Patients with nonmelanoma skin cancer (NMSC)—ie, basal cell carcinoma (BCC) or squamous cell carcinoma (SCC)—have an increased risk of developing a second skin cancer. The aim of this study was to describe the frequency, incidence per 1000 person-years, and predictors of a second skin cancer in a cohort of patients with NMSC treated with Mohs micrographic surgery (MMS).
Material and methodsProspective study of a national cohort of patients with NMSC who underwent MMS at 22 Spanish hospitals between July 2013 and February 2020; case data were recorded in the REGESMOHS registry. The study variables included demographic characteristics, frequency and incidence per 1000 person-years of second skin cancers diagnosed during the study period, and risk factors identified using mixed-effects logistic regression.
ResultsWe analyzed data for 4768 patients who underwent MMS; 4397 (92%) had BCC and 371 (8%) had SCC. Mean follow-up was 2.4 years. Overall, 1201 patients (25%) developed a second skin cancer during follow-up; 1013 of the tumors were BCCs (21%), 154 were SCCs (3%), and 20 were melanomas (0.4%). The incidence was 107 per 1000 person-years (95% CI, 101–113) for any cancer, 90 per 1000 person-years (95% CI, 85–96) for BCC, 14 (95% CI, 12–16) per 1000 person-years for SCC, and 2 (95% CI, 1–3) per 1000 person-years for melanoma. More men than women developed a subsequent skin cancer (738 [61%] vs 463 [39%]). The main risk factors were a history of multiple tumors before diagnosis (relative risk [RR], 4.6; 95% CI, 2.9–7.1), immunosuppression (RR, 2.1; 95% CI, 1.4–3.1), and male sex (RR, 1.6; 95% CI, 1.4–1.9).
ConclusionPatients have an increased risk of developing a second tumor after MMS treatment of NMSC. Risk factors are a history of multiple tumors at diagnosis, immunosuppression, and male sex.
Los pacientes diagnosticados de cáncer queratinocítico (carcinoma basocelular y carcinoma epidermoide cutáneo) o cáncer cutáneo no melanoma (CCNM) tienen un riesgo aumentado de desarrollar una segunda neoplasia cutánea. Nuestro objetivo es describir la frecuencia, la tasa de incidencia y los factores de riesgo predisponentes para desarrollar una segunda neoplasia cutánea en una cohorte de pacientes tratados mediante cirugía micrográfica de Mohs (CMM).
Material y métodosEstudio prospectivo de una cohorte nacional de pacientes incluidos para realización de CMM para tratar CCNM en 22 centros españoles (julio 2013-febrero 2020) REGESMOHS. Las variables analizadas incluyen las características demográficas, la frecuencia de aparición de segundas neoplasias cutáneas, sus tasas de incidencia y los factores de riesgo, y se estimaron utilizando un modelo de regresión logístico multivariante de efectos mixtos.
ResultadosFueron intervenidos 4.768 pacientes: 4.397 (92%) carcinomas basocelulares y 371 (8%) carcinomas epidermoides. El tiempo medio de seguimiento fue de 2,4 años. Se diagnosticó un nuevo tumor durante el seguimiento en 1.201 pacientes (25%); 1.013 (21%) fueron carcinomas basocelulares, 154 (3%) carcinomas epidermoides cutáneos, 20 melanomas (0,4%) La tasa de incidencia fue de 107 (101-113) por 1.000 personas/año para cualquier tumor; 90 (85-96) para el carcinoma basocelular, 14 (12-16) para el carcinoma epidermoide cutáneo y 2 (1-3) para el melanoma. El riesgo de nueva neoplasia fue mayor en varones que en mujeres 738 (61%) vs. 463 (39%). Los factores de riesgo más significativos fueron la historia de múltiples tumores previos al diagnóstico (RR: 4,6; IC 95%: 2,9-7,1); la inmunosupresión (RR: 2,1; IC 95%: 1,4-3,1) y paciente varón (RR: 1,6; IC 95%: 1,4-1,9).
ConclusiónLos pacientes diagnosticados de cáncer queratinocítico intervenido mediante cirugía de Mohs tienen un riesgo aumentado de aparición de segundas neoplasias, sobre todo en aquellos pacientes con historia de tumores múltiples al diagnóstico, inmunodeprimidos y varones.
