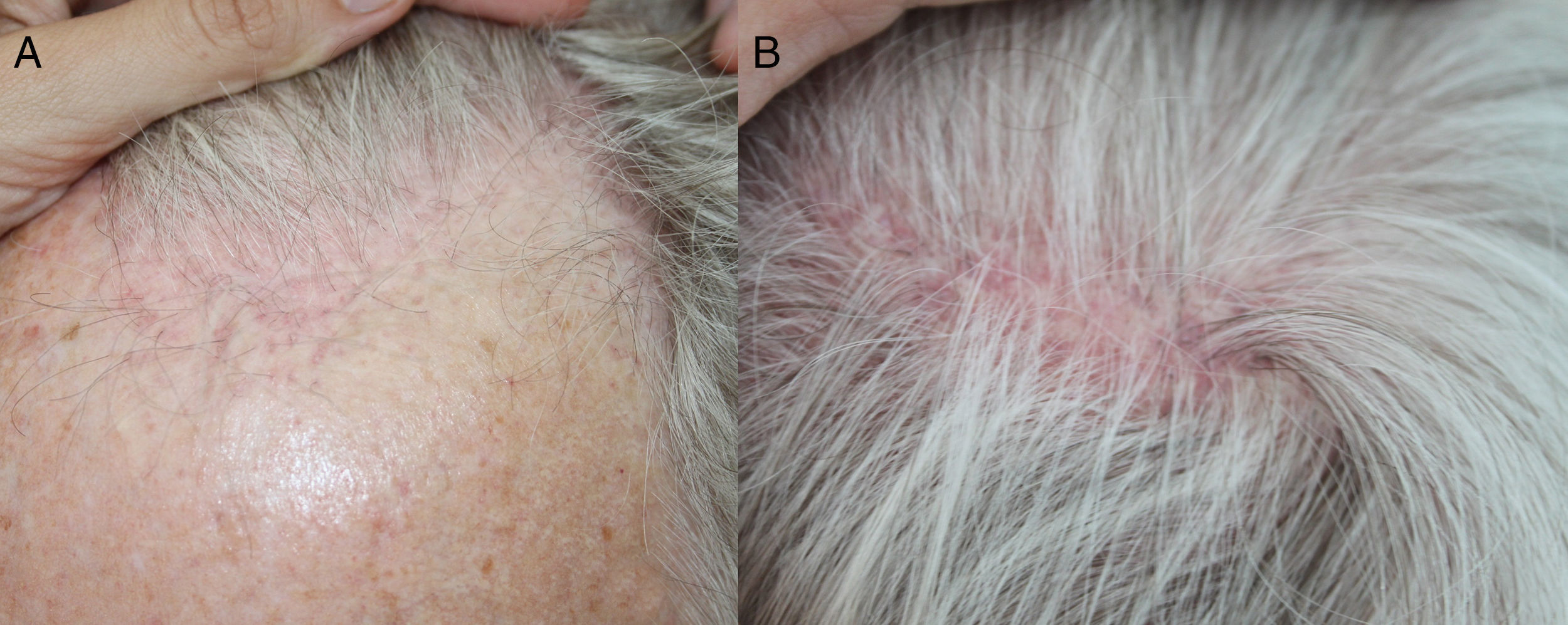
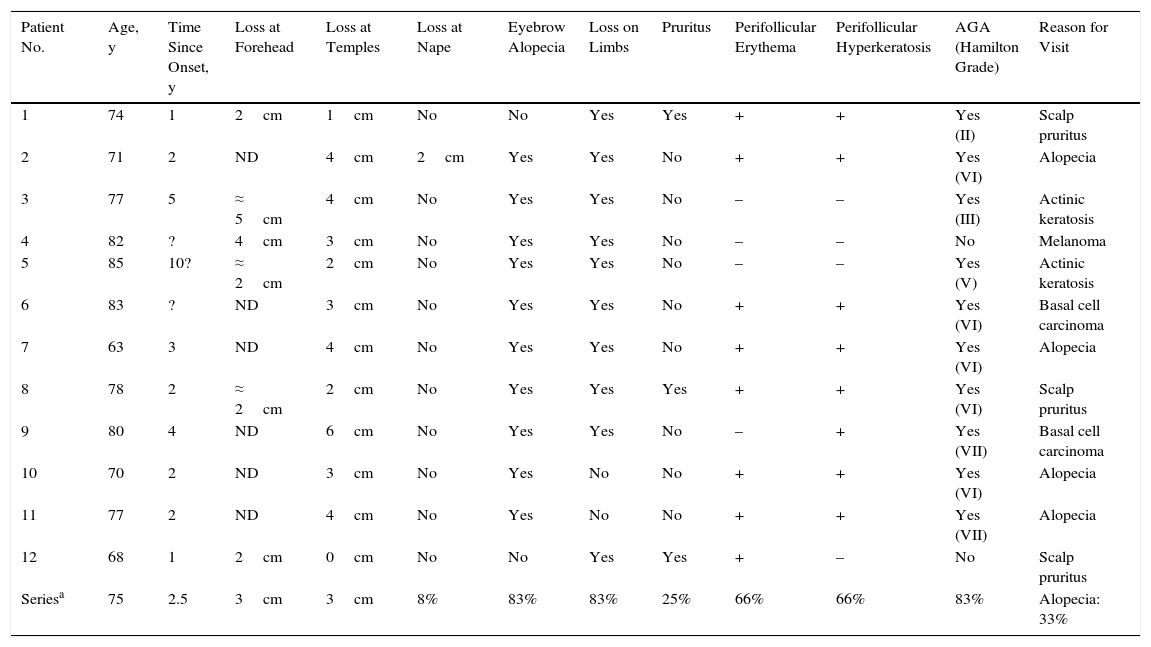
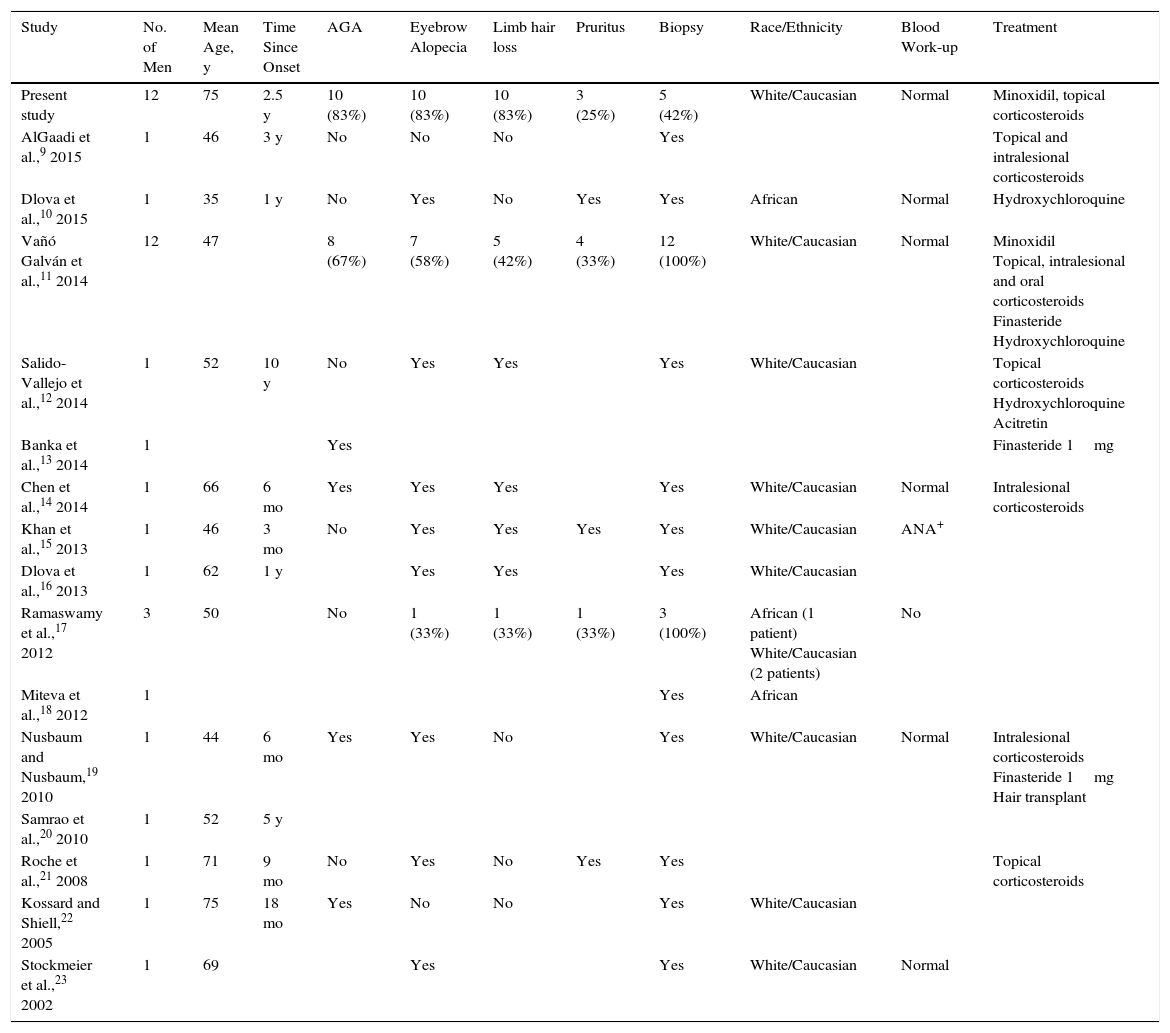
Ages ranged from 63 to 85 years (mean, 75 years). Only 4 patients had sought our care for baldness. Three others complained of an itchy scalp. FFA was an incidental finding in the remaining 5 patients, who required care for other conditions (mainly actinic keratosis and basal cell carcinoma). The hairline had receded from the forehead and temples in all patients, though baldness at the forehead could be attributed to FFA, AGA, or both, and from the nape of the neck in 1 patient (11%). The distance the hairline had receded ranged from 1to 6cm (mean, 3cm), although the band was sometimes difficult to measure if AGA was present (Figs. 1–4). A single patient had parietal scalp patches of scarring alopecia typical of FLP (Fig. 5). Erythema and perifollicular hyperkeratosis were observed in 8 patients (66%) and only 3 (25%) complained of itching. Eyebrow hair loss, which is very common in FFA, was