A 22-year-old man consulted the dermatology department with a lesion on his right scapula. The lesion had been present since birth, was sometimes painful, and bled with friction. He reported that the lesion had been treated with cryotherapy when he was an adolescent. Nevertheless, the lesion persisted and had gradually increased in size.
Physical ExaminationThe lesion comprised several papules and tumors arranged linearly on the right scapula. These were pink, differed in size between 0.5 and 3cm in diameter, and had a pedunculated base. The spherical parts were covered with smooth, shiny skin, and many had a marked layer of yellowish, blackish hyperkeratosis that was spiked and crateriform in appearance (Fig. 1). The whole lesion measured 9.5×3cm.
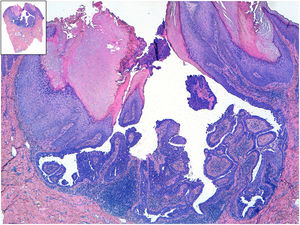
HistopathologyHistopathology revealed numerous cystic lesions that were invaginated from the epidermis and several exophytic papillomatous lesions covered by squamous epithelium with hyperkeratosis. The deepest area comprised a double-layered epithelium (the internal layer formed by cylindrical cells and the external layer formed by cuboidal myoepithelial cells). The underlying stroma was rich in plasma cells (Fig. 2).
What is your diagnosis?
DiagnosisCongenital linear syringocystadenoma papilliferum.
Course and TreatmentGiven that the lesion was causing the patient some discomfort, we removed it surgically using shave excision and electrocoagulation. No recurrences have been observed in the last 2 years.
CommentSyringocystadenoma papilliferum is an uncommon benign hamartomatous adnexal tumor.1 While its pathogenesis remains unclear, it is thought to result from pluripotent cells with eccrine differentiation and, more frequently, apocrine differentiation.2
The tumor typically affects children and adolescents; in fact, it is congenital in half of all cases.3 Clinical presentation is variable, ranging from a solitary papule (the most common manifestation) to several nodules arranged linearly, as in the present case, and often with a hyperkeratotic center. During adolescence, it tends to increase in size and become more verrucous.4
The most common locations are the scalp, face, and neck (75%).5 Less common sites include the abdomen, arm, axilla, breast, back, buttock, and vulva. The lesion has been reported on the back in only 4 cases.6
Syringocystadenoma papilliferum may appear alongside other benign adnexal tumors, such as tubular apocrine adenoma, hidradenoma papilliferum, and trichoblastoma.2 In 30% of cases, the tumor originates within a nevus sebaceus of Jadassohn.4 Basal cell carcinoma has been reported in 10% of cases. Other, more unusual associated malignant neoplasms include squamous cell carcinoma and syringocystadenocarcinoma papilliferum.3 Ulceration and/or rapid growth are indicative of malignant transformation.1
The differential diagnosis should include basal cell carcinoma, squamous cell carcinoma, and cysts.1 Diagnosis must be confirmed by biopsy. Hematoxylin-eosin staining reveals epithelial projections toward the dermis with tubular structures that connect to the surface and are composed of a double layer of cells: the external layer comprises cuboidal cells and the internal layer cylindrical cells. The stroma is rich in plasma cells.2
Treatment is based on surgical excision, although CO2 laser treatment is a good alternative when the location makes surgery difficult.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Morales-Conde M, Raya-Maldonado J, García-Bravo B, Ríos-Martin JJ. Tumoraciones con distribución lineal en la región escapular de un varón joven. Actas Dermosifiliogr. 2019;110:683–684.