The incidence of nonmelanoma skin cancer (NMSC) has risen, leading to higher treatment costs.1 The reported incidence of basal cell carcinoma (BCC) in Spain is 253 per 100000 person-years, while the incidence of squamous cell carcinoma (SCC) is 38.2 per 100000 person-years.2 The relative risk (RR) of a subsequent skin cancer for patients diagnosed with an NMSC versus persons in the general population ranges from 29.1 for a new BCC and 13.5 for a new SCC within 3 years of the initial NMSC diagnosis.3 Previous studies of the appearance of subsequent cancers in patients diagnosed with NMSC suggest that they appear in 22.6% of patients followed for a mean of 28.3 months4 and in 67.8% of those followed for 10 years.5 These figures oblige us to follow patients to detect new tumors in order to lower mortality.
Patients who underwent Mohs micrographic surgery (MMS) may be a subgroup at higher risk of subsequent tumors.6
The aim of this study was to assess the risk of developing a new tumor in a cohort of patients diagnosed with NMSC who were initially treated with MMS and to identify factors associated with higher risk.
Material and MethodsThe REGESMOHS registry has been described previously.7,8 Briefly, REGESMOHS stores data for a prospective cohort of patients registered starting in July 2013 at 22 Spanish hospitals that perform at least 1 MMS per week. Both private and public health system hospitals participated. All adult patients were registered consecutively as they were evaluated for MMS. Only minors and patients found legally incompetent were excluded.
Variables were grouped as they included recorded during clinical visits. Information registered on the first visit were demographic data; history of diseases or conditions associated with immunosuppression, such as hematologic diseases, transplant recipients, prolonged immunosuppression, and diabetes mellitus; clinical and histopathologic features of the tumor; and prior treatments. In the second visit we recorded surgical variables: type of Mohs surgery, anesthesia, hospital admission, anticoagulant and antiplatelet management during the procedure, size of the surgical defects and reconstructions, complementary treatments, duration of surgery, complications, and intraoperative morbidity. In the third visit short-term results and complications were recorded. In successive visits up to at least 1 year, we assessed the outcome of surgery and registered recurrences and the development of new tumors. Patients who had more than 1 tumor treated with Mohs surgery during the registry period and follow-up will be described in this study, although only the initial tumor was registered in REGESMOHS.
Information was collected according to a set protocol in an online system (OpenClinica, version 3.1, Waltham, MA, USA). Data quality was monitored online on a continuing basis and in situ at each participating hospital annually to ensure compliance with the data collection protocol in each center and verify that data were consistent with source documents.
Statistical AnalysisWe analyzed data for patients diagnosed with NMSC (BCC or SCC) who underwent MMS. Descriptive statistics were compiled and expressed as mean (SD) if normally distributed and median (interquartile range [IQR]) if nonnormally distributed. Categorical variables were reported as number and percentage. We compared data for patients who developed a subsequent tumor to data for patients who did not have new tumors using the Mann–Whitney U test, the t test, Pearson's χ2 test, or the Fisher exact test as appropriate for distributions.
Incidences and 95% CIs were calculated by dividing the number of new tumors by the number of patient-years of follow-up. To analyze factors associated with RR for developing new tumors, we used a mixed effects logistic regression model. Hospital was considered a random effect and year of surgery a fixed effect. Cumulative incidence curves were used to show survival time from surgery until the appearance of a new tumor within a scenario of competing risks, where death was considered the main competing factor. We used Stata software (version 16.1, Statacorp, College Station, TX, USA) to process the data. Statistical significance was set at a P value less than .05.
The study was approved by the ethics committee of Navarre (EO11/2013) in compliance with the Declaration of Helsinki and current laws. All patients gave their signed consent to participation in the study.
ResultsA total of 4768 patients underwent MMS; 4397 (92%) were diagnosed with BCC and 371 (8%) with SCC (Table 1). Follow-up continued for a mean (SD) of 2.4 (1.6) years for patients with BCCs and 2.2 (1.5) years for those with SCCs.