found in nearly all our patients (n= 10, 83%), as was hair loss on forearms and legs (n= 10, 83%). Ten of these men (83%) also had AGA. Only 1 (8%) had facial (beard) alopecia. We observed facial papules in 6 (50%), although in some cases they were hardly visible. No lichen planus lesions were evident on skin, mucosal surfaces, or nails in any of the patients in this cohort; nor did we see generalized follicular keratotic papules. Dermoscopy showed an absence of follicles in all patients and perifollicular hyperkeratosis in 8 (66.6%), consistent with the clinical findings described above. Patients 2, 6, 7, 9, 10, and 11 (50%) had pale patches of scarring along with the yellow dots typical of AGA. Skin was biopsied only in the 5 patients (42%) whose diagnoses were in question. Histology revealed intense, concentric perifollicular fibrosis and varying degrees of lymphocytic inflammation in the epidermis between follicles. Four men (33%) underwent treatment with minoxidil 5% (patients 2, 7, 10, and 11) at night and topical betamethasone 17-valerate twice a week. They reported that disease stabilized with treatment. Patients 1, 6, 8, and 12 (33%) used topical corticosteroids occasionally, achieving control of itching, which was the symptom that concerned them. Another 4 patients (33%) declined treatment. A low antinuclear antibody titer (1:80) was found in only 1 blood work-up (8%). No indication of abnormal thyroid function was found in any patient. None reported using facial cosmetics or make-up bases with sunscreens. The most common concomitant conditions were high cholesterol levels (n=2, 17%) and high blood pressure (n=3, 25%). #OMIT# Two patients (17%) were on statins, 3 (25%) were on angiotensin-converting enzyme inhibitors, and 2 (17%) were on acetylsalicylic acid. Noteworthy in the history of 1 man (8%) was a diagnosis of autoimmune hepatitis 10 years earlier. He was treated with azathioprine and oral steroids. Another man had undergone a prostatectomy for prostate cancer 5 years before the onset of FFA.
