A 56-year-old man, with a past medical history of stage IIIA squamous cell carcinoma of the lung who had received 4 cycles of neoadjuvant chemotherapy (CT) with cisplatin–vinorelbine and radiotherapy. Ultimately, the tumor was deemed unresectable, and treatment with carboplatin, paclitaxel, and pembrolizumab every 3 weeks was initiated. Four weeks after initiation and after the 2nd cycle, he developed an asymptomatic rash on his left flank, leading to referral to our clinic with a clinical suspicion of herpes zoster.
Physical examinationThe physical examination revealed the presence multiple erythematous, shiny, flat papules on the left hemithorax, coalescing in a serpiginous pattern along Blaschko's lines. With dermoscopy, the lesions showed multiple red and gray dots (Fig. 1).
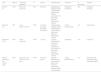
HistopathologyHistopathological examination showed a moderate inflammatory infiltrate with deep periannexial extension (Fig. 2A) and, at higher magnification, an epidermis with vacuolar degeneration of the basal layer and apoptotic keratinocytes. The inflammatory infiltrate was primarily lymphoplasmacytic, with perivascular and interstitial distribution, and with the presence of extravasated blood and melanophages (Fig. 2B and C).
(A) Punch biopsy including epidermis, dermis, and subcutaneous tissue. The superficial dermis shows a moderate inflammatory infiltrate with deep periannexial extension (hematoxylin–eosin [HE], ×20). (B, C) Slightly hyperplastic epidermis, vacuolar degeneration of the basal layer, and occasional apoptotic keratinocytes. The inflammatory infiltrate is mainly lymphoplasmacytic, with an interstitial and perivascular distribution and lymphocytic exocytosis into the epidermal basal layer. Additionally, slight edema of the superficial dermis, extravasated blood, and melanophages are observed (hematoxylin–eosin [HE], ×80 [b] and ×200 [c]).
What is your diagnosis?
DiagnosisLichenoid cutaneous eruption following the Blaschko's lines due to pembrolizumab.
Course of the disease and treatmentTreatment with topical betamethasone was initiated, and the patient completed a total of 4 cycles of CT-immunotherapy (IT), followed by maintenance treatment with pembrolizumab 200mg every 3 weeks. The lesions resolved, leaving residual post-inflammatory hyperpigmentation, and have not recurred after 7 additional cycles.
CommentLichenoid mucocutaneous eruptions are an immune-mediated cutaneous adverse effect primarily related to anti-PD1/PDL1 agents.1 These eruptions show significant clinical variability, and a wide range of anatomical distributions has been reported, including localized, generalized, palmoplantar, mucosal, follicular, or ungual variants.1 The onset of this cutaneous toxicity is usually late, weeks or months after treatment initiation.2 However, this latency can be highly variable, ranging from a few days to more than a year.1 In most cases, these are mild-to-moderate reactions and can be easily managed without discontinuing IT.2
Currently, only 3 cases of IT-related blaschkoid lichenoid cutaneous reactions have been reported (Table 1).3–5 However, other drugs such as angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers, or anti-TNF-α agents have been involved in the development of lichenoid eruptions with this distribution.6 Blaschko's lines reflect the migration of neural crest cells during embryogenesis. Dermatoses that follow Blaschko's lines would, therefore, be the cutaneous expression of genetic mosaicism caused by a postzygotic mutation, leading to the appearance of genetically distinct cell populations in the same individual. The resulting clonal cells may have a different histocompatibility antigen profile and, consequently, be more susceptible to T-cell-induced cytotoxicity after appropriate endogenous or environmental stimuli.6 It could be hypothesized that anti-PD1 induced T-cell activation may have been the trigger that, in our patient, unmasked a latent subpopulation of abnormal keratinocytes.5
Published cases of lichenoid cutaneous eruptions following immunotherapy-related Blaschko's lines.