Description of the Study Population, Results, and Treatment of New Tumors.
| Patients | BCC | SCC | |
|---|---|---|---|
| No. of patients, n (%) | 4768 (100) | 4397 (100) | 371 (100) |
| Patient follow-up visits, n | 11.241 | 10.426 | 815 |
| Follow-up, mean (SD), y | 2.4 (1.6) | 2.4 (1.6) | 2.2 (1.5) |
| New skin cancer after MMS, n (%) | 1201 (25) | 1111 (25) | 90 (24) |
| BCC | 1013 (21) | 960 (22) | 53 (14) |
| SCC | 154 (3) | 121 (3) | 33 (9) |
| Other, including melanoma | 34 (0.7) | 30 (0.7) | 4 (1) |
| Melanoma only | 20 (0.4) | 19 (0.4) | 1 (0.3) |
| Number of new skin tumors | |||
| 1 | 756 (16) | 702 (16) | 54 (15) |
| 2 | 270 (6) | 248 (6) | 22 (6) |
| ≥3 | 175 (4) | 161 (4) | 14 (4) |
| Treatment of new skin tumors | |||
| Topical treatment, electrosurgery, cryotherapy | 97 (9) | 93 (9) | 4 (1) |
| Conventional surgery | 856 (76) | 791 (76) | 55 (18) |
| MMS | 168 (15) | 157 (15) | 11 (3) |
| Radiotherapy | 3 (<1) | 3 (<1) | 0 (<1) |
| Other | 2 (<1) | 1 (<1) | 1 (<1) |
| Incidence, n per 1000 person-years (95% CI) | |||
| Any tumor type | 107 (101–113) | 107 (100–113) | 110 (90–136) |
| BCC | 90 (85–96) | 92 (86–98) | 65 (50–85) |
| SCC | 14 (12–16) | 12 (10–14) | 41 (29–57) |
| Other, including melanoma | 3 (2–4) | 3 (2–4) | 5 (2–13) |
| Melanoma only | 2 (1–3) | 2 (1–3) | 1 (0–9) |
Abbreviations: BCC, basal cell carcinoma; MMS, Mohs micrographic surgery; SCC, squamous cell carcinoma.
A new malignant tumor was diagnosed in 1201 patients (25%). In 1013 of them (21%) the diagnosis was BCC, in 154 (3%) it was SCC, and in 20 (0.4%) it was melanoma. In 960 patients (22%) whose initial tumor was a BCC, the new tumor was also a BCC; in 212 cases (3%) it was an SCC. In patients whose MMS procedure removed an SCC, the subsequent tumor was a BCC in 53 cases (14%) and an SCC in 33 (9%).
A single new tumor was diagnosed in 756 patients (16%), while 2 new tumors appeared in 270 (6%), and 3 or more appeared in 175 (4%).
Most of the new tumors were removed with conventional surgery (856 patients [76%]). However, MMS was used in 168 cases (15%) and topical treatments (imiquimod, photodynamic therapy, electrosurgery, or cryotherapy) in 97 (9%). Radiotherapy was used in 3 patients and other treatments in 2 patients (vismodegib in 1 of them). One patient declined treatment.
The incidence of new tumors of any type was 107 (95% CI, 101–113) per 1000 person-years. The incidences for BCC, SCC, and melanoma, respectively, were 90 (95% CI, 85–96) per 1000 person-years, 14 (95% CI, 12–16) per 1000 person-years, and 2 (95% CI, 1–3) per 1000 person-years (Table 1).
The appearance of a new tumor was associated with male sex and age (Table 2). The median (IQR) age was 73.9 years (65.9–80.9 years) in the group with subsequent tumors and 69.9 years (58.1–79.5 years) in the group with none.
Demographic, Clinical, and Histologic Information Registered at the First Visit.
