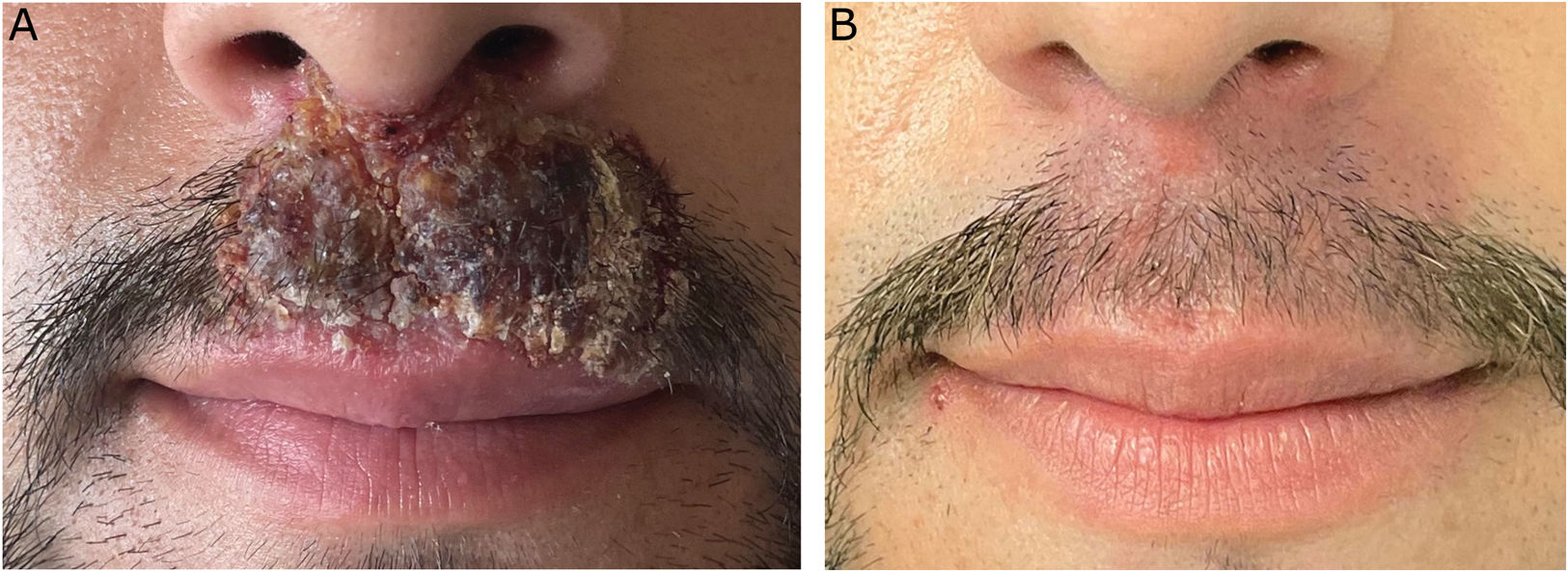
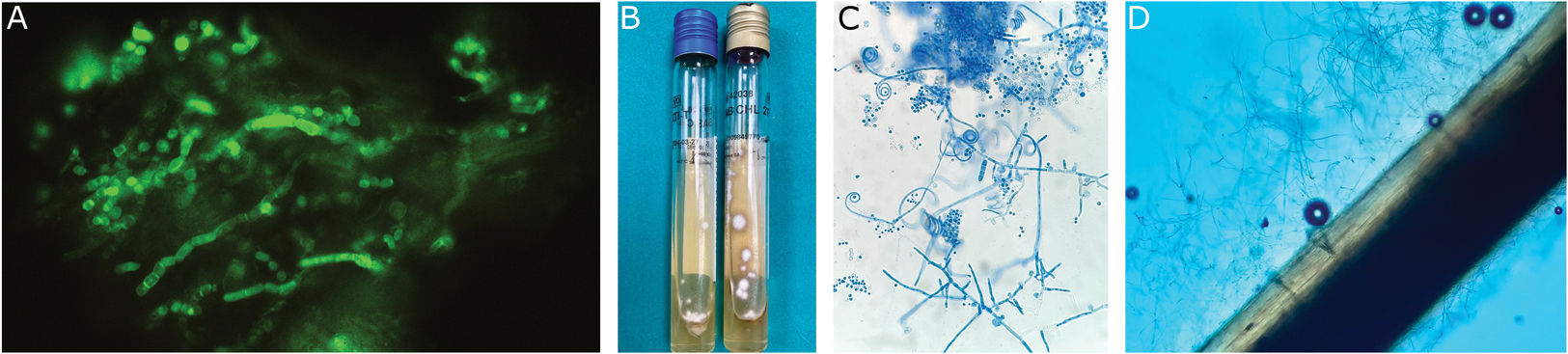
A 36-year-old man presented with a 2-week history erythematous–edematous plaque, exhibiting desquamation and positive hair-pull test, affecting the upper lip and nasal vestibules (Fig. 1A). No other lesions were identified elsewhere. He had been on topical mupirocin and fusidic acid, acyclovir, cloxacillin, amoxicillin–clavulanate, and systemic glucocorticoids, due to a suspected diagnosis of impetiginized herpes simplex with a torpid course. Material for direct examination was obtained by scraping the lesion (Fig. 2A). After 7 days, culture showed flat, powdery colonies with yellow margins and an orange pigment on the reverse side after 10 days of incubation (Fig. 2B). Microculture revealed the presence of septate hyaline hyphae with occasional spiral hyphae typical of the causative agent, spherical microconidia, and multi-septate smooth-walled macroconidia (Fig. 2C). The hair perforation test demonstrated the invasive capacity of the agent on the hair shaft (Fig. 2D). In a directed anamnesis, the only notable antecedent was his habit of having his beard trimmed at a barbershop.
