Stretch marks are common lesions that affect areas under stress, especially common in pregnant women and adolescents. Despite its prevalence, its treatment and prevention are a challenge in Dermatology.
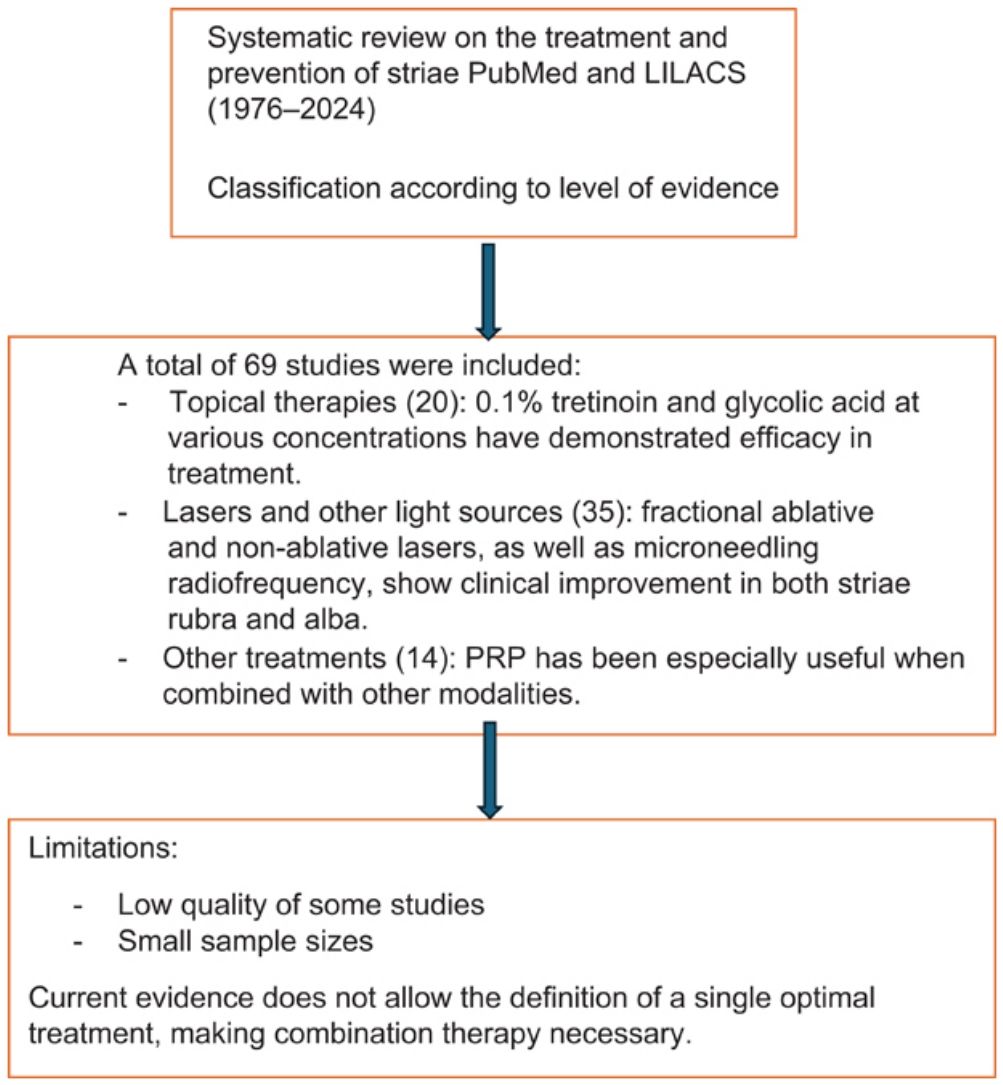
Material and methodsSystematic review of the literature published in PubMed and LILACS (1976–2024). The articles were classified according to their scientific evidence (level 1, randomized controlled studies; level 5, clinical cases).
ResultsA total of 69 articles were evaluated: 20 on topical treatments, 35 on lasers and energy devices, and 14 on other therapies. Tretinoin at 0.1% and glycolic acid at different concentrations demonstrated clinical improvement, especially in recent stretch marks. Ablative and non-ablative lasers and radiofrequency with microneedles presented good results. Other treatments, such as PRP, are useful in combination.
ConclusionsCurrent evidence does not allow defining a single treatment; some works are of low quality and with small samples. The combination of treatments helps to improve results.
Stretch marks are common cutaneous lesions associated with mechanical, hormonal, and genetic factors.1,2 They present as red stretch marks (striae rubra) in early stages and white stretch marks (striae alba) in later stages. These lesions affect areas exposed to tension, such as the abdomen, thighs, and breasts, and are more prevalent in pregnant women, adolescents, and individuals with higher phototypes.3
From a histologic standpoint, striae rubra demonstrate inflammation, collagen fiber thickening, and reduced elastic fibers,4,5 whereas striae alba show dermal atrophy and rupture with decreased vascularization.
Despite their high prevalence, their treatment and prevention remain a therapeutic challenge in Dermatology.
This study is based on the hypothesis that at least one scientifically supported, effective therapeutic option may currently be identified for the treatment of striae.
The endpoints of this study are:
- 1.
To evaluate and synthesize the available evidence on the various therapeutic modalities used in the management of cutaneous striae.
- 2.
To determine whether one or several options could be positioned as first-line therapy.
- 3.
To provide a practical clinical guide and identify potential areas for future research.
We conducted a systematic review of the literature published in PubMed from January 1976 to February 2024 and LILACS from January 1986 to February 2024 was performed on the treatment and prevention of striae.
Search terms were selected according to MeSH and DeCS vocabularies and included: “striae,” “striae distensae,” “stretch marks,” “striae gravidarum,” “striae rubrae,” “striae albae,” and “treatment.”
Studies included clinical trials, cohort studies, controlled studies, and isolated case reports. Exclusion criteria were articles not published in English or Spanish, animal or in vitro studies, letters to the editor, narrative or systematic reviews, meta-analyses, and duplicate publications.
