Reduced minimal erythema dose (MED) is an abnormal erythematous reaction to light according to the skin phototype, which is determined by phototest. MED is reduced or abnormal in some photodermatoses. However, we have not found information about reduced MED in patients with solar urticarial (SU), a condition which causes hives after sun exposure.
ObjectiveTo determine MED in a series of patients with SU.
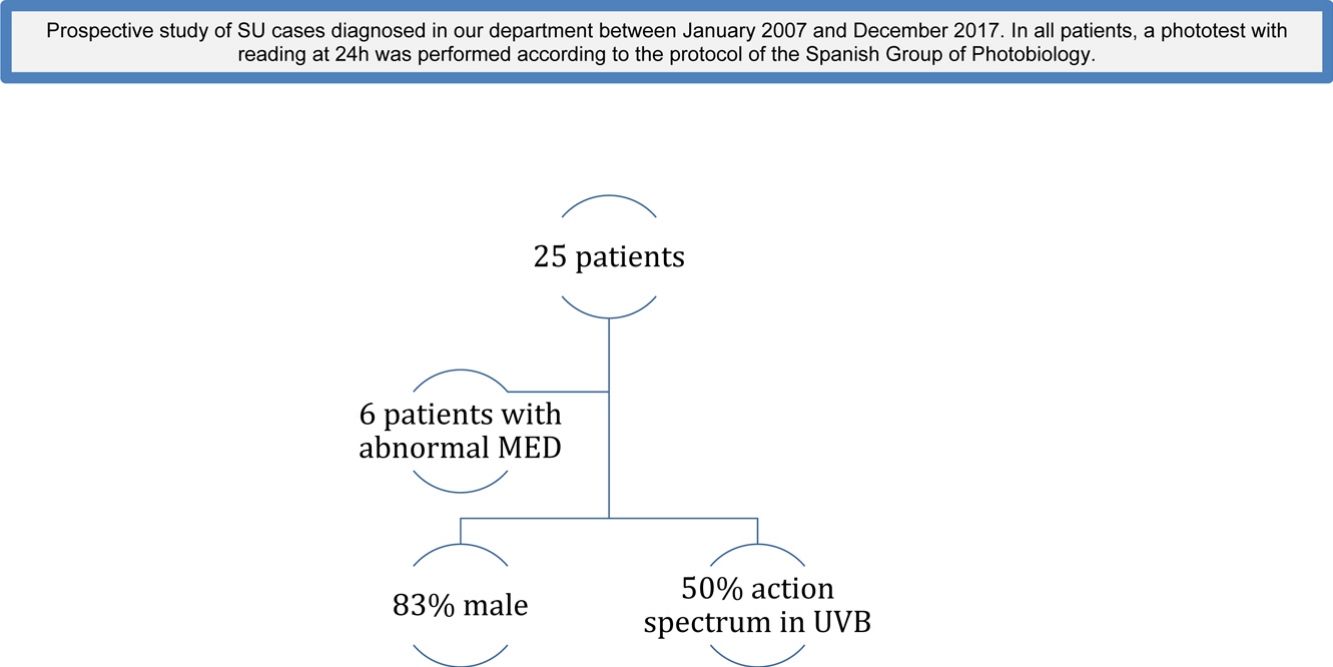
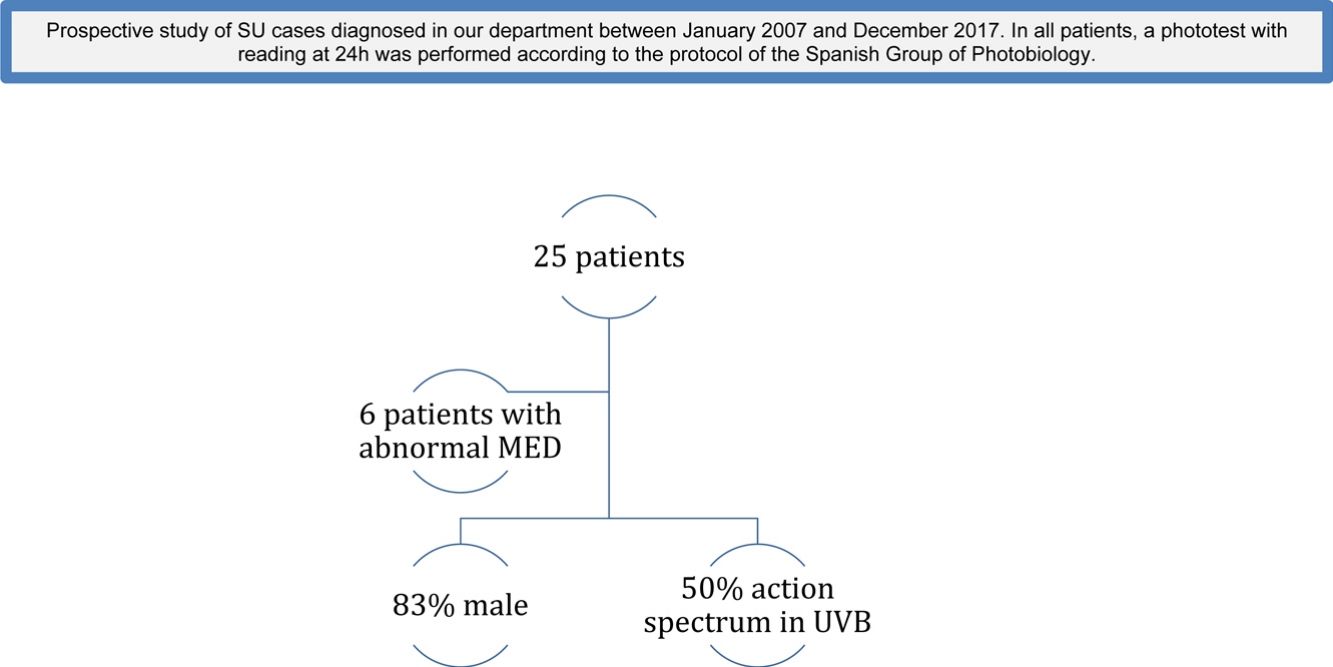
MethodsWe conducted a prospective study of SU cases diagnosed in our department between January 2007 and December 2017, either by anamnesis, provocation with natural sunlight or provocation with artificial light sources. In all patients, a phototest with reading at 24 h was performed according to the protocol of the Spanish Group of Photobiology. Variables related to the patient (age, sex, phototype), disease (time of evolution, action spectrum) and others related to possible reduced MED (autoantibodies, phototoxic medication) were collected.
ResultsTwenty-five patients were studied. Six patients (24%) had abnormal MED. Eighty-three percent of patients with abnormal MED were men, and 50% had action spectrum in UVB.
ConclusionAbnormal MED can be seen in up to a fourth of the patients with SU. This could have implications in the selection of patients and protocols for treatment with phototherapy.
