Interleukin 12/23 inhibitors (IL12/23i) and interleukin 17 and 23 inhibitors (IL17i and IL23i) represent the drug classes with the most favorable expectations for therapeutic response. However, the introduction of biosimilars has led many centers, for reasons of efficiency, to prioritize tumor necrosis factor inhibitors (TNFi) as first-line therapy. Data on whether prior exposure to TNFi may affect the drug survival of IL17i and IL23i therapies are lacking. Using data from the Biobadaderm registry, we compared treatment persistence among patients with psoriasis who received IL17i or IL23i as first-line therapy and those who received these agents after prior TNFi treatment. Rates of treatment discontinuation and adverse events (AEs) were compared between groups. Results showed that overall drug survival was higher in patients treated first line with IL17i or IL23i vs those treated after TNFi exposure. However, no significant differences were observed between groups in treatment discontinuation due to inefficacy or serious AEs. Overall AE rates were similar, with no differences in serious AEs or serious infections. Although global AE rates and discontinuation due to AEs were higher in patients previously on TNFi who subsequently received IL17i or IL23i vs biologic-naïve patients, these differences did not reach statistical significance. In conclusion, this study suggests that prior exposure to TNFi may influence the persistence of IL17i and IL23i therapies in patients with psoriasis.
The treatment of moderate-to-severe plaque psoriasis has advanced significantly over the past 20 years, particularly with the development of targeted therapies – first with tumor necrosis factor-alpha inhibitors (TNFi) and later with interleukin-12/23 inhibitors (IL12/23i) and interleukin-17 and interleukin-23 inhibitors (IL17i and IL23i). These treatments have demonstrated high efficacy in controlling psoriasis symptoms.
Numerous studies have evaluated the efficacy of TNFi agents such as infliximab, etanercept, and adalimumab in plaque psoriasis, showing significant improvement in symptoms and patient quality of life.1,2 The introduction of biosimilars has further increased their use – especially adalimumab – frequently positioning them as the first-line biological option due to cost-effectiveness.3 However, some patients exhibit limited responses4 or develop resistance over time.5
The arrival of interleukin inhibitors, particularly IL17i and IL23i, has expanded therapeutic options with more targeted mechanisms and generally high efficacy in psoriasis. Clinical development programs, including numerous head-to-head trials, suggest these therapies may be especially effective in patients who respond inadequately to TNFi or who experience adverse events.6,7 However, the impact of prior TNFi exposure on the persistence or survival of these more specific therapies remains unclear.
In Spain's public health system, treatment recommendations and funding decisions for innovative therapies are defined in Therapeutic Positioning Reports (TRP). For psoriasis, clinical practice guidelines recommend initiating therapy with conventional systemic agents (methotrexate, cyclosporine, or acitretin), unless contraindicated or not tolerated. If a biologic is required, a TNFi biosimilar is recommended as first-line for reasons of efficiency. Given these policies, questions arise regarding whether prior TNFi exposure influences the survival of IL17i and IL23i therapies, affects disease evolution, and whether this impact is similar across biological drug classes.
To explore the association between prior TNFi exposure and the survival of IL17i and IL23i therapies in plaque psoriasis, we conducted an analysis using data from the Spanish Registry of Systemic Adverse Events in Psoriasis (BIOBADADERM).
Materials and methodsThe data analyzed originate from the BIOBADADERM registry, created to monitor adverse events associated with systemic psoriasis therapy. A detailed description of data collection and coding has been previously published.8,9 BIOBADADERM is a nationwide, prospective, multicenter cohort registry of patients with psoriasis in real-world practice. This study included all patients registered across 21 hospitals in Spain from January 2008 through November 2023. The analysis compared patients receiving IL17i or IL23i as first-line biologic therapy vs those receiving the same agents after TNFi exposure.
BIOBADADERM undergoes continuous online monitoring, with annual onsite audits for data validation. The registry was approved by the Ethics Committee of Hospital 12 de Octubre (216/07) (Madrid, Spain) and complies with the Declaration of Helsinki.
The primary analysis compared treatment persistence or survival of IL17i and IL23i therapies between biologic-naïve patients and those previously treated with TNFi. Secondary analyses included reasons for treatment discontinuation and adverse event (AE) rates.
Statistical analysisA descriptive analysis was performed for each group, presenting absolute numbers and percentages for qualitative variables and mean±standard deviation for quantitative variables. Group differences were tested using chi-square or Student's t-tests.