Each included study was assigned a level of evidence according to its scientific quality: Level 1 for randomized controlled trials, level 2 for randomized comparative studies, level 3 for nonrandomized comparative studies, level 4 for case series, and level 5 for isolated case reports.
ResultsIncluded and excluded studiesA total of 364 records were identified in PubMed and 36 in LILACS. After screening titles and abstracts, a total of 325 articles were excluded for not meeting inclusion criteria. The full text of 69 articles was reviewed and categorized by therapeutic approach: (A) topical treatments (20 articles), (B) lasers and light-based therapy (35 articles), and (C) other therapies (14 articles).
- A)
Results of topical treatments
- 1)
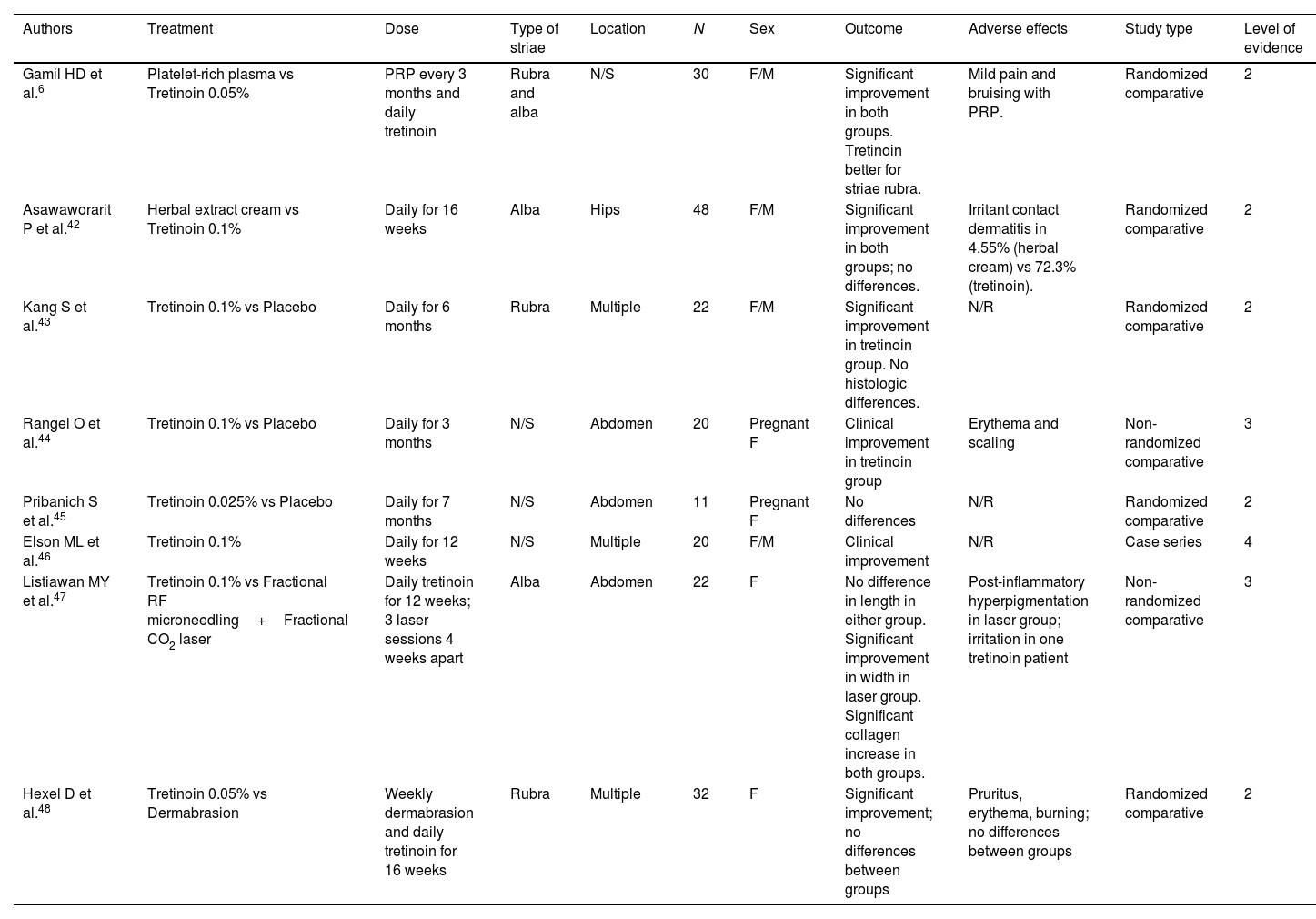
Tretinoin (Table 1)
A vitamin A derivative, tretinoin promotes neoangiogenesis, collagen formation, and cellular differentiation. Most studies used a concentration of 0.1%. All reported significant clinical improvement except at 0.025%. A 12-week regimen was generally required to achieve results. Adverse effects were mild and rare, including local irritation and desquamation.
Summary of studies on the treatment of striae with tretinoin.