La dosis eritematosa mínima (DEM) reducida es una reacción anormal a la luz según el fototipo de piel y que se determina mediante fototest. La DEM es reducida o anormal en algunas fotodermatosis. Sin embargo, no hemos encontrado información sobre la DEM reducida en pacientes con urticaria solar (US), enfermedad que cursa con urticaria tras la exposición al sol.
ObjetivoDeterminar la DEM en una serie de pacientes con US.
MétodosLlevamos a cabo un estudio prospectivo de casos de US diagnosticados en nuestro departamento entre enero de 2007 y diciembre de 2017, a través de anamnesis o por provocación mediante exposición a la luz solar natural o a fuentes de luz artificial. De acuerdo con el protocolo del Grupo Español de Fotobiología, a las 24 horas se llevó a cabo la lectura del fototest en todos los pacientes. Se recopilaron las variables relativas al paciente (edad, sexo, fototipo), enfermedad (tiempo de evolución, espectro de activación) y otras relacionadas con la posible DEM reducida (autoanticuerpos, medicación fototóxica).
ResultadosSe estudiaron 25 pacientes, de los cuales, seis (24%) presentaron una DEM anormal, el 83% de ellos eran hombres, y el 50% mostraba el espectro de acción en el rango de la radiación UVB.
ConclusiónHasta en una cuarta parte de los pacientes con US se puede observar la DEM anormal. Esta circunstancia podría tener implicaciones en la selección de los pacientes y en los protocolos para el tratamiento con fototerapia.