Subsequently, treatment persistence was analyzed, defined as the follow-up time from treatment initiation until discontinuation or switching to another therapy. The results were presented using Kaplan–Meier survival curves. To compare survival curves, the log-rank test and a Cox regression model were applied, followed by verification of the proportional hazards assumption. The comparison of specific causes of discontinuation was examined within a competing-risks survival framework. To compare cumulative incidence function (CIF) curves for treatment discontinuation – whether due to inefficacy or an AE – competing-risks regression models were used. These models estimate each cause-specific subhazard ratio (SHR) for inefficacy or AE, which are interpreted similarly to hazard ratios in Cox regression. Inefficacy and AEs were considered the main competing events, whereas all other causes of discontinuation (e.g., loss to follow-up, patient decisions, planned or desired pregnancy, etc.) were treated as right-censored observations. SHR estimates were first obtained using crude models and then through multivariable models.
Finally, AE incidence rates were calculated per 1000 patient-years with 95% confidence intervals (CI). Incidence rate ratios – crude and adjusted – were computed via Poisson regression with robust variance to account for overdispersion.
In some variables, missing values ranged from 0.4% (age) to 29.1% (alcohol consumption). Multiple imputation was used to handle missing data, creating 20 complete datasets using chained equations. In subsequent stages, each of the 20 datasets was analyzed using regression models specific to each outcome. Finally, the results from the complete datasets were pooled into a single set of estimates using Rubin's rules.
All analyses were performed using STATA v17.0. A p-value <0.05 was considered statistically significant.
ResultsAs of November 2023, BIOBADADERM included 5905 patients receiving systemic therapy, with 14,134 treatment cycles. A total of 891 patients met inclusion criteria: 359 received IL17i as first-line vs 245 after TNFi, and 128 received IL23i as first-line vs 159 after TNFi.
The characteristics of the patients are shown in Table 1. Notably, patients who received IL17 inhibitors (IL17i) or IL23 inhibitors (IL23i) as first-line therapy had a shorter disease duration – 14.8 and 15.1 years, respectively – vs those who received IL17i or IL23i after prior TNF inhibitor (TNFi) therapy (20.4 and 19.8 years). They also had more severe psoriasis, with a baseline Psoriasis Area and Severity Index (PASI) of 10.5 in both naïve groups, vs 6.0 and 8.7 in the IL17i and IL23i groups previously exposed to TNFi, respectively. Of note, among patients treated with IL17i, there was a higher proportion of psoriatic arthritis (PsA) vs those receiving IL23i; however, no significant differences were observed between the specific cohorts being compared (naïve vs TNFi-experienced). Among IL23i-treated patients, PsA was less frequent in the naïve group than in those previously treated with TNFi.
Descriptive characteristics according to treatment used (IL17 inhibitors or IL23 inhibitors) or preceded by TNF inhibitors.
| IL17i naïve | IL17i/TNFi | p-Value | IL23i naïve | IL23i/TNFi | p-Value | |
|---|---|---|---|---|---|---|