(A) Direct examination of the sample with calcofluor white, showing abundant septate hyphae. (B) Growth of flat, powdery colonies, with yellow margins and orange pigment on the reverse after 10 days of incubation at 30°C on Sabouraud agar with chloramphenicol (yellow cap) and Sabouraud agar with chloramphenicol and actidione (blue cap). (C) Microculture showing septate hyaline hyphae with occasional spiral hyphae typical of the causative agent, spherical microconidia, and multi-septate smooth-walled macroconidia. (D) Positive hair perforation test on neonatal hair, showing conical images with a base on the outer part and apex on the inner part of the hair, demonstrating invasive capacity in the hair.
What is your diagnosis?
DiagnosisInflammatory tinea barbae caused by Trichophyton interdigitale.
CommentsThe diagnosis was confirmed by mass spectrophotometry (MALDI-TOF). After treatment with an 8-week regimen of oral terbinafine, at a dose of 250mg/24h, associated with topical terbinafine cream every 12h, the patient showed clinical (Fig. 1B) and mycological resolution of the condition.
Dermatophytoses are a common reason for consultation. The term “dermatophyte” implies the microorganism's affinity for keratinized tissue, regardless of taxonomic or molecular classification. Within the overall scope, tinea barbae is infrequent or underreported. Advanced age, immunosuppression, diabetes, local trauma, or occupational factors confer an increased risk. Although it is generally caused by zoophilic fungi (Trichophyton verrucosum, Trichophyton mentagrophytes, Microsporum canis), in recent years there has been an increase in anthropophilic fungi such as Trichophyton rubrum and some emerging ones such as Trichophyton benhamiae1 or Trichophyton tonsurans in Europe.2 Originally, it was attributed to suboptimal disinfection of material used in hairdressers-barbershops, and a decrease in its incidence rate for this reason has been observed thanks to various legal regulations.2
Tinea barbae can be superficial, inflammatory (analogous to kerion of tinea capitis), or circinate. Human-to-human transmission is rare but possible, and self-inoculation from another skin focus, which was not present in our case, should be ruled out.3 Culture growth, usually rapid (7–14 days), constitutes the diagnostic test of choice. Biopsy is reserved for doubtful cases.
The treatment of choice is oral antifungals (terbinafine, itraconazole, fluconazole, or griseofulvin), with topical antifungals possibly added. The exact duration is not supported by any guideline or consensus, but it is accepted to maintain them for 4–6 weeks and/or until 2–3 weeks after resolution. In our case, we extended the treatment for 8 weeks due to persistent erythema and minimal desquamation at 6 weeks, confirming mycological cure after that period.
Our case illustrates, from a clinical point of view, that early diagnosis and treatment can limit possible scarring sequelae. Clinical suspicion is fundamental, given the differential diagnosis with impetigo, contact dermatitis, folliculitis, and other entities that lead to antibiotic treatments, which are not useful. Given the delay in culture results, initiating empirical antifungal treatment is justified if there is high suspicion.
Secondly, it presents a microbiological interest, as inflammatory tineas are mostly a consequence of zoophilic fungi (T. rubrum, T. mentagrophytes, and Trichophyton erinacei, among others).4 However, anthropophilic fungi such as T. interdigitale—frequently involved in tinea pedis and tinea unguium—very exceptionally cause inflammatory tineas.3,4 It is important to rely on molecular diagnosis in the T. mentagrophytes complex given the recent changes in its taxonomy, which is under continuous review. Trichophyton is a polyphyletic genus of the family Arthrodermataceae, currently considered analogous to clade A in the phylogenetic tree of dermatophyte fungi.5T. interdigitale is understood as an anthropophilic clonal descendant of T. mentagrophytes (clade A1), in compliance with the proposed hypothesis of a geophilic ancestor that would be generating clonal descendants with an increasing degree of adaptation to the human host.5,6 A more detailed study is needed in the coming years to achieve greater nomenclatural stability. Finally, it presents an epidemiological interest, in view of the recent alert from the Spanish Academy of Dermatology and Venereology on the increase in cases of tinea capitis in Spain detected in barbershops,7 previously reported in Germany.8 Although we cannot demonstrate causality, our case is a tinea barbae whose only relevant antecedent was repeated visits to a barbershop.
Conflicts of interestNone declared.
Special thanks to Dr. Marta Martín García for her interest and comprehensive and meticulous study of the case, providing valuable microbiological information.