Solar urticaria (SU) is a rare inducible chronic urticaria that also belongs to the group of idiopathic photodermatoses. In SU, transient wheals appear within 5 to 10 minutes of exposure to ultraviolet (UV) and/or visible radiation, resolving over a period of minutes to a few hours1.
SU diagnosis can be usually made through anamnesis, although it is widely recommended to conduct a photoprovocation, which consists of repeatedly exposing an area of skin to a pre-established dose of radiation with the aim of reproducing the clinical lesions being investigated 2,3. The study of Minimal Erythema Dose (MED) must be performed through phototesting, which involves exposing an area of skin to a known dose of ultraviolet B radiation (UVB) and then observing, recording, and interpreting the erythematous response at the irradiated site after a pre-established time (generally 24 hours). Similarly, the threshold for provoking wheals is established by exposing the individual to incremental doses of light radiation and is called the Minimal Urticaria Dose (MUD). Finally, photoprovocation is also useful to determine the action spectrum (wavelengths which trigger SU, which can be more than one in a single patient) 4.
It has been reported that a large percentage of photodermatoses (up to 68% in some series) could present a phototest with an MED that is considered normal5. Furthermore, some reviews report that SU is a photodermatosis that usually shows normal MED but without any support apart from sporadic cases 3,6,7. On the other hand, in spite of the lack of data of abnormal MED in the general population, its frequency in different series ranges from 5% to 16% of the total patients referred for phototesting 8,9. Lastly, we must also take into account that the mechanisms involved in MED are unknown and they might be related to constitutional factors such as age, gender or phototype. Currently, the influence of MED in the course of SU remains unexplored.
OBJECTIVETo evaluate the presence of abnormal MED in patients with SU. Secondly, try to analyse its association with the baseline characteristics of our patients and the type of SU.
MATERIALS AND METHODSWe undertook a prospective study of SU cases diagnosed in our department from January 2007 to December 2017. The inclusion criteria were: patients diagnosed with SU according to anamnesis, provocation with natural sunlight or with artificial light sources (photoprovocation) who had their MED measured according to the phototesting protocol established by the Spanish Group of Photobiology 4,10.
The following data were collected from each patient: gender, age at the time of diagnosis, time since SU onset, co-morbidities, skin phototype, current medication, serum IgE, antinuclear antibodies (ANA), anti Ro antibodies (Anti-Ro) and results of the phototesting, including action spectrum and MED.
The MED study was carried out following the recommendations made by the Spanish Society of Photobiology. A Simulator Multiport 601, Solar Light ® (Philadelphia, Pennsylvania) and a Gigatest UVB broadband, Medisun ® (Brühl, Germany) were used to perform the phototest. Using the Solar Simulator with broadband UVB, MEDs under 7, 19, 27 and 38mj/cm2 were considered pathologic for skin phototypes 1, 2, 3 and 4 respectively, while using UVA, MEDs under 18, 24 and 24mj/cm2 were considered pathologic for skin phototypes 2, 3 and 4 respectively 10. These values were selected as they represent the expected normal MEDs for our country, but there is not international consensus of what are the normal values.