FFA is considered a variant of FLP that tends to affect the area of the scalp at the frontotemporal hairline. A receding hairline at the forehead is a pattern of balding usually seen in postmenopausal women. Loss of eyebrow hair is highly characteristic, and nonscarring alopecia is often seen in the axillas, on arms, and on the abdomen. Patients with FFA do not usually report the pruritus typical of FLP, and erythema and perifollicular hyperkeratosis are usually less intense. The findings of histology overlap in FFA and FLP, although less follicular inflammation and more apoptotic cells are usually reported in FFA. An inflammatory infiltrate in the interfollicular epidermis of the scalp is occasionally seen in FLP but is very rare in FFA.8
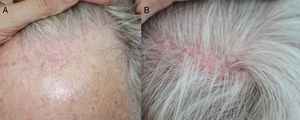
Most patients with FFA described are postmenopausal women. We found only 28 cases in men in the literature (Table 2). In all such cases, the patient had gone to the physician seeking treatment for FFA; in contrast, we enrolled men consulting us for other reasons. Pruritus was reported in 8 of the previously published cases in men (about 28%), a frequency that was similar to the 25% (n=3) in our study. Associated AGA was reported in 12 of the previously described cases in men (42%), a lower percentage than the 83% (n=10) in our series. Whereas the average age of men with FFA previously reported was 55 years, the average in our series was 75 years, possibly accounting for both the higher prevalence of associated AGA in our patients and the fact that they had not sought care for alopecia. Our patients were older on average because we enrolled men consulting us for other conditions (n=8, 66%; mean age, 78 years) as well as those specifically seeking care for FFA (n=4, 33%; mean age, 70 years. Conversely, the lower mean age in cases previously reported may be the result of describing only patients who complained of FFA, which probably concerns younger men more; in contrast FFA is usually an incidental finding in older men. One of our patients had concurrent FFA and FLP lesions, a finding that has not been described in men to our knowledge. It is important to examine the top of the scalp for signs of scarring alopecia to differentiate between FFA and FLP in men. In FFA, we can expect to find a hairless band receding from the original hairline at the forehead and/or temples; typically frontotemporal loss is associated with eyebrow loss. In FLP, we expect to see 1 or more bald patches at the crown, with perifollicular hyperkeratosis at the receding hairline.
Cases of FFA in Men Described in the Literature.
| Study | No. of Men | Mean Age, y | Time Since Onset | AGA | Eyebrow Alopecia | Limb hair loss | Pruritus | Biopsy | Race/Ethnicity | Blood Work-up | Treatment |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Present study | 12 | 75 | 2.5 y | 10 (83%) | 10 (83%) | 10 (83%) | 3 (25%) | 5 (42%) | White/Caucasian | Normal | Minoxidil, topical corticosteroids |
| AlGaadi et al.,9 2015 | 1 | 46 | 3 y | No | No | No | Yes | Topical and intralesional corticosteroids | |||
| Dlova et al.,10 2015 | 1 | 35 | 1 y | No | Yes | No | Yes | Yes | African | Normal | Hydroxychloroquine |
| Vañó Galván et al.,11 2014 | 12 | 47 | 8 (67%) | 7 (58%) | 5 (42%) | 4 (33%) | 12 (100%) | White/Caucasian | Normal | Minoxidil Topical, intralesional and oral corticosteroids Finasteride Hydroxychloroquine | |
| Salido-Vallejo et al.,12 2014 | 1 | 52 | 10 y | No | Yes | Yes | Yes | White/Caucasian | Topical corticosteroids Hydroxychloroquine Acitretin | ||