| Authors | Treatment | Dose | Type of striae | Location | N | Sex | Outcome | Adverse effects | Study type | Level of evidence |
|---|---|---|---|---|---|---|---|---|---|---|
| Gamil HD et al.6 | Platelet-rich plasma vs Tretinoin 0.05% | PRP every 3 months and daily tretinoin | Rubra and alba | N/S | 30 | F/M | Significant improvement in both groups. Tretinoin better for striae rubra. | Mild pain and bruising with PRP. | Randomized comparative | 2 |
| Asawaworarit P et al.42 | Herbal extract cream vs Tretinoin 0.1% | Daily for 16 weeks | Alba | Hips | 48 | F/M | Significant improvement in both groups; no differences. | Irritant contact dermatitis in 4.55% (herbal cream) vs 72.3% (tretinoin). | Randomized comparative | 2 |
| Kang S et al.43 | Tretinoin 0.1% vs Placebo | Daily for 6 months | Rubra | Multiple | 22 | F/M | Significant improvement in tretinoin group. No histologic differences. | N/R | Randomized comparative | 2 |
| Rangel O et al.44 | Tretinoin 0.1% vs Placebo | Daily for 3 months | N/S | Abdomen | 20 | Pregnant F | Clinical improvement in tretinoin group | Erythema and scaling | Non-randomized comparative | 3 |
| Pribanich S et al.45 | Tretinoin 0.025% vs Placebo | Daily for 7 months | N/S | Abdomen | 11 | Pregnant F | No differences | N/R | Randomized comparative | 2 |
| Elson ML et al.46 | Tretinoin 0.1% | Daily for 12 weeks | N/S | Multiple | 20 | F/M | Clinical improvement | N/R | Case series | 4 |
| Listiawan MY et al.47 | Tretinoin 0.1% vs Fractional RF microneedling+Fractional CO2 laser | Daily tretinoin for 12 weeks; 3 laser sessions 4 weeks apart | Alba | Abdomen | 22 | F | No difference in length in either group. Significant improvement in width in laser group. Significant collagen increase in both groups. | Post-inflammatory hyperpigmentation in laser group; irritation in one tretinoin patient | Non-randomized comparative | 3 |
| Hexel D et al.48 | Tretinoin 0.05% vs Dermabrasion | Weekly dermabrasion and daily tretinoin for 16 weeks | Rubra | Multiple | 32 | F | Significant improvement; no differences between groups | Pruritus, erythema, burning; no differences between groups | Randomized comparative | 2 |
N, number of participants; F, female; M, male; N/R, not reported; N/S, not specified; PRP, platelet-rich plasma; RF, radiofrequency. Note: References outside the range [1–41] are included as Supplementary data.
Of note, the study by Gamil6 compared daily 0.05% tretinoin for 3 months with monthly platelet-rich plasma (PRP) injections. Greater improvement was observed in red vs white striae, with superior results and higher patient satisfaction in the PRP group.
- 2)
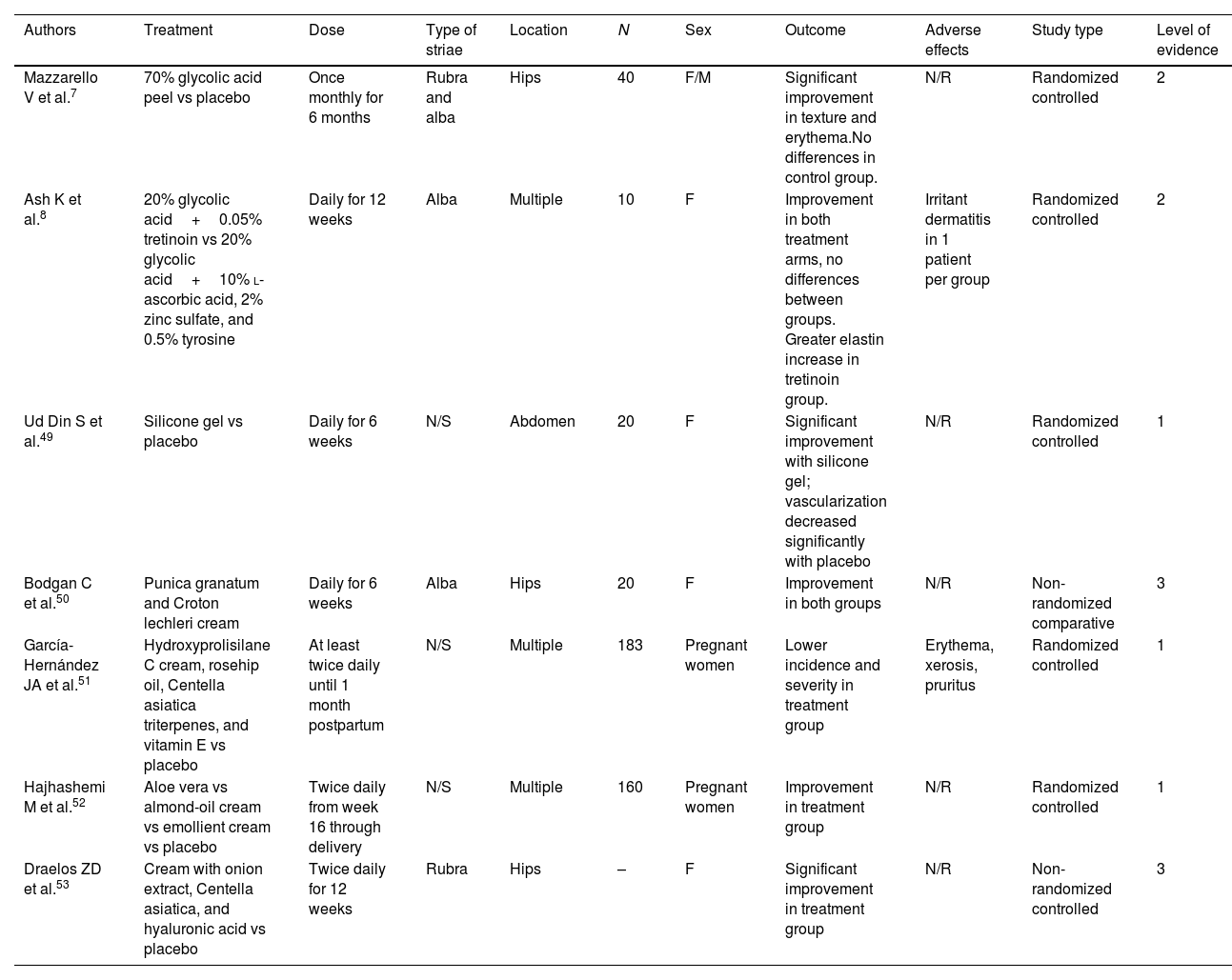
Glycolic acid (Table 2)
An alpha-hydroxy acid involved in cellular repair, glycolic acid accelerates collagen regeneration through fibroblast stimulation and cytokine release by keratinocytes.