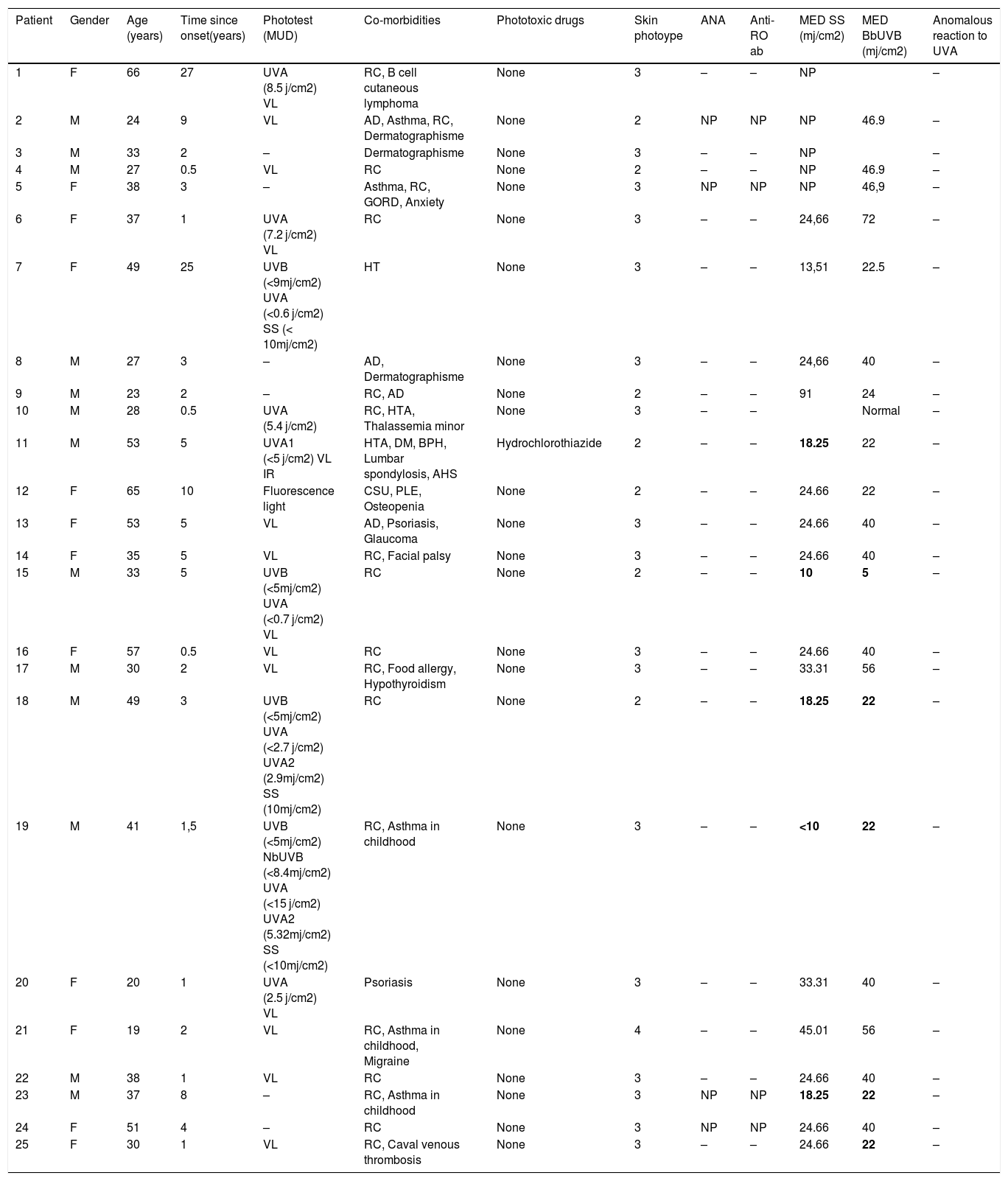
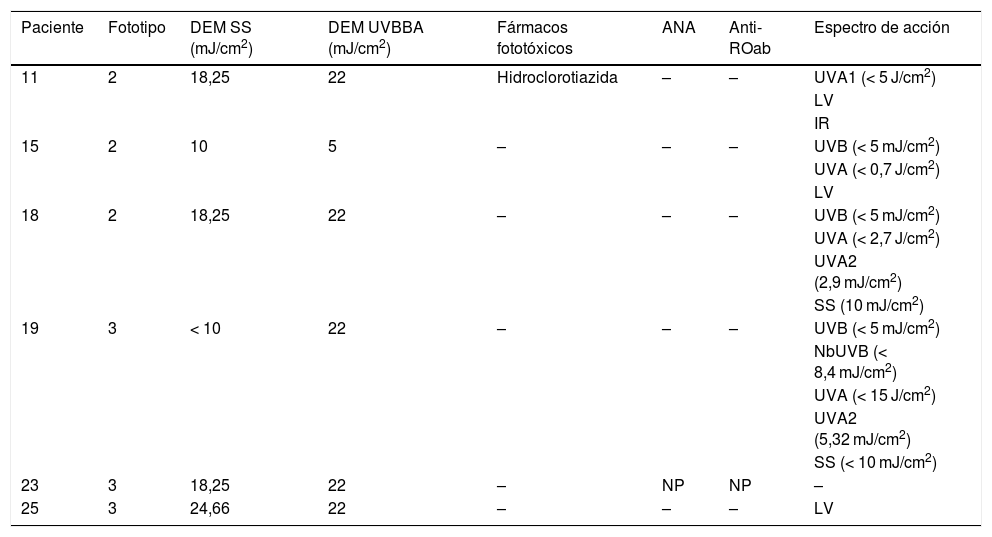
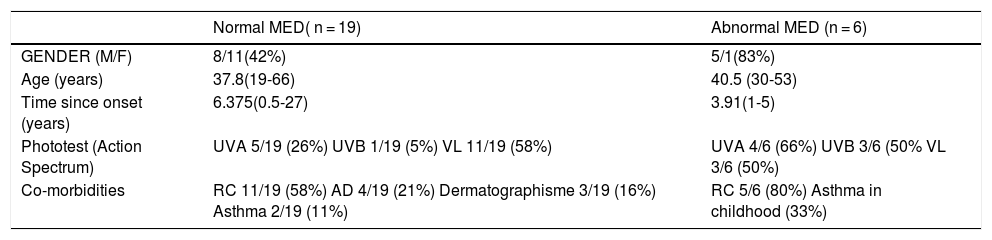
RESULTSTwenty-five patients were included (Table1). Sixty-four percent were men, and mean age was 39.7 years, Sixty-four percent of our patients had skin phototype III and the mean time since onset of disease was 5.9 years. None of the patients were positive for autoantibodies, one patient was under a potentially phototoxic drug (thiazides) (4%), and the most frequent co-morbidities were as follows: rhinoconjunctivitis (72%), asthma (20%) and atopic dermatitis (16%). The action spectrum was: visible light (58%), UVA (26%) and UVB (5%). None of the patients showed an anomalous reaction to UVA radiation. In our series, six patients (24%) presented an abnormal MED according to their phototype (Table 2). Out of this six patients, five were men, mean age was 40.5 years, three had skin phototype III and the mean time since onset of disease was 3.9 years. None of the patients had autoantibodies (1 unknown), one was under treatment with a potentially phototoxic drug (17%), five presented concomitant rhinoconjunctivitis (83%) and three had action spectrum in UVB (50%). Comparison between the group of patients with abnormal MED and patients with normal MED is displayed in Table 3.
Summary of patients.
| Patient | Gender | Age (years) | Time since onset(years) | Phototest (MUD) | Co-morbidities | Phototoxic drugs | Skin photoype | ANA | Anti-RO ab | MED SS (mj/cm2) | MED BbUVB (mj/cm2) | Anomalous reaction to UVA |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 66 | 27 | UVA (8.5 j/cm2) VL | RC, B cell cutaneous lymphoma | None | 3 | – | – | NP | – | |
| 2 | M | 24 | 9 | VL | AD, Asthma, RC, Dermatographisme | None | 2 | NP | NP | NP | 46.9 | – |