| Number of patients | 359 | 245 | 128 | 159 | ||
| Patient-years | 971 | 496 | 199 | 251 | ||
| Exposure time, years, mean (SD) | 2.7 (2.0) | 2.0 (1.7) | 0.0000*** | 1.6 (1.0) | 1.6 (1.0) | 0.8836 |
| Prior TNFi exposure time, years, mean (SD) | – | 3.0 (3.4) | – | 2.4 (3.1) | ||
| Number of prior TNFi, mean (SD) | – | 1.5 (0.9) | – | 1.3 (0.7) | ||
| Female, n (%) | 157 (44) | 121 (49) | 0.1709 | 51 (40) | 66 (42) | 0.7753 |
| Current age, years. mean (SD) | 52.5 (14.7) | 52.7 (14.3) | 0.9037 | 54.7 (15.8) | 51 (14.65) | 0.0396* |
| Age at treatment start, years, mean (SD) | 49.1 (14.5) | 49.9 (13.5) | 0.4805 | 53 (16) | 49.1 (14.69) | 0.0298* |
| Disease duration at start, years, mean (SD) | 14.8 (13.9) | 20.4 (13.5) | 0.0000*** | 15.1 (13.1) | 19.8 (13.1) | 0.0035** |
| Baseline PASI, mean (SD) | 10.5 (8.8) | 6 (6.5) | 0.0000*** | 10.5 (7.8) | 8.7 (7.03) | 0.0415* |
| BMI, mean (SD) | 29.5 (8.6) | 28.5 (6.1) | 0.1312 | 29.1 (6.5) | 28.4 (6.17) | 0.3903 |
| Plaque psoriasis | 319 (89) | 201 (82) | 0.0174* | 120 (94) | 139 (87) | 0.0725 |
| Guttate psoriasis | 20 (6) | 12 (5) | 0.7169 | 4 (3) | 5 (3) | 0.9924 |
| Erythrodermic psoriasis | 4 (1) | 8 (3) | 0.0629 | 0 (0) | 3 (2) | 0.1182 |
| GPP | 4 (1) | 1 (0) | 0.3470 | 1 (1) | 1 (1) | 0.8775 |
| Palmoplantar pustular psoriasis | 34 (9) | 10 (4) | 0.0123* | 3 (2) | 3 (2) | 0.7880 |
| Annular pustular psoriasis | 0 (0) | 1 (0) | 0.2257 | 1 (1) | 1 (1) | 0.8775 |
| Acrodermatitis continua of Hallopeau | 1 (0) | 0 (0) | 0.4084 | 0 (0) | 1 (1) | 0.3688 |
| Psoriatic arthritis | 75 (21) | 52 (21) | 0.9214 | 5 (4) | 12 (8) | 0.1940 |
| Ischemic heart disease | 12 (4) | 5 (3) | 0.4498 | 6 (7) | 2 (2) | 0.0453* |
| Heart failure | 3 (1) | 0 (0) | 0.1731 | 3 (4) | 1 (1) | 0.1612 |
| Hypertension | 83 (27) | 53 (27) | 0.9113 | 41 (45) | 30 (24) | 0.0019** |
| Diabetes | 42 (14) | 30 (16) | 0.5319 | 25 (29) | 18 (15) | 0.0149* |
| Hypercholesterolemia | 113 (37) | 76 (38) | 0.7121 | 34 (40) | 42 (34) | 0.401 |
| COPD | 8 (3) | 6 (3) | 0.7344 | 4 (5) | 1 (1) | 0.0735 |
| Chronic liver disease | 63 (21) | 17 (9) | 0.0007*** | 13 (16) | 17 (14) | 0.6949 |
| Chronic kidney disease | 4 (1) | 2 (1) | 0.8159 | 8 (10) | 1 (1) | 0.0030** |
| Previous cancer | 15 (5) | 5 (3) | 0.2181 | 14 (17) | 1 (1) | 0.0000*** |
| Cancer excluding non-melanoma skin cancer (last 5 years) | 5 (2) | 2 (1) | 0.6012 | 6 (7) | 0 (0) | 0.0028** |
| Lymphoma | 2 (1) | 0 (0) | 0.266 | 0 (0) | 0 (0) | NA |
| HBV | 18 (6) | 4 (2) | 0.0818 | 12 (11) | 7 (5) | 0.1684 |
| HCV | 8 (3) | 2 (1) | 0.102 | 4 (4) | 2 (1) | 0.3579 |
| HIV | 0 (0) | 0 (0) | 0.2617 | 2 (2) | 0 (0) | 0.1881 |
| Previous biologic treatments, n (% overall) | ||||||
| Secukinumab (Cosentyx®) | 211 (59) | 128 (52) | 0.0283* | – | – | |
| Ixekizumab (Taltz®) | 101 (28) | 93 (38) | – | – | ||
| Brodalumab (Kyntheum®) | 39 (11) | 16 (7) | – | – | ||
| Bimekizumab (Bimzelx®) | 8 (2) | 8 (3) | – | – | ||
| Secukinumab (Cosentyx®) | – | – | 62 (48) | 62 (39) | 0.1869 | |
| Ixekizumab (Taltz®) | – | – | 36 (28) | 46 (29) | ||
| Brodalumab (Kyntheum®) | – | – | 30 (23) | 51 (32) |
PASI, Psoriasis Area Severity Index; BMI, body mass index; GPP, generalized pustular psoriasis; COPD, chronic obstructive pulmonary disease; HBV, hepatitis B virus; HCV, hepatitis C virus; HIV, human immunodeficiency virus.