| New skin tumorsa | |||
|---|---|---|---|
| Characteristics | Non=3567 (100%) | Yesn=1201 (100%) | P value |
| Sex | <.001 | ||
| Male | 1718 (48) | 738 (61) | |
| Female | 1849 (52) | 463 (39) | |
| Age, median (IQR), y | 69.9 (58.1–79.5) | 73.9 (65.9–80.9) | <.001 |
| Place of residence | <.001 | ||
| Health district with a reference hospital | 2736 (77) | 1044 (87) | |
| Another health district | 806 (23) | 152 (13) | |
| Immunosuppression | .0002 | ||
| No | 3476 (97) | 1143 (95) | |
| Yes | 91 (3) | 58 (5) | |
| Diabetes mellitus | .0933 | ||
| No | 3093 (88) | 1022 (87) | |
| Yes | 404 (12) | 158 (13) | |
| Prior history of tumors | <.001 | ||
| No | 3523 (99) | 1132 (94) | |
| Yes | 44 (1) | 69 (6) | |
| Prior history of skin tumors | |||
| Time elapsed since appearance, median (IQR), mo | 14.4 (6.7–32.8) | 12.2 (5.8–29.5) | .0031 |
| Histologic type | .6674 | ||
| BCC | 3286 (92) | 1111 (93) | |
| SCC | 281 (8) | 90 (7) | |
| Histologic aggressiveness | .0101 | ||
| No | 990 (28) | 380 (32) | |
| Yes | 2577 (72) | 821 (68) | |
| Size | .2969 | ||
| <10mm | 1455 (42) | 471 (40) | |
| ≥10mm | 2036 (58) | 708 (60) | |
| Type | .0174 | ||
| Primary | 2255 (63) | 751 (63) | |
| Recurrent | 702 (20) | 275 (23) | |
| Persistent | 610 (17) | 175 (15) | |
| Site | .0250 | ||
| Area Hb | 2880 (81) | 929 (78) | |
| Area Mc | 643 (18) | 258 (22) | |
| Area Ld | 18 (1) | 8 (1) | |
| Prior surgical treatment | .5154 | ||
| No | 2907 (82) | 991 (83) | |
| Yes | 646 (18) | 208 (17) | |
| Prior nonsurgical treatment | .0009 | ||
| No | 3393 (96) | 1117 (93) | |
| Yes | 152 (4) | 80 (7) | |
Abbreviations: BCC, basal cell carcinoma; IQR, interquartile range; SCC, squamous cell carcinoma.
Demographic, clinical, and histologic data for both groups are summarized in Table 2.
Table 3 shows the risk factors for the appearance of new tumors that were identified by univariable analysis. Table 4 shows the risk factors identified by multivariable analysis. After adjusting the models, we found that the main risk factors were multiple tumors on diagnosis (RR, 4.59; 95% CI, 2.95–7.13), immunosuppression (RR, 2.11; 95% CI, 1.44–3.08), and male sex (RR, 1.61; 95% CI, 1.39–1.85) (Table 4).
Univariable Analysis of Risk Factors for the Appearance of Subsequent Skin Tumors After MMS.
| Factors | RR (95% CI) | P value |
|---|---|---|
| Patient | ||
| Male sex | 1.72 (1.50–1.97) | <.001 |
| Age in y | 1.03 (1.02–1.03) | <.001 |
| Residence not near a reference hospital | 0.56 (0.46–0.68) | <.001 |
| Immunosuppression, yes | 2.00 (1.41–2.83) | .0001 |
| History of prior tumors, yes | 5.2 (3.47–7.81) | <.001 |
| Initially diagnosed skin tumors | ||
| Time since appearance in y | 0.98 (0.96–1.00) | .0813 |
| Histologic type | ||
| BCC | Reference | |
| SCC | 0.98 (0.76–1.26) | .8766 |
| Aggressive, yes | 0.88 (0.75–1.02) | .0899 |
| Tumor type | ||
| Primary | Reference | |
| Recurrent | 1.18 (1–1.4) | .0492 |
| Persistent | 0.9 (0.74–1.09) | .2758 |
| Site | ||
| Area Ha | Reference | |
| Area Mb | 1.24 (1.05–1.46) | .0118 |
| Area Lc | 1.42 (0.61–3.32) | .4141 |
| Prior nonsurgical treatment, yes | 1.67 (1.25–2.22) | .0004 |
Abbreviations: BCC, basal cell carcinoma; MMS, Mohs micrographic surgery; RR, relative risk; SCC, squamous cell carcinoma.
Multivariable Analysis of Risk Factors for the Appearance of Subsequent Skin Tumors After MMS.
| Factors | RR (95% CI) | P value |
|---|---|---|
| Year of MMS | 0.79 (0.75–0.83) | <.001 |
| Male sex | 1.61 (1.39–1.85) | <.001 |
| Age in y | 1.03 (1.02–1.03) | <.001 |
| Residence not near a reference hospital | 0.62 (0.5–0.77) | <.001 |
| Immunosuppression, yes | 2.11 (1.44–3.08) | .0001 |
| Prior tumor, yes | 4.59 (2.95–7.13) | <.001 |
| Prior nonsurgical treatment, yes | 1.78 (1.31–2.43) | .0002 |
| Hospitalization, yes | 0.59 (0.43–0.8) | .0008 |
| Incomplete MMS, yes | 0.59 (0.35–0.99) | .0445 |
Abbreviations: MMS, Mohs micrographic surgery; RR, relative risk.