| 3 | M | 33 | 2 | – | Dermatographisme | None | 3 | – | – | NP | – | |
| 4 | M | 27 | 0.5 | VL | RC | None | 2 | – | – | NP | 46.9 | – |
| 5 | F | 38 | 3 | – | Asthma, RC, GORD, Anxiety | None | 3 | NP | NP | NP | 46,9 | – |
| 6 | F | 37 | 1 | UVA (7.2 j/cm2) VL | RC | None | 3 | – | – | 24,66 | 72 | – |
| 7 | F | 49 | 25 | UVB (<9mj/cm2) UVA (<0.6 j/cm2) SS (< 10mj/cm2) | HT | None | 3 | – | – | 13,51 | 22.5 | – |
| 8 | M | 27 | 3 | – | AD, Dermatographisme | None | 3 | – | – | 24,66 | 40 | – |
| 9 | M | 23 | 2 | – | RC, AD | None | 2 | – | – | 91 | 24 | – |
| 10 | M | 28 | 0.5 | UVA (5.4 j/cm2) | RC, HTA, Thalassemia minor | None | 3 | – | – | Normal | – | |
| 11 | M | 53 | 5 | UVA1 (<5 j/cm2) VL IR | HTA, DM, BPH, Lumbar spondylosis, AHS | Hydrochlorothiazide | 2 | – | – | 18.25 | 22 | – |
| 12 | F | 65 | 10 | Fluorescence light | CSU, PLE, Osteopenia | None | 2 | – | – | 24.66 | 22 | – |
| 13 | F | 53 | 5 | VL | AD, Psoriasis, Glaucoma | None | 3 | – | – | 24.66 | 40 | – |
| 14 | F | 35 | 5 | VL | RC, Facial palsy | None | 3 | – | – | 24.66 | 40 | – |
| 15 | M | 33 | 5 | UVB (<5mj/cm2) UVA (<0.7 j/cm2) VL | RC | None | 2 | – | – | 10 | 5 | – |
| 16 | F | 57 | 0.5 | VL | RC | None | 3 | – | – | 24.66 | 40 | – |
| 17 | M | 30 | 2 | VL | RC, Food allergy, Hypothyroidism | None | 3 | – | – | 33.31 | 56 | – |
| 18 | M | 49 | 3 | UVB (<5mj/cm2) UVA (<2.7 j/cm2) UVA2 (2.9mj/cm2) SS (10mj/cm2) | RC | None | 2 | – | – | 18.25 | 22 | – |
| 19 | M | 41 | 1,5 | UVB (<5mj/cm2) NbUVB (<8.4mj/cm2) UVA (<15 j/cm2) UVA2 (5.32mj/cm2) SS (<10mj/cm2) | RC, Asthma in childhood | None | 3 | – | – | <10 | 22 | – |
| 20 | F | 20 | 1 | UVA (2.5 j/cm2) VL | Psoriasis | None | 3 | – | – | 33.31 | 40 | – |
| 21 | F | 19 | 2 | VL | RC, Asthma in childhood, Migraine | None | 4 | – | – | 45.01 | 56 | – |
| 22 | M | 38 | 1 | VL | RC | None | 3 | – | – | 24.66 | 40 | – |