Summary of studies on the treatment of striae with glycolic acid, cocoa butter, and olive oil.
| Authors | Treatment | Dose | Type of striae | Location | N | Sex | Outcome | Adverse effects | Study type | Level of evidence |
|---|---|---|---|---|---|---|---|---|---|---|
| Mazzarello V et al.7 | 70% glycolic acid peel vs placebo | Once monthly for 6 months | Rubra and alba | Hips | 40 | F/M | Significant improvement in texture and erythema.No differences in control group. | N/R | Randomized controlled | 2 |
| Ash K et al.8 | 20% glycolic acid+0.05% tretinoin vs 20% glycolic acid+10% l-ascorbic acid, 2% zinc sulfate, and 0.5% tyrosine | Daily for 12 weeks | Alba | Multiple | 10 | F | Improvement in both treatment arms, no differences between groups. Greater elastin increase in tretinoin group. | Irritant dermatitis in 1 patient per group | Randomized controlled | 2 |
| Ud Din S et al.49 | Silicone gel vs placebo | Daily for 6 weeks | N/S | Abdomen | 20 | F | Significant improvement with silicone gel; vascularization decreased significantly with placebo | N/R | Randomized controlled | 1 |
| Bodgan C et al.50 | Punica granatum and Croton lechleri cream | Daily for 6 weeks | Alba | Hips | 20 | F | Improvement in both groups | N/R | Non-randomized comparative | 3 |
| García-Hernández JA et al.51 | Hydroxyprolisilane C cream, rosehip oil, Centella asiatica triterpenes, and vitamin E vs placebo | At least twice daily until 1 month postpartum | N/S | Multiple | 183 | Pregnant women | Lower incidence and severity in treatment group | Erythema, xerosis, pruritus | Randomized controlled | 1 |
| Hajhashemi M et al.52 | Aloe vera vs almond-oil cream vs emollient cream vs placebo | Twice daily from week 16 through delivery | N/S | Multiple | 160 | Pregnant women | Improvement in treatment group | N/R | Randomized controlled | 1 |
| Draelos ZD et al.53 | Cream with onion extract, Centella asiatica, and hyaluronic acid vs placebo | Twice daily for 12 weeks | Rubra | Hips | – | F | Significant improvement in treatment group | N/R | Non-randomized controlled | 3 |
N, number of participants; F, female; M, male; N/R, not reported; N/S, not specified. Note: References outside the range [1–41] are included as Supplementary data.
Two major studies are noteworthy. Mazzarello et al.7 compared glycolic acid 70% monthly for 6 months vs placebo in 40 patients with red and white striae. Clinical improvement was reported in texture and erythema, along with increased melanin detected by spectrophotometry. Ash et al.8 compared glycolic acid 20%+tretinoin 0.05% vs a combination of glycolic acid 20%, l-ascorbic acid 10%, zinc sulfate 2%, and tyrosine 0.5% in 10 women with white striae, without significant differences across groups.
- 3)
Cocoa butter and olive oil:
Cocoa butter has emollient properties, as does olive oil, which is rich in vitamin E.
Studies9–13 evaluated their usefulness in preventing striae in pregnant women vs placebo or other emollient creams. No significant differences were observed in any study.
- 4)
Silicone gel and other topical agents:
Summarized in Table 3.
- B)
Results of laser-based treatments
Summary of studies on the treatment of striae with silicone gels and other topical therapies.
| Authors | Treatment | Dose | Type of striae | Location | N | Sex | Outcome | Adverse effects | Study type | Level of evidence |
|---|---|---|---|---|---|---|---|---|---|---|
| Sobhi MR et al.14 | Fractional CO2 vs MRF | 5 sessions, 4 weeks apart, 2 passes/session | N/S | Multiple | 17 | F | No significant differences | Post-inflammatory hyperpigmentation with CO2 | Non-randomized comparative | 3 |
| Seong GH et al.15 | Fractional CO2 vs CO2+MRF vs MRF | 3 sessions, 4 weeks apart, 1 pass/session | N/S | Abdomen | 19 | F (phototypes III–IV) | Significant improvement in the combined group | Hyperpigmentation and pruritus in combined and CO2 groups | Randomized comparative | 2 |
| Khater MH et al.16 | Fractional CO2 vs MRF | 3 sessions, 4 weeks apart | Rubra and alba | Abdomen and thighs | 20 | F (phototypes III–IV) | Clinical improvement; increased collagen, elastic fibers, and epidermal thickness in 90% with microneedling vs 50% with CO2 | Post-inflammatory hyperpigmentation in CO2 group | Non-randomized comparative | 3 |
| Soliman M et al.17 | Fractional CO2 vs microneedling (dermaroller) | 3 sessions, 4 weeks apart | N/S | Multiple | 33 | F/M | Greater satisfaction and effectiveness with CO2 | Post-inflammatory hyperpigmentation in CO2 group | Non-randomized comparative | 3 |
| Saki N et al.18 | Fractional CO2 vs microneedling | 4 sessions, 4 weeks apart | N/S | N/S | 40 | F/M | Reduction in striae width with no group differences | Not reported | Randomized comparative | 2 |
| Elmorsy EH et al.19 | Fractional CO2 vs carboxytherapy | CO2: 6 sessions, 4 weeks apart; Carboxy: 6 sessions, 2 weeks apart | Rubra and alba | Abdomen | 40 | F | Improvement with both therapies; no significant differences | CO2: erythema, crusts, pain, PIH; Carboxy: erythema, bruising, tingling | Randomized comparative | 2 |
| Crocco EI et al.54 | Fractional CO2 vs control | 4 sessions with increasing intensity (80–110 mJ/MTZ), 4 weeks apart | Alba | Abdomen | 13 | F | Significant increase in collagen fibers and epidermal thickness; non-significant increase in elastic fibers | Erythema, edema, crusting | Controlled comparative | 1 |
| Cho SB et al.55 | Fractional CO2 | 2 sessions, 4 weeks apart | Alba | Thighs | 1 | F | Clinical improvement | None | Case report | 5 |
| Nouri K et al.56 | CO2 vs PDL 585nm vs control | Single session; assessment at 4 and 20 weeks | N/S | Abdomen | 4 | F (phototypes IV & VI) | PDL: No improvement in phototype IV; worsening hyperpigmentation in VI. CO2: persistent erythema in IV, hyperpigmentation in VI | Hyperpigmentation | Controlled comparative | 1 |
| Preclaro IA et al.57 | CO2+PRP vs CO2+placebo | 4 sessions, 4 weeks apart; combined group: CO2 followed by PRP | N/S | Abdomen | 16 | F | Clinical and subjective improvement in CO2+PRP; no significant differences | Not reported | Controlled comparative | 1 |
| Shin JU et al.58 | CO2 vs CO2+(succinylated atelocollagen or placebo) vs collagen or placebo | 3 sessions, 4 weeks apart; follow-up 1 month after completion | Alba | N/S | 14 | F | Significant differences between collagen and placebo in irradiated groups; and between collagen and placebo without CO2; epidermal thickening in all groups | Pruritus, erythema; one case of psoriasis | Controlled comparative | 1 |
N, number of participants; F, female; M, male; N/R, not reported; N/S, not specified. Note: References outside the range [1–41] are included as Supplementary data.