| Banka et al.,13 2014 | 1 | Yes | Finasteride 1mg | ||||||||
| Chen et al.,14 2014 | 1 | 66 | 6 mo | Yes | Yes | Yes | Yes | White/Caucasian | Normal | Intralesional corticosteroids | |
| Khan et al.,15 2013 | 1 | 46 | 3 mo | No | Yes | Yes | Yes | Yes | White/Caucasian | ANA+ | |
| Dlova et al.,16 2013 | 1 | 62 | 1 y | Yes | Yes | Yes | White/Caucasian | ||||
| Ramaswamy et al.,17 2012 | 3 | 50 | No | 1 (33%) | 1 (33%) | 1 (33%) | 3 (100%) | African (1 patient) White/Caucasian (2 patients) | No | ||
| Miteva et al.,18 2012 | 1 | Yes | African | ||||||||
| Nusbaum and Nusbaum,19 2010 | 1 | 44 | 6 mo | Yes | Yes | No | Yes | White/Caucasian | Normal | Intralesional corticosteroids Finasteride 1mg Hair transplant | |
| Samrao et al.,20 2010 | 1 | 52 | 5 y | ||||||||
| Roche et al.,21 2008 | 1 | 71 | 9 mo | No | Yes | No | Yes | Yes | Topical corticosteroids | ||
| Kossard and Shiell,22 2005 | 1 | 75 | 18 mo | Yes | No | No | Yes | White/Caucasian | |||
| Stockmeier et al.,23 2002 | 1 | 69 | Yes | Yes | White/Caucasian | Normal |
Abbreviations: AGA, androgenetic alopecia; ANA, antinuclear antibodies.
The cases we describe showed certain important differences from those of a series of 355 patients (including 12 men) analyzed by Vañó Galván et al.11 In that study, only 144 (40%) of the total presented with concurrent AGA (vs 83% in our series), 14% had facial papules (vs 50% in ours), and 24% showed hair loss in other parts of the body (vs 83% in ours). Fifteen percent of their patients had hypothyroidism, a finding that was absent in our series and also absent in the subgroup of 12 men they studied. However, we also saw similarities. Thirty-five percent of their patients reported pruritus (25% of ours), 15% had lost hair at the nape of the neck (8% of ours), and 80% had eyebrow alopecia (83% of ours). We might therefore speculate that AGA, facial papules, and hair loss on surfaces other than the scalp are more common in men than women with FFA. Focusing only on comparing our patients to their 12 men with FFA, we emphasize the similarly low prevalence of pruritus (33%) and the absence of hypothyroidism and elevated antinuclear antibody levels. However, the men studied by VañóGalvánetal. had lower prevalences of facial papules (33%), hair loss on other body surfaces (42%), and associated AGA (67%). Their patients were also younger than ours, possibly explaining the lower prevalence of AGA. Besides the fact that AGA would not have masked the FFA in their male patients, diagnosis would have been easier because their patients were seeking care for receding hairlines. VañóGalvánetal. considered that loss of body hair and the presence of perifollicular papules on the face were associated with a poor prognosis. We could therefore wonder whether FFA in men is associated with a worse outcome or if these features are present more often because onset of disease is earlier and the course is therefore longer (or their age more advanced, 75 years on average in our series). However, López-Pestañaetal.24 found facial papules more often in younger patients, either because they appear early in the course of disease or because they are easier to distinguish in patients whose skin has been less damaged by sun exposure. Hypothyroidism was not present in either our series or that of Vañó Galván et al., calling into question the hypothesis of an autoimmune mechanism in the pathogenesis of FFA. These findings may be attributable to small samples of men; in contrast, 15% of the total of 355 patients in the multicenter study of VañóGalvánetal. presented hypothyroidism.