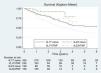
All-cause survival was statistically higher (log-rank test <0.05) in patients treated with IL17i or IL23i as first-line biologics vs those previously exposed to TNFi (Fig. 1). This finding persisted in the multivariable Cox regression model, which adjusted for potential confounders, including age, sex, body mass index (BMI), baseline PASI, number of comorbidities, presence of PsA, drug class, prior systemic therapies, and year of systemic treatment initiation. Quantitatively, according to this model, the instantaneous risk (hazard ratio, HR) of treatment discontinuation was 1.80 (95%CI, 1.32–2.44) times higher in TNFi-experienced patients treated with IL17i vs IL17i-naïve patients, and more than 3.30 (95%CI, 1.29–8.47) times higher in TNFi-experienced patients treated with IL23i vs IL23i-naïve patients.
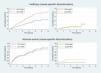
Discontinuation due to specific causes – namely inefficacy or AEs – did not show significant differences, except among patients receiving IL17i (Fig. 2). In the IL17i-treated group, the risk of discontinuation due to inefficacy was higher in TNFi-experienced patients vs naïve patients (HR, 2.25; 95%CI, 1.45–3.50).
AE rates were generally similar between groups, except in specific cases (Tables 2 and 3). In the adjusted model, among patients treated with IL17 inhibitors, all-type infections were more frequent in biologic-naïve patients vs those previously treated with TNFi. Conversely, in patients treated with IL23 inhibitors, all-type infection rates were higher among those with prior TNFi exposure. In both treatment groups, no statistically significant differences were observed when evaluating serious AEs or serious infections. With regard to overall AE rates, these were higher in patients previously treated with TNFi who subsequently received IL17i or IL23i vs naïve patients, although this difference reached statistical significance only in the IL23i group. The cumulative incidence rate of AE-related discontinuation was also higher in IL17i- or IL23i-treated patients with prior TNFi exposure, although statistical significance was not reached (Fig. 2).
Rate of adverse events according to treatment used (IL17 inhibitors or IL23 inhibitors) or preceded by TNF inhibitors, for the most frequent organ-system groups.
| iIL17 | iIL17/iTNF | iIL23 | iIL23/iTNF | |||||
|---|---|---|---|---|---|---|---|---|
| No. of events | Incidence rate (per 1000 PY) | No. of events | Incidence rate (per 1000 PY) | No. of events | Incidence rate (per 1000 PY) | No. of events | Incidence rate (per 1000 PY) | |
| Person-years of exposure | 971 | 496 | 199 | 251 | ||||
| All adverse events | 566 | 583 (537–633) | 293 | 591 (527–662) | 67 | 336 (264–427) | 140 | 559 (474–659) |
| Serious adverse events | 39 | 40 (29–55) | 27 | 54 (37–79) | 9 | 45 (23–87) | 15 | 60 (36–99) |
| SOC category | ||||||||
| Infections (serious) | 5 | 5 (2–12) | 5 | 10 (4–24) | 1 | 5 (1–36) | 3 | 12 (4–37) |
| Infections (all) | 155 | 160 (136–187) | 53 | 107 (82–140) | 15 | 75 (45–125) | 44 | 176 (131–236) |
| Musculoskeletal and connective tissue disorders | 50 | 51 (39–68) | 45 | 91 (68–121) | 8 | 40 (20–80) | 10 | 40 (21–74) |
| Skin and subcutaneous tissue disorders | 56 | 58 (44–75) | 23 | 46 (31–70) | 7 | 35 (17–74) | 14 | 56 (33–94) |
| Investigations | 34 | 35 (25–49) | 35 | 71 (51–98) | 6 | 30 (14–67) | 7 | 28 (13–59) |
| Gastrointestinal disorders | 32 | 33 (23–47) | 18 | 36 (23–58) | 3 | 15 (5–47) | 3 | 12 (4–37) |
| General disorders | 33 | 34 (24–48) | 15 | 30 (18–50) | 1 | 5 (1–36) | 5 | 20 (8–48) |
| Surgical and medical procedures | 26 | 27 (18–39) | 16 | 32 (20–53) | 3 | 15 (5–47) | 7 | 28 (13–59) |
| Neoplasms (benign, malignant, unspecified) | 24 | 25 (17–37) | 14 | 28 (17–48) | 3 | 15 (5–47) | 10 | 40 (21–74) |
| Neoplasms (malignant) | 7 | 7 (3–15) | 5 | 10 (4–24) | 1 | 5 (1–36) | 3 | 12 (4–37) |
Incidence rate ratios of adverse events according to treatment used (IL17 inhibitors or IL23 inhibitors) or preceded by TNF inhibitors.