- 1)
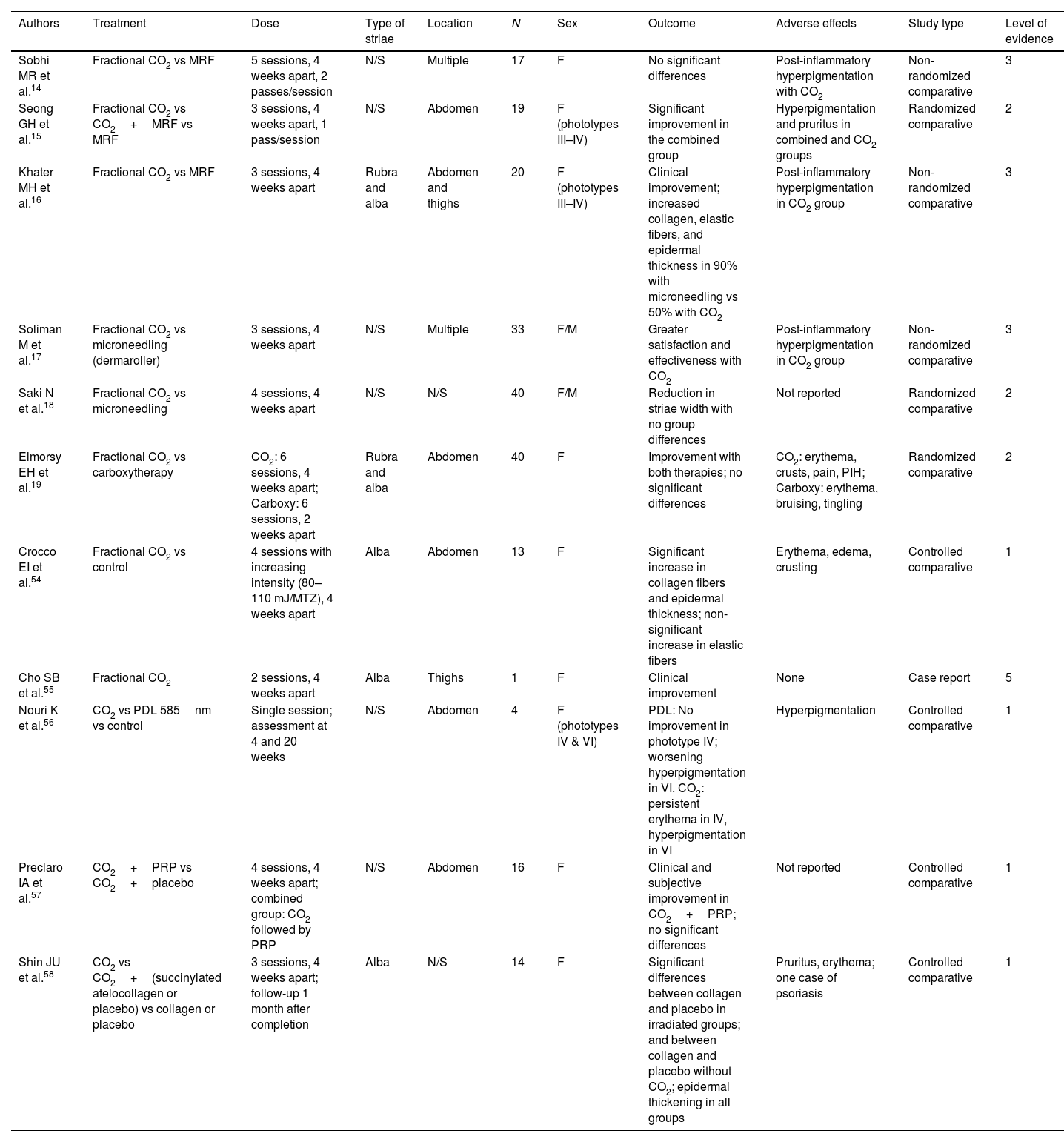
CO2 Laser (Table 4)
Table 4.Summary of studies on the treatment of striae using CO2 lasers.