| 23 | M | 37 | 8 | – | RC, Asthma in childhood | None | 3 | NP | NP | 18.25 | 22 | – |
| 24 | F | 51 | 4 | – | RC | None | 3 | NP | NP | 24.66 | 40 | – |
| 25 | F | 30 | 1 | VL | RC, Caval venous thrombosis | None | 3 | – | – | 24.66 | 22 | – |
AD: Atopic dermatitis, AHS: Apnea hypopnea syndrome, ANA: Antinuclear antibodies, Anti-ROab: Anti- RO antibodies, BPH: Benign prostatic hypertrophy, CSU: Chronic spontaneous urticaria, DM: Diabetes mellitus, GORD: Gastro-oesophageal reflux disease, HT: Hypertension, MED: Minimal erythema dose, MUD: Minimal urticarial dose, NbUVB: narrow-band ultraviolet B, NP: Not performed, PLE: Polymorphous light eruption, RC: Rhinoconjunctivitis, SS: Solar simulator, UVA: Ultraviolet A, BbUVB: Broadband ultraviolet B, VL: Visible light.
Patients with abnormal ME.
| Paciente | Fototipo | DEM SS (mJ/cm2) | DEM UVBBA (mJ/cm2) | Fármacos fototóxicos | ANA | Anti-ROab | Espectro de acción |
|---|---|---|---|---|---|---|---|
| 11 | 2 | 18,25 | 22 | Hidroclorotiazida | – | – | UVA1 (< 5 J/cm2) |
| LV | |||||||
| IR | |||||||
| 15 | 2 | 10 | 5 | – | – | – | UVB (< 5 mJ/cm2) |
| UVA (< 0,7 J/cm2) | |||||||
| LV | |||||||
| 18 | 2 | 18,25 | 22 | – | – | – | UVB (< 5 mJ/cm2) |
| UVA (< 2,7 J/cm2) | |||||||
| UVA2 (2,9 mJ/cm2) | |||||||
| SS (10 mJ/cm2) | |||||||
| 19 | 3 | < 10 | 22 | – | – | – | UVB (< 5 mJ/cm2) |
| NbUVB (< 8,4 mJ/cm2) | |||||||
| UVA (< 15 J/cm2) | |||||||
| UVA2 (5,32 mJ/cm2) | |||||||
| SS (< 10 mJ/cm2) | |||||||
| 23 | 3 | 18,25 | 22 | – | NP | NP | – |
| 25 | 3 | 24,66 | 22 | – | – | – | LV |
ANA: Antinuclear antibodies, Anti-ROab: Anti- RO antibodies, IR: Infrared, MED: Minimal erythema dose, NbUVB: narrow-band ultraviolet B, NP: Not performed, SS: Solar simulator, UVA: Ultraviolet A, UVB: Ultraviolet B, VL: Visible light.