| SOC group | IL17i vs IL17i/TNFi | IL23i vs IL23i/TNFi | ||
|---|---|---|---|---|
| Crude IRR | Adjusted IRRa | Crude IRR | Adjusted IRRa | |
| All adverse events | 1.01 (0.81–1.26) | 0.94 (0.75–1.19) | 1.66 (1.09–2.55)* | 1.85 (1.18–2.9)** |
| Serious adverse events | 1.36 (0.72–2.55) | 1.54 (0.67–3.56) | 1.33 (0.48–3.69) | 2.15 (0.67–6.94) |
| Serious infections | 1.96 (0.57–6.77) | 2.93 (0.6–14.26) | 2.39 (0.25–22.81) | 1.37 (0.15–12.82) |
| Infections (all) | 0.67 (0.46–0.98)* | 0.57 (0.36–0.88)** | 2.33 (1.33–4.11)** | 2.05 (1.13–3.72)** |
| Musculoskeletal and connective tissue disorders | 1.76 (1.12–2.77)* | 1.51 (0.96–2.39) | 0.99 (0.31–3.2) | 1.64 (0.51–5.27) |
| Skin and subcutaneous disorders | 0.8 (0.48–1.34) | 0.78 (0.43–1.44) | 1.59 (0.52–4.89) | 1.85 (0.58–5.9) |
| Investigations | 2.01 (1.01–4.02)* | 1.43 (0.65–3.13) | 0.93 (0.28–3.09) | 0.81 (0.35–1.84) |
| GI disorders | 1.1 (0.48–2.5) | 1.12 (0.53–2.34) | 0.8 (0.17–3.8) | 0.3 (0.02–4.44) |
| General disorders | 0.89 (0.41–1.95) | 0.84 (0.39–1.84) | 3.98 (0.44–36.25) | 2.66 (0.25–28.61) |
| Surgical and medical procedures | 1.2 (0.61–2.38) | 1.44 (0.68–3.03) | 1.86 (0.37–9.36) | 1.36 (0.34–5.54) |
The main reason for using TNFi as the first-line biological treatment in psoriasis is the lower economic cost of biosimilars vs originator molecules. However, there is limited evidence on whether this strategy may influence response to subsequent lines of therapy in real-world psoriasis management. We present a real-life study analyzing whether prior exposure to a TNFi may affect the survival of IL17i or IL23i therapies in patients with psoriasis. Overall treatment survival was higher in patients treated with IL17i or IL23i as first-line therapy vs those previously exposed to TNFi. This finding was consistent in both crude and adjusted analyses. One possible explanation is that the patient populations differ. Patients starting IL17i or IL23i as first-line therapy had shorter disease duration and greater severity (measured by PASI) than those previously treated with TNFi – factors that may influence treatment persistence, particularly disease duration. Psoriatic arthritis (PsA) may also affect treatment survival.10 In our study, a higher proportion of IL17i-treated patients had PsA vs those on IL23i, but no significant differences were observed between the compared cohorts (naïve vs TNFi-experienced). However, among IL23i-naïve patients, PsA prevalence was lower than in those on IL23i after TNFi, possibly because IL23 inhibitors were approved for PsA more recently. Another explanation is that treatment failure with a prior TNFi may select for a poorer-responder population. Nonetheless, clinical trials of IL17i and IL23i have not shown differential efficacy based on prior biological exposure.11–14 When analyzing discontinuation due to specific causes (inefficacy or adverse events), only IL17i-treated patients showed a higher risk of discontinuation due to inefficacy after prior TNFi exposure vs biologic-naïve IL17i users.
Regarding AE rates, infections of all types were more frequent in biologic-naïve patients receiving IL17i, whereas among IL23i recipients, infection rates were higher in those previously treated with TNFi after adjusting for covariates. Similarly, overall AE rates were higher in TNFi-experienced patients subsequently on IL23i. This may reflect selection bias in the choice of biological class, given the differing baseline characteristics of the populations. However, no statistically significant differences were observed in serious AEs or serious infections. Importantly, differences in infection rates did not affect treatment survival, as discontinuation due to AEs was higher in TNFi-experienced patients for both IL17i and IL23i.
