Cutaneous manifestations associated with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection have been described since the first case reports from China1 and the publication of case series in Italy2 and Spain,3 among other countries. The lesion classification system proposed by Marzano et al. classifies these lesions into 6 subgroups: urticarial rash; maculopapular–morbilliform rash; papulovesicular exanthem; chilblain-like acral pattern; livedo reticularis–livedo racemosa-like pattern; and purpuric–“vasculitic” pattern.4 Here, we describe a case of papulosquamous eruption clinically and histologically reminiscent of guttate psoriasis in a patient with COVID-19.
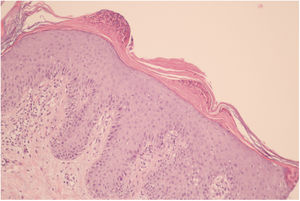
A 39-year-old woman was referred from the emergency department in our institution for pruritic lesions accompanied by a fever of up to 38.5°C, odynophagia, and malaise. She had with no personal medical history of interest and had a paternal uncle with psoriasis. The skin lesions had appeared 2 weeks earlier, developing first on the arms and later spreading to the trunk, lower limbs, face, and scalp. They consisted of erythematous papules with superficial scaling, coalescing in some areas, and were accompanied by marked hyperkeratosis on the scalp (Figs. 1 and 2). Histology of one of the lesions showed an irregular psoriasiform-type acanthotic epidermis with hyperkeratosis and parakeratosis. Aggregates of neutrophils were observed between the keratin sheets, together with foci of exudate. Perivascular mononuclear inflammatory infiltrate was observed in the superficial and mid dermis. These findings were consistent with psoriasiform dermatitis resembling guttate psoriasis (Fig. 3). Reverse transcription polymerase chain reaction (RT-PCR) was positive for SARS-CoV-2. Initial blood tests revealed no alterations. The anti-streptolysin O (AELO) antibody titer was positive (879IU/mL at 24 days). However, no throat swab culture was performed. The patient received oral antibiotic treatment with amoxicillin–clavulanic acid for 10 days, and topical treatment with calcipotriol and betamethasone ointment. During this period, complete remission of the skin lesions and systemic signs was achieved, with residual hyperpigmentation remaining.
Guttate psoriasis is the most frequently diagnosed form of psoriasis in younger patients. Although onset of this type of psoriasis has traditionally been associated with streptococcus infection, which is present in 56–97% of patients,5 associations with other acute infections caused by viruses such as chickenpox6 and Epstein–Barr virus7 are also described. Given the recent emergence of SARS-CoV-2, only one case of guttate psoriasis linked to infection by this virus has been reported.8 The affected patient was a man with a clinical history of psoriasis vulgaris who experienced a flare of skin lesions typical of guttate psoriasis coinciding with positivity for SARS-CoV-2. In that case, AELO was not detected. Our patient's rash coincided with acute SARS-CoV-2 infection and possible streptococcal coinfection, as suggested by the positive AELO titer. In this case, both SARS-CoV-2 and streptococcal infection may have acted as triggers of the skin lesions.
COVID-19 should be considered and ruled out in cases involving psoriasiform lesions together with other suggestive symptoms such as fever or sore throat.
Conflicts of InterestThe authors declare that they have no conflicts of interest.