Authors Treatment Dose Type of striae Location N Sex Outcome Adverse effects Study type Level of evidence Kim BJ et al.20 NAFL 1550nm vs control 1 session; evaluation at 4 and 8 weeks Alba Thighs 6 F Improvement in erythema, pigmentation, and partial elasticity; increased epidermal thickness, collagen, and elastic fibers histologically Pain, hyperpigmentation Non-randomized comparative 3 Stotland et al.21 NAFL 1550nm 6 sessions, 2–3 weeks apart Alba Abdomen, thighs, buttocks 20 F 26–50% improvement in 63%; < 25% improvement in dyschromia in 50%; 26–50% texture improvement in 50% Not reported Case series 4 de Angelis F et al.25 NAFL 1540nm 2–4 sessions, 4–6 weeks apart; 2–3 passes; long-term evaluation Rubra and alba Multiple 51 F/M 50% improvement at 6 months; increased dermal collagen/elastin; no recurrence at 18–24 months Erythema, edema, PIH Case series 4 Park KK et al.22 NAFL 1550nm vs control 3 sessions, 4 weeks apart N/S Abdomen 17 F (phototypes IV–VI) Significant clinical improvement of striae and DLQI vs control Pruritus, scaling, erythema; no PIH Controlled comparative 1 Katz TM et al.23 NAFL 1550nm 3–5 sessions, 4 weeks apart Rubra Thighs and breasts 2 F Clinical improvement Erythema, edema Case series 4 Clementoni MT et al.24 NAFL 1565nm 3 sessions, 4–5 weeks apart N/S Multiple 12 F/M Clinical improvement; reduced depression and discoloration Transient erythema, edema Case series 4 Oliveira Alves R et al.26 NAFL 1540nm 3–6 sessions Rubra Arms, thighs 4 F/M Improvement after 3rd session Transient erythema, edema Case series 4 Tay YK et al.27 NAFL 1450nm (6mm, 40ms; 4, 8, 12J) vs control 3 sessions, 6 weeks apart Rubra and alba Multiple 11 F/M (phototypes IV–VI) No improvement vs control Session erythema; PIH (64%) Controlled comparative 1 Meningaud JP et al.28 NAFL 2940nm 6 sessions, 4 weeks apart N/S N/S 20 F/M Increased skin thickness, elasticity, and skin quality Erythema during session Case series 4 Wanitphakdeedecha R et al.29 NAFL 2940nm 2 sessions, 4 weeks apart; 400mJ SP+2.2J/cm2 smooth N/S Multiple 29 F/M Significant improvement in both groups; no differences in roughness, smoothness, surface Transient PIH in dark phototypes Randomized comparative 2 Kaewkes A et al.30 Fractional picosecond laser 1064nm 4 sessions, 4 weeks apart Alba Abdomen 20 F (phototypes IV–V) Significant texture improvement at 1 and 6 months; increased melanin at 1-month follow-up PIH (2 cases) Case series 4 Tang Z et al.59 NAFL 1565nm vs MRF 3 sessions, 6 weeks apart Alba Abdomen 14 F MRF significantly more effective clinically; both effective overall; no difference in satisfaction or melanin; more neocollagenesis with MRF Significantly more pain with MRF Non-randomized comparative 3 Gungor S et al.60 1064nm Nd:YAG LP vs 2940nm Er:YAG 3 sessions, 4 weeks apart Rubra and alba Abdomen, arm (1), lumbar (2) 20 F No clinical improvement in alba, though histologic changes present; neither treatment useful clinically No complications with 1064nm; erythema and PIH with 2940nm Non-randomized comparative 3 Cao Y et al.61 Beta-glucan vs vehicle vs NAFL 1565nm+vehicle vs NAFL 1565nm+beta-glucan 3 sessions, 4 weeks apart; topicals twice daily×12 weeks Alba Abdomen 64 F Greater improvement with NAFL than beta-glucan; histology also favored NAFL Not reported Controlled comparative 1 Zaleski-Larson LA et al.62 Picosecond NAFL 1064/532nm vs NAFL 1565nm 3 sessions, 3 weeks apart Alba Abdomen 20 F Significant texture improvement with both; no density differences; picosecond laser less painful and faster healing Erythema, pain Non-randomized comparative 3 Naspolini AP et al.63 1340nm NAFL vs microneedling 5 sessions, 4 weeks apart Alba Abdomen 20 F (phototype III–IV) Improvement without significant group differences; increased collagen/elastin in both Erythema, pruritus; NAFL also caused PIH and crusting Non-randomized comparative 3 Gauglitz GG et al.64 NAFL 2940nm vs PDL 5 sessions, 4 weeks apart Rubra Axillae 2 M Improvement in texture and color on Er:YAG side PIH (1) Case series 4 N, number of participants; F, female; M, male; N/R, not reported; N/S, not specified; MRF, microneedling radiofrequency; PDL, pulsed dye laser. Note: References outside the range [1–41] are included as Supplementary data.
Used in fractional mode, CO2 lasers—due to their high affinity for water—create microscopic ablative and coagulative columns (microthermal zones, MTZ), with preserved tissue in between, promoting new collagen and elastin formation.
Most studies reported that fractional CO2 laser improved dermal collagen regeneration, increased skin thickness, and enhanced clinical appearance. Adverse effects were mild and expected: post-inflammatory hyperpigmentation, erythema, and crusting.
Comparisons between fractional CO2 and microneedling radiofrequency (MRF)—an energy-based device causing deep dermal thermal injury and growth factor release14–16—or microneedling alone17,18—showed variable results. MRF demonstrated clinically satisfactory outcomes, and in some studies, was superior to CO2.16
One study19 compared fractional CO2 laser with carboxytherapy (subcutaneous CO2 infusion inducing stretching and low-grade inflammation) in 40 women with abdominal striae. Both treatments produced improvement, with no significant differences in efficacy or adverse events.