| Case | Age/sex | Underlying neoplasm | IT | Latency | Histopathology | Treatment | IT interruption | Outcome |
|---|---|---|---|---|---|---|---|---|
| Biolo et al.3 | 77/M | Renal cell carcinoma | NIV | 8 months | Hyperkeratosis, hypergranulosis, Civatte bodies, subepidermal clefting, vacuolization of basal layer, band-like inflammatory infiltrate | Clobetasol, prednisone | NS | Complete remission |
| Ogawa et al.4 | 79/F | Lung adenocarcinoma | PEM | 10 months (6 months after PEM completion) | Hyperkeratosis, hypergranulosis, Civatte bodies, vacuolization of basal layer, lichenoid inflammatory infiltrate | Topical corticosteroids | NA | Improvement |
| Ganbichler et al.5 | 39/M | Breast carcinoma | PEM | 7 cycles | Compact orthokeratosis, acanthosis, scattered dyskeratosis, vacuolization of basal layer, band-like inflammatory infiltrate | Clobetasol | Yes | Clearance |
| Álvarez-Salafranca et al. (current case) | 56/M | Squamous cell carcinoma of the lung | PEM | 4 weeks (2 cycles) | Apoptotic keratinocytes, vacuolization of basal layer, lichenoid inflammatory infiltrate, dermal melanophages | Topical betamethasone | No | Resolution with post-inflammatory hyperpigmentation |
IT: immunotherapy; M: male; F: female; NA: not applicable; NS: not specified; NIV: nivolumab; PEM: pembrolizumab.
The differential diagnosis should include herpes zoster, as it can temporarily limit the continuity of treatment. In our case, the absence of pain, along with the non-metameric distribution and a more prolonged course of the disease, allowed us to rule it out. Furthermore, an acquired unilateral rash in the context of advanced cancer requires ruling out zosteriform metastasis. This possibility was excluded based on the distribution and histopathological analysis. Finally, it should be noted that there is a broad spectrum of acquired blaschkoid dermatoses, including adult inflammatory linear verrucous epidermal nevus, linear psoriasis, blaschkitis, or lichen striatus, among others. Specifically, there is clinical and histopathological overlap between the spectrum of lichen striatus/blaschkitis and linear lichen planus or drug-induced lichenoid eruptions.7 In this regard, spongiotic changes would favor the diagnosis of blaschkitis or lichen striatus. Nevertheless, the definitive diagnosis must be established based on a comprehensive clinicopathological correlation, taking into account age, distribution, clinical and histological findings, as well as drug history.
Conflicts of interestNone declared.




![(A) Punch biopsy including epidermis, dermis, and subcutaneous tissue. The superficial dermis shows a moderate inflammatory infiltrate with deep periannexial extension (hematoxylin–eosin [HE], ×20). (B, C) Slightly hyperplastic epidermis, vacuolar degeneration of the basal layer, and occasional apoptotic keratinocytes. The inflammatory infiltrate is mainly lymphoplasmacytic, with an interstitial and perivascular distribution and lymphocytic exocytosis into the epidermal basal layer. Additionally, slight edema of the superficial dermis, extravasated blood, and melanophages are observed (hematoxylin–eosin [HE], ×80 [b] and ×200 [c]). (A) Punch biopsy including epidermis, dermis, and subcutaneous tissue. The superficial dermis shows a moderate inflammatory infiltrate with deep periannexial extension (hematoxylin–eosin [HE], ×20). (B, C) Slightly hyperplastic epidermis, vacuolar degeneration of the basal layer, and occasional apoptotic keratinocytes. The inflammatory infiltrate is mainly lymphoplasmacytic, with an interstitial and perivascular distribution and lymphocytic exocytosis into the epidermal basal layer. Additionally, slight edema of the superficial dermis, extravasated blood, and melanophages are observed (hematoxylin–eosin [HE], ×80 [b] and ×200 [c]).](https://static.elsevier.es/multimedia/00017310/0000011600000009/v1_202510020504/S0001731025005071/v1_202510020504/en/main.assets/thumbnail/gr2.jpeg?xkr=ue/ImdikoIMrsJoerZ+w9/t1/zx4Q/XH5Tma1a/6fSs=)