Several studies have examined biological treatment survival in psoriasis, but few have specifically analyzed the persistence of IL17i or IL23i following TNFi vs their first-line use. A large French population cohort study of 8693 psoriasis patients examined second-line therapies and found that IL23i had greater persistence regardless of prior biologic exposure; TNFi persistence was lowest across all groups. No differences in second-line persistence were found between IL12/23i and IL17i, but the study did not compare first-line vs post-TNFi use of IL17i or IL23i as we did.15
Other smaller studies (not including all current biologics) found greater second-line persistence for IL12/23i than TNFi, but similarly did not examine the impact of prior TNFi on IL17i or IL23i persistence.16–18
A more recent analysis from the British BADBIR registry – including 16,122 biological treatment cycles – found greater survival with guselkumab and lower survival with adalimumab vs ustekinumab. Prior biological exposure, nail involvement, PsA, and ethnicity all influenced treatment survival. When analyzing second-line survival after adalimumab failure, only ustekinumab showed significantly reduced survival. When adalimumab failure was due to AEs, second-line survival decreased for ustekinumab and secukinumab.10
A single-center retrospective study evaluated IL17i and IL23i effectiveness after adalimumab failure in 1053 psoriasis patients. Among them, 92 had prior adalimumab exposure and 659 were biologic-naïve. The study found no significant differences in IL17i or IL23i effectiveness at 16, 28, or 52 weeks between naïve and adalimumab-experienced patients.19 However, the study did not assess long-term response beyond one year, and <100 patients had prior adalimumab exposure.
When considering treatment duration in addition to effectiveness, the most economical option is not always the most efficient. An Italian observational study showed that some biologics were more cost-effective than biosimilar adalimumab. Simultaneously assessing treatment cost and expected long-term response may offer valuable guidance to clinicians and payers.20
Thus, while starting with a TNFi may not affect the speed or short- to medium-term efficacy of later, more targeted biologics, our findings suggest that prior TNFi exposure is associated with reduced duration of treatment response – particularly for IL17i – partially differing from some observations in the British registry. Moreover, the choice of biologic class may influence the long-term course of psoriatic disease, especially regarding comorbidity prevention such as PsA. A large U.S. retrospective cohort study of 15,501 psoriasis patients found that IL12/23i and IL23i significantly reduced the risk of developing inflammatory arthritis vs TNFi. IL17i did not demonstrate a significant reduction vs TNFi.21
Despite being a multicenter, prospective, real-world study, our work has several limitations. Although treatment persistence can serve as an indirect measure of effectiveness and safety, it is influenced by physician- and patient-related factors that are difficult to quantify, though these should affect all groups equally. The sample size is also limited. Although agents were grouped by biological class to increase statistical power, individual agents within a class differ in effectiveness, safety, and persistence. Similarly, as an observational study, causal relationships cannot be established; we can only conclude that prior TNFi exposure was associated with reduced persistence of IL17i and IL23i therapies in plaque psoriasis, with no differences in serious AEs or serious infections. The impact on safety was limited: although overall AE rates and AE-driven discontinuations were higher in TNFi-experienced patients, these did not reach statistical significance. Further studies are required to confirm these findings and better understand their clinical implications.
FundingThe BIOBADADERM project is promoted by Fundación Piel Sana of the Spanish Academy of Dermatology and Venereology (AEDV), which receives financial support from the Spanish Agency of Medicines and Medical Devices (AEMPS) and pharmaceutical companies (Abbott/AbbVie, Almirall, Amgen, Biogen, Boehringer Ingelheim, Bristol Myers Squibb, Janssen, and UCB). The following companies have collaborated in the past (LEO Pharma, Novartis Pharma, Lilly, MSD, and Pfizer). The collaborating pharmaceutical companies were not involved in any of the following: study design or conduct; data collection, management, analysis, or interpretation; manuscript preparation, review, or approval; or the decision to submit the manuscript for publication.
Conflicts of interestRaquel Rivera-Díaz has participated as an advisor, speaker, and investigator and has received support to attend scientific meetings from AbbVie, Almirall, Amgen, Boehringer, Bristol Myers Squibb (BMS), Incyte, Johnson & Johnson, LEO Pharma, Lilly, Novartis, and UCB.
Alicia González-Quesada has participated as an advisor, speaker, and investigator and has received support to attend scientific meetings from AbbVie, Almirall, Amgen, BMS, Incyte, LEO Pharma, Novartis, Lilly, UCB, and Pfizer.