Our study shows a high incidence of subsequent skin cancer after MMS treatment of NMSCs, especially in men, patients initially presenting with multiple tumors, and patients who are immunocompromised.
Previous studies also reported that patients with NMSC are at greater risk of developing subsequent tumors.3,9–15 Domínguez-Cruz et al.4 found a 22.6% risk in a retrospective cohort of 926 patients diagnosed with NMSC; mean follow-up was 6.4 years (range, 0.5–12.1 years). Revenga et al.3 estimated a RR of 29.1 for a new BCC and 13.6 for a new SCC in a retrospective cohort of 118 patients initially diagnosed with NMSC. In a prospective cohort of 1805 patients with this diagnosis, Karagas et al.11 calculated the risk of subsequent NMSC to be 17%, 35%, and 50% at 1, 3, and 5 years, respectively.
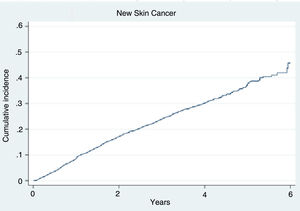
A study by Schinstine & Goldman6 of patients with characteristics similar to ours—with MMS-treated NMSCs and followed for 2 years—reported a frequency of multiple new tumors of 19.8% (in 87 of 440 patients) and a frequency of single new tumors of 19.5% (in 86 of 440). Our study population of 4768 patients followed for a mean of 2.4 (1.6) years, was representative of patients with NMSCs treated with MMS in Spain. We registered a lower percentage (2%) of cases of multiple tumors at diagnosis, yet the frequency of subsequent tumors was somewhat higher in our patients, at 25% (in 1201), than in the study of by Schinstine & Goldman. The frequencies of subsequent tumors after MMS treatment reported from studies with fewer than 5 years of follow-up have ranged from 14.6%13 to 22%.14 We calculated an incidence of 107 (101–113) per 1000 person-years for new NMSCs of any type. The incidences per 1000 person-years were 90 (85–96) for BCC, 14 (12–16) for SCC, and 2 (1–3) for melanoma (Table 1). Fig. 1 is a graph of the cumulative incidence of new skin cancers.
The strongest risk factor for developing a subsequent NMSC in our cohort was the presence of multiple tumors on diagnosis (RR, 4.59), consistent with the literature.5,6,12 Immunosuppression (RR, 2.11) was another important factor. Some studies have excluded immunocompromised patients when calculating risk for subsequent NMSC.4 Male sex (RR, 1.61,) was also important, consistent with the findings of Karagas et al.,11 although other studies have seen similar frequencies in both sexes.6,13 Prior nonsurgical treatment (RR, 1.78) also conferred risk for a new tumor in our study, as did whether the initial MMS-treated tumor was recurrent (RR, 1.18) or not.
Strengths of our study include its prospective design, the large population size, the representativeness of the MMS-treated patients with NMSC in Spain, and the long-term follow-up of cases. A possible limitation is the difficulty of organizing follow-up for some of our patients, especially those living in areas far from referral hospitals. Supporting the relevance of this limitation is the fact that such residence or the need for hospitalization were protective factors, possibly indicating bias since recurrence would have been more difficult to detect in such patients. If bias was present, the real incidence of new tumors would be even higher than the incidence we report and would therefore support our conclusions.
We conclude that subsequent skin tumors are very frequent in patients whose initial tumors are treated with MMS, particularly in men, immunocompromised patients, or those who have multiple tumors on diagnosis. Our findings suggest that there is a need for long-term follow-up of patients after MMS. In addition, full-body skin examination is probably necessary, rather than the examination only of the operated zone.
FundingREGESMOHS(the registry of Mohs micrographic surgery procedures performed in 22 Spanish hospitals) was promoted by the Healthy Skin Foundation of the Spanish Academy of Dermatology and Venereology (AEDV) with funding from Roche Pharma. This study also received funding from Sun Pharma. Neither Roche Pharma nor Sun Pharma participated in the design of the study or data analysis and interpretation.
Conflicts of InterestThe authors declare no conflicts of interest.