- 2)
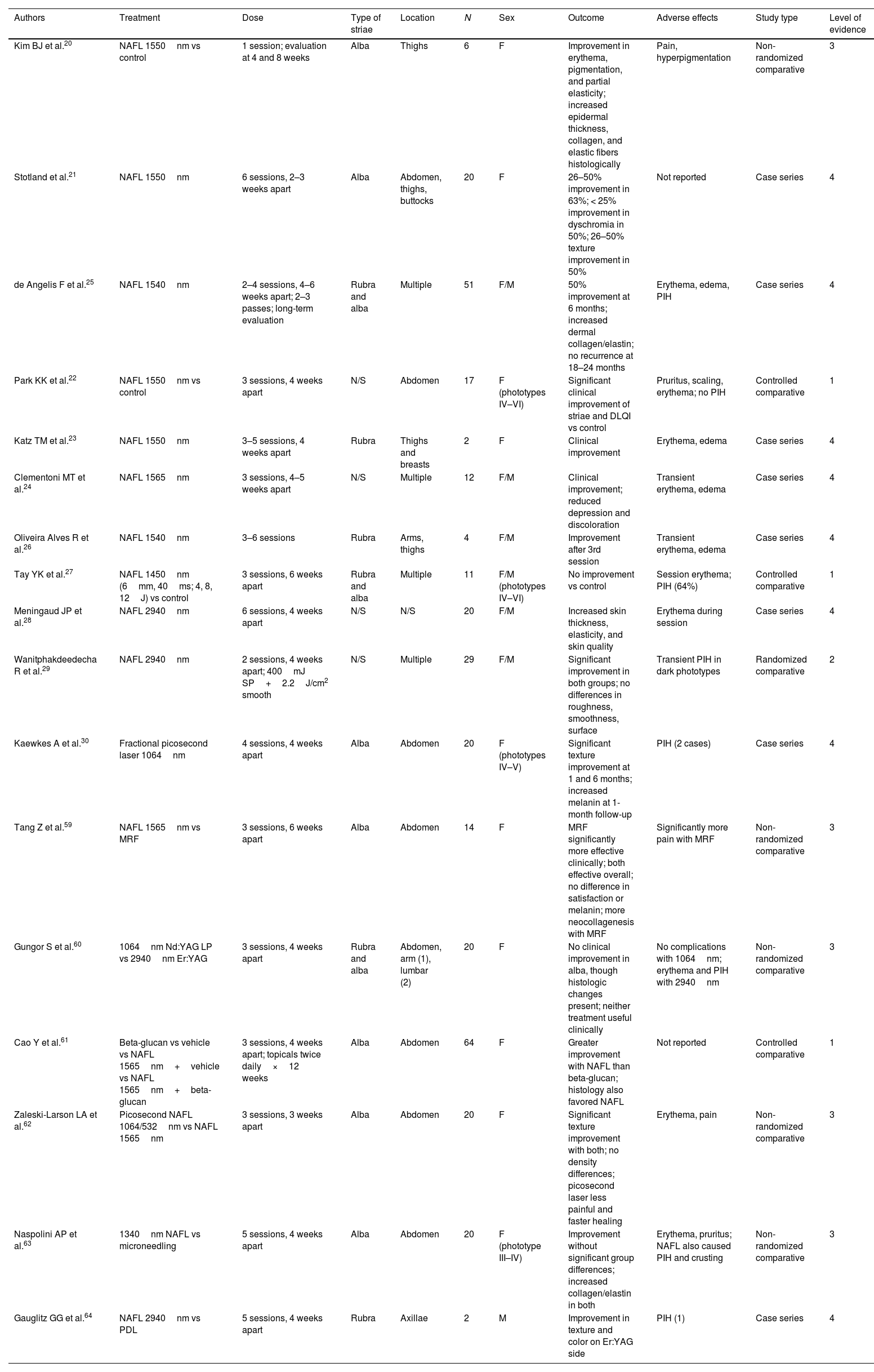
Nonablative fractional lasers (NAFL) (Table 5):
Due to lower water affinity, NAFL do not ablate epidermal layers. Tissue remodeling occurs by deep dermal heating, stimulating collagen and elastin regeneration without crust formation. NAFL are classified by wavelength (1450, 1540, 1550, 1064, 2940nm), which determines penetration depth.
Summary of studies on the treatment of striae using non-ablative fractional lasers (NAFL).
| Authors | Treatment | Type of striae | Location | N | Sex | Outcome | Adverse effects | Study type | Level of evidence |
|---|---|---|---|---|---|---|---|---|---|
| Jiménez GP et al.31 | PDL 585nm vs control | Rubra and alba | Multiple | 20 | F/M | Limited benefit in red striae; no change in white striae | Post-inflammatory hyperpigmentation in 1 phototype VI patient | Controlled comparative | 1 |
| McDaniel DH et al.32 | PDL 585nm vs control | Alba | Abdomen, thighs, breasts | 39 | F | Improvement with all parameters; best effectiveness with 3J, 10-mm spot | N/R | Case series | 4 |
| Al Dhalimi MA et al.34 | IPL 650nm vs 590nm | Rubra | N/S | 20 | F/M | Significant reduction with both; 590nm more effective | Transient erythema and pain; PIH (2), more with 590nm | Non-randomized comparative | 3 |
| Alexiades-Armenakas MR et al.35 | Excimer 308nm | Alba | Face, trunk, extremities | 31 | F/M | Colorimetric correction increased proportionally to number of sessions (> 9) | N/R | Controlled comparative | 1 |
| Shokeir H et al.33 | PDL 585nm vs IPL 565nm | Rubra and alba | Multiple | 20 | F/M | Significant improvement with both; better response in red striae | Transient erythema, pain, pruritus; PIH | Non-randomized comparative | 3 |
| Elsaie ML et al.65 | Nd:YAG 1064nm LP (10ms) 75 vs 100J/cm2 | Rubra and alba | Trunk, back, shoulders | 45 | F/M | Significant improvement with 100J/cm2 in both types; no differences between fluences in rubra | Pain | Non-randomized comparative | 3 |
| Suh DH et al.66 | Non-ablative RF+PDL | Rubra and alba | Abdomen | 37 | F/M | Subjective improvement and increased elasticity in most patients | Transient purpura (6); transient PIH (1) | Case series | 4 |
N, number of participants; F, female; M, male; N/R, not reported; N/S, not specified; MRF, microneedling radiofrequency; LP, long pulse; PDL, pulsed dye laser. Note: References outside the range [1–41] are included as Supplementary data.
Five studies evaluated 1550- and 1565-nm Er:Glass lasers,20–24 3 evaluated 1540-nm and 1450-nm diode lasers,25–27 2 evaluated 2940-nm Er:YAG,28,29 and 1 evaluated 1064-nm Nd:YAG.30 Although results varied, most reported partial improvement. One study27 using diode lasers at different energies found no benefit vs control. Adverse effects were mild, with post-inflammatory hyperpigmentation—particularly in darker skin types—being the most common.