José Manuel Carrascosa has participated as an advisor, speaker, and investigator and has received support to attend scientific meetings from AbbVie, Almirall, Amgen, Boehringer, BMS, Incyte, Johnson & Johnson, LEO Pharma, Lilly, Novartis, UCB, Sandoz, Gebro, Pfizer, Sanofi, and Galderma.
Isabel Belinchón-Romero has received consulting and/or speaker fees and/or has participated in clinical trials sponsored by companies manufacturing drugs used for the treatment of psoriasis, including Janssen Pharmaceuticals Inc, Almirall, Lilly, AbbVie, Novartis, Celgene, Biogen, Amgen, LEO Pharma, Pfizer-Wyeth, BMS, UCB, Sandoz, and MSD.
Esteban Daudén has served or currently serves as an advisory board member or consultant and has received grants, research support, clinical trial participation fees, and speaker honoraria from Abbott/AbbVie, Almirall, Amgen, Biogen, Celgene, Janssen-Cilag, LEO Pharma, Lilly, MSD, Novartis, Pfizer, UCB, Bristol Myers Squibb, and Boehringer Ingelheim.
D. P. Ruiz-Genao has participated as an advisor, speaker, and investigator and has received support to attend scientific meetings from AbbVie, Almirall, Amgen, Boehringer, BMS, Johnson & Johnson, LEO Pharma, Lilly, Novartis, and UCB.
Ofelia Baniandrés Rodríguez has participated as an advisor, speaker, and investigator and/or has received support to attend scientific meetings from AbbVie, Almirall, Amgen, Boehringer, BMS, Johnson & Johnson, LEO Pharma, Lilly, Novartis, and UCB.
Marta Ferran has participated as a speaker, investigator, or advisor and/or has received support to attend scientific meetings from AbbVie, Almirall, Amgen, BMS, Johnson & Johnson, LEO Pharma, Lilly, Novartis, and UCB.
Pablo de la Cueva has participated as an advisor, investigator, and/or speaker for AbbVie, Almirall, Amgen, Astellas, Beiersdorf, Biogen, BMS, Boehringer, Celgene, Gebro, Johnson & Johnson, LEO Pharma, Lilly, MSD, Novartis, Pfizer, Roche, Sandoz, Sanofi, SVR, Takeda, and UCB.
Lourdes Rodríguez Fernández-Freire has participated as an advisor, speaker, and investigator and has received support to attend scientific meetings from AbbVie Laboratories, Almirall SA, Amgen, Boehringer, BMS, Janssen-Cilag, LEO Pharma, Lilly, MSD, Novartis, Pfizer-Wyeth, and UCB.
Almudena Mateu has participated as a speaker, investigator, or advisor and/or has received support to attend scientific meetings from AbbVie, Almirall, BMS, Johnson & Johnson, LEO Pharma, Lilly, Novartis, Sanofi Aventis, and UCB.
Josep Riera-Monroig has participated as an advisor, investigator, and/or speaker for AbbVie, Almirall, Amgen, Janssen, LEO Pharma, Eli Lilly, Novartis, UCB Pharma, and BMS.
Mariano Ara-Martín has participated as an advisor, speaker, and investigator and has received support to attend scientific meetings from AbbVie, Almirall, Amgen, Boehringer, BMS, Johnson & Johnson, LEO Pharma, Lilly, Novartis, Pfizer, and UCB.
María Teresa Abalde Pintos has served as an advisory board member, participated in clinical trials, and received speaker honoraria from Abbott/AbbVie, Almirall, Amgen, Celgene, Janssen-Cilag, LEO Pharma, Lilly, Novartis, UCB, and Boehringer Ingelheim.
Mónica Roncero-Riesco has participated in clinical trials, received speaker honoraria, and received support to attend scientific meetings from AbbVie, Almirall, Novartis, UCB, Lilly, Janssen, and Amgen.
Carmen García-Donoso has participated as a speaker, investigator, or advisor and/or has received support to attend scientific meetings from AbbVie, Almirall, BMS, Johnson & Johnson, LEO Pharma, Lilly, Novartis, and UCB.
Ignacio García-Doval has received travel grants to attend scientific meetings from AbbVie, MSD, Pfizer, and Sanofi.
Miguel Ángel Descalzo declared no conflicts of interest whatsoever.
The authors thank the patients and all collaborating investigators participating in BIOBADADERM.