Only 4 of our 12 patients consulted us about hair loss—a difference between our 5-year prospective series and the cases reported in the literature. We think FFA is underdiagnosed in men because many of them do not seek a medical opinion, probably for the following reasons: 1) itching, erythema, and perifollicular hyperkeratosis are not always present in FFA, so the receding hairline may go unnoticed, or 2) most men also develop AGA, which often includes hair loss at the forehead that masks the receding hairline. There is another basic reason why FFA may be noticed less in men than in women: AGA is the most common type of baldness in men, affecting 69.6% of the male population.25 The onset typically presents when a man is in his 40s with miniaturization of hair follicles beginning at the forehead and temples, causing the hairline to recede. Decreased density at the top of the head follows. Female pattern AGA presents later in women; 36% of women over the age of 80 years have this form of baldness.26 The area above the frontoparietal hairline is affected, but the hairline itself is maintained. Thus, the onset of AGA in women comes later and the hairline is usually preserved. Many men who have AGA probably take no notice of the onset of FFA, given that their hair was was already in the process of thinning near the hairline. Based on the literature we reviewed, we might infer that only 42% of men have both FFA and AGA9–23; in contrast, this association was present in 88% of our cohort. Because FFA is more noticeable in women, they consult dermatologists more often. Men, on the other hand, can be diagnosed only by means of thorough physical examination.
Although the etiology of FFA is unknown, the increased incidence in recent years suggests an environmental cause. A study by Aldoori et al.27 to explore possible risk factors for FFA suggested an association with the use of certain facial care products. Chemical sunscreens used in some products might be the culprits, but as none of our patients reported using cosmetics or sunscreens routinely, we cannot confirm such an association. It has also been suggested that genetic, hormonal, and autoimmune mechanisms may be implicated. None of the patients in our series had a family history of FFA or reported taking hormone treatments. However, the fact that one of our patients had a past history of autoimmune hepatitis requiring immunosuppression may support the involvement of autoimmune mechanisms. The presentation of FFA in men, and reports of improvement with 5-α-reductase therapy, indicate that androgens might play a role in triggering this disease.
Treating FFA is challenging because it is a scarring alopecia and most patients seek treatment in advanced stages of the condition. We treated only 4 of our patients, prescribing topical corticosteroids and minoxidil 5%. This approach controlled their FAA and associated AGA relatively well for a mean of 20 months of follow-up (range, 6–26 months). Both topical and intralesional corticosteroids can be used in the early stages of FFA, in addition to oral tetracyclines and antimalarial drugs to reduce inflammation and prevent secondary alopecia.28 5-α- reductase inhibitors block the follicular miniaturization typical of AGA, benefiting patients with both types of alopecia. Finasteride and dutasteride may be useful in some patients with FFA given that a hormonal component is a possibility.29 We did not prescribe these treatments for any of our patients, however, as they all declined oral medication. Hair transplants might also be a valid treatment choice, but FFA has recurred in most patients who have tried this approach.30
The limitations of our study are that we did not perform skin biopsies in all our patients and our sample was small. Larger studies are needed to confirm our findings.
ConclusionsFFA may be underdiagnosed in men, possibly because it causes few symptoms or is ignored because it is often found in association with AGA, which appears earlier than FFA in men. We therefore recommend thorough examination of the hairline in men. A diagnosis of FFA in a man who has consulted a dermatologist for another reason may be suggested by the presence of eyebrow hair loss; thin, pale skin at the hairline; perifollicular erythema; and occlusion of follicles. Trichoscopy can be useful for confirming the absence of follicles and pale patches of scarring.
We believe that hair loss in parts of the body other than face and scalp and the presence of facial papules may be more common in men with FFA than in women. We also emphasize the absence of hypothyroidism and FLP in our series. However, larger studies are needed to confirm these observations.
Ethical DisclosuresProtection of humans and animalsThe authors declare that no tests were carried out in humans or animals for the purposes of this study.
Confidentiality of dataThe authors declare that they have followed their insitutional protocols on publication of patient data.
Right to privacy and informed consentThe authors declare that no private patient data appear in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest
Please cite this article as: Ormaechea-Pérez N, López-Pestaña A, Zubizarreta-Salvador J, Jaka-Moreno A, Panés-Rodríguez A, Tuneu-Valls A. Alopecia frontal fibrosante en el varón: presentación de 12 casos y revisión de la literatura. Actas Dermosifiliogr. 2016;107:836–844.