We report the case of a 7 year-old boy who presented with a lesion on the left arm that had developed 2 years earlier and had suddenly increased in size in the preceding month. A Doppler ultrasound performed 1 month earlier revealed an echogenic mass of 1.6 × 1.7 × 1cm with posterior acoustic shadowing.
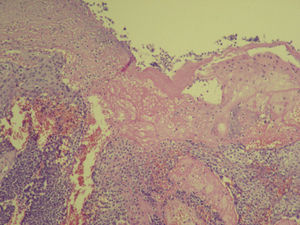
Examination revealed a stony-hard, exophytic, pedunculated tumor of 8cm in diameter on the patient's left arm. The overlying skin was absent, exposing an eroded surface and a bleeding tumor bed with a crater-like appearance (Fig. 1). Nuclear magnetic resonance imaging (MRI) and magnetic resonance angiography showed an exophytic formation consisting of a heterogeneous nodule with a hypointense halo surrounded by hyperintense tissue, and a large number of tortuous vessels in the stalk (Fig. 2). The tumor was excised and the defect reconstructed with a Dufourmentel flap. Histopathology revealed the presence of lobules of basaloid cells showing maturation toward the surface, the formation of cells with abundant eosinophilic cytoplasm, sheets of eosinophilic keratinous debris, and pilar keratinization. The lobules were surrounded by a fibrous stroma with mononuclear, histiocytic inflammatory infiltrate and foreign body-type multinucleated giant cells. Numerous foci of dystrophic calcification were observed. These findings were consistent with a diagnosis of giant pilomatrixoma with foreign-body giant-cell reaction (Fig. 3). The patient progressed favorably and there was no recurrence after 1 year of follow-up.
Pilomatrixoma is a benign adnexal tumor with differentiation towards hair matrix cells, and is most common in children and those over 60.1 Although the etiology of this tumor is unknown, in 75% of cases a mutation has been identified in CTNNB1, the gene encoding beta-catenin, a signaling protein involved in hair follicle development.2
Pilomatrixomas are slow-growing nodules measuring 1 to 1.5cm across; they frequently calcify, giving rise to bluish discoloration of the overlying skin, which may extrude calcific material.3 Nodules can be multiple or solitary. Solitary tumors have been described in genetic syndromes such as Turner syndrome, Sotos syndrome, myotonic dystrophy, Rubinstein-Taybi syndrome, Gardner syndrome, trisomy 9, basal cell nevus syndrome, and xeroderma pigmentosum.4 Multiple pilomatrixomas have been reported in healthy patients.5 Other clinicopathologic variants have also been described, including blistering, anetodermic, perforating/ulcerated, lymphangiectasic, and malignant forms.
Pilomatrixomas of over 5cm in diameter are considered giant. Only 4 cases of giant pilomatrixoma have been described, all in adults6,7: 2 ulcerated and 2 with areas of erosion. Two cases of giant pilomatrixoma associated with hypercalcemia have also been described, both of which resolved after resection.7
The differential diagnosis includes dermatofibrosarcoma protuberans, calcinosis cutis, osteoma cutis, cutaneous lymphomas, sarcomas, squamous carcinoma, and cutaneous metastases.
The giant, ulcerated clinical form must be differentiated from the malignant form, and should be suspected in cases of sudden growth of a pre-existing lesion with ulceration and bleeding. Indicators of malignancy include necrosis, atypical mitotic figures, perineural or perivascular invasion, and the degree and extent of infiltration.8
Ultrasound reveals an echogenic lesion with posterior acoustic shadowing. In the present case the extension of the lesion was evaluated by MRI, which revealed an exophytic formation with hypervascularization, as described in a previous case of giant pilomatrixoma.9
The pilomatrixoma case described here is of interest due to the sudden increase in the size of the lesion; while this characteristic suggested a malignant tumor, malignancy was subsequently ruled out by histopathology.
We thank the doctors in the Hospital Nacional de Pediatría Prof. Dr. JP Garrahan who were involved in the handling and resolution of this case: Dr. Adrián Martín Pierini, Dr. Amelia Laterza, and Dr. Fabiana Lubieniecki.
Please cite this article as: Stefano P, Apa S, Balancini B. Pilomatrixoma gigante y ulcerado en un niño. Actas Dermosifiliogr. 2013;104:924–925.