Comparison of patients with abnormal MED to normal MED.
| Normal MED( n = 19) | Abnormal MED (n = 6) | |
|---|---|---|
| GENDER (M/F) | 8/11(42%) | 5/1(83%) |
| Age (years) | 37.8(19-66) | 40.5 (30-53) |
| Time since onset (years) | 6.375(0.5-27) | 3.91(1-5) |
| Phototest (Action Spectrum) | UVA 5/19 (26%) UVB 1/19 (5%) VL 11/19 (58%) | UVA 4/6 (66%) UVB 3/6 (50% VL 3/6 (50%) |
| Co-morbidities | RC 11/19 (58%) AD 4/19 (21%) Dermatographisme 3/19 (16%) Asthma 2/19 (11%) | RC 5/6 (80%) Asthma in childhood (33%) |
AD: Atopic dermatitis, MED: Minimal erythema dose, RC: Rhinoconjunctivitis, SS: Solar simulator, UVA: Ultraviolet A, UVB: Ultraviolet B, VL: Visible light.
In our study, 24% (6/25) of the patients had an abnormal MED, lower than expected by their phototype. We have not found case series in the literature reporting similar results. The outcome found in our series suggests that patients with SU could have more associated photosensitivity with its condition than other photodermatoses 9,10. Apart from triggering solar urticaria in some of them, patients with SU and reduced MED did not show anomalous unexpected reactions to UVA radiation.
Eighty-three per cent of our patients with abnormal MED were men. Comparing with a study carried out to determine MED in psoriatic patients before starting phototherapy, it also showed that an abnormal reduced MED was more frequent in men and older patients 11. Moreover, it has also been reported that in 110 patients with polymorphic light eruption, a reduced MED for UVB was present in 43% of men and 0% of women 12. However in SU patients, the role of gender in MED was previously unreported. The time of disease evolution until diagnosis was shorter in the patients with abnormal MED: 3.9 years compared with 6.4 years, which could mean that they have a more symptomatic disease and look for medical attention earlier. Regarding to drugs, one of our patients was taking hydrochlorothiazide and was reluctant to take another phototest without it. The fact that this patient showed an abnormal MED only with the solar simulator could mean that reduced MED was triggered by UVA radiation, which is supposed to be more common in drug phototoxicity 13. The most frequently involved action spectrum was different in our two groups (Table 3). Visible radiation and UVA were the most frequent in the group with normal MEDs, similarly to the reports of action spectrums in SU in our country 3. However, UVB was part of the action spectrum in 50% of the patients with abnormal MED, which is an uncommon finding that could indicate that these patients are prone to have an abnormal MED. Autoantibodies do not seem to play a role in the reduced MED in our patients since none of the patients tested were positive.
In conclusion, abnormal MED in our series can be seen in a fourth of the patients with SU, mostly in men and in patients with an action spectrum in UVB. This could have implications in the selection of patients and protocols for treatment with phototherapy.
The limitations of our study are, first that we do not have a control group of healthy patients. And second, that with online six patients with low MED in our series, all conclusions must be taken cautiously.
Conflict of interestDr. De Argila has been Clinical Advisor and participated in clinical trials promoted by Novartis. The rest of the authors declare that they do not have conflicts of interest.
Please cite this article as: Rodríguez-Jiménez P, Chicharro P, Reolid A, Muñoz-Aceituno E, De Argila D. Estudio de la dosis eritematosa mínima en una serie de urticaria solar. Actas Dermosifiliogr. 2021;112:546–550.