- 3)
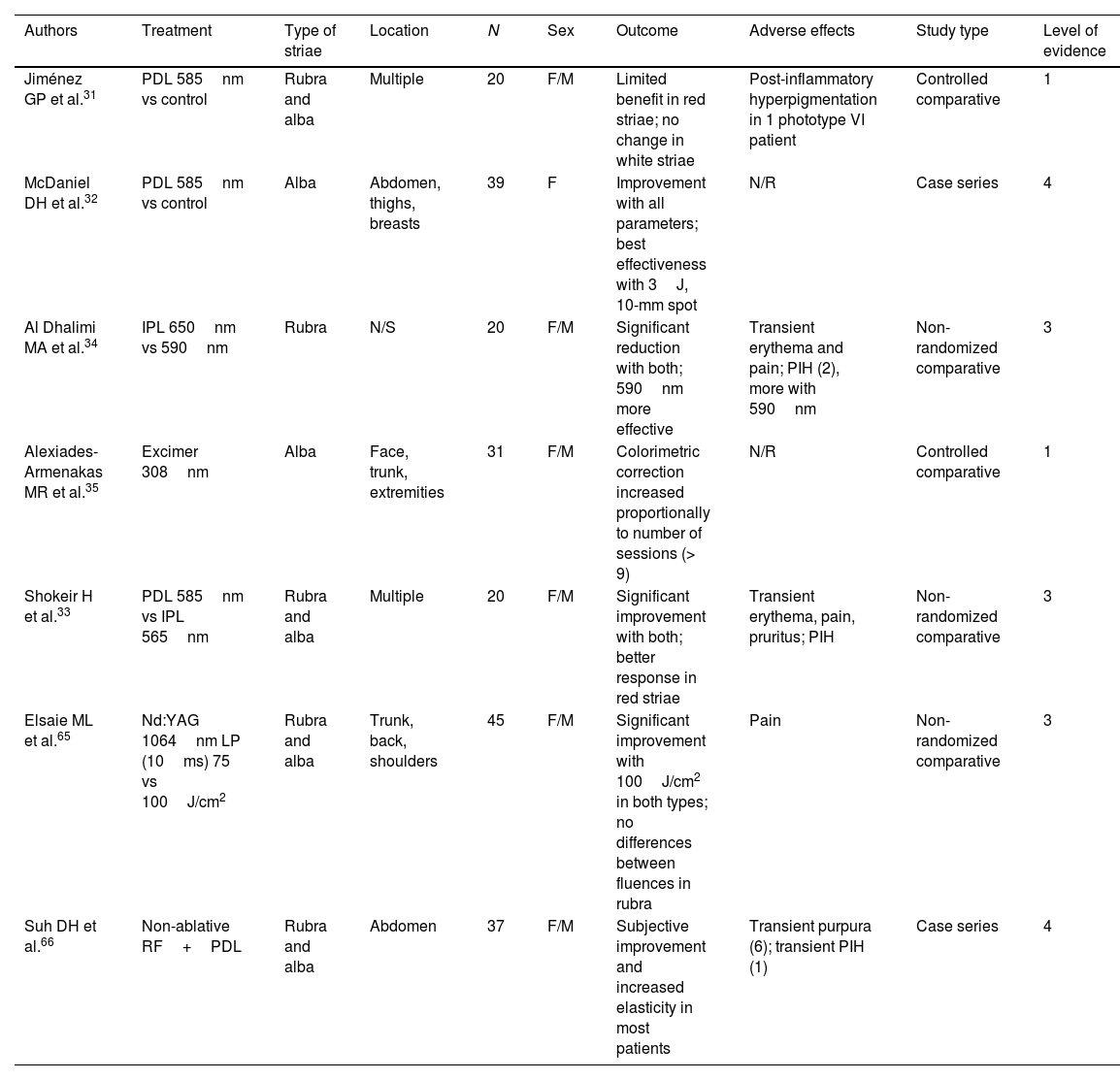
Vascular lasers (Table 6)
Several studies evaluated pulsed dye laser (PDL), long-pulse 1064-nm Nd:YAG, or intense pulsed light (IPL), targeting hemoglobin due to their wavelengths.
Summary of studies on the treatment of striae using vascular laser and other energy-based devices.
| Authors | Treatment | Dose | Type of striae | Location | N | Sex | Outcome | Adverse effects | Study type | Level of evidence |
|---|---|---|---|---|---|---|---|---|---|---|
| Suwanchinda A et al.41 | Cold atmospheric pressure plasma (CAP) | 5 sessions, every 15 days | N/S | N/S | 23 | F/M | Significant improvement after 1 session | Crusting and superficial wounds | Controlled comparative | 1 |
| Ahmed NA et al.38 | Carboxytherapy vs PRP vs Tripolar RF | 5 weekly sessions | Rubra and alba | Trunk and lower limbs | 45 | F | Improvement in all groups, no significant differences | Pain and ecchymosis (PRP); erythema (RF) | Randomized comparative | 2 |
| Hodeib AA et al.37 | Carboxytherapy vs PRP | 4 sessions every 3–4 weeks | Alba | Multiple | 20 | F/M | Improvement, no significant inter-group differences | Mild ecchymosis and pain | Non-randomized comparative | 3 |
| Manuskiatti W et al.67 | Tripolar RF | 6 weekly sessions | Rubra and alba | Abdomen and thighs | 17 | F | Improvement; no differences in texture 1 and 6 weeks after therapy | N/R | Case series | 4 |
| Ibrahim ZAE et al.36 | PRP vs microdermabrasion vs PRP+microdermabrasion | 6 sessions every 15 days | Rubra and alba | Multiple | 68 | F/M | PRP and PRP+microdermabrasion superior to microdermabrasion alone | Pain, ecchymosis; worsening with PRP in 3 cases | Randomized comparative | 2 |
| Ferreira ACR et al.68 | Galvanopuncture vs microdermabrasion vs control | 10 weekly sessions | Alba | Buttocks | 48 | F | Improvement without significant inter-group differences | Pain | Randomized controlled | 1 |
| Nassar A et al.69 | Microneedling vs microdermabrasion+sonophoresis | Biweekly or monthly sessions | Rubra and alba | Thighs and legs | 40 | F | Significant improvement with microneedling | Transient erythema and PIH | Non-randomized comparative | 3 |
| Harmelin Y et al.70 | Bipolar RF vs IR-enhanced bipolar RF vs IR+RF vs control | 3 monthly sessions | N/S | Abdomen | 22 | F/M | No differences among active treatments or control | Transient pain related to RF | Controlled comparative | 1 |
| Montesi G et al.71 | Bipolar RF | 6–8 sessions, every 2 weeks | N/S | Abdomen, buttocks, scapulohumeral region | 30 | N/S | Improvement from second session onward | Transient ecchymosis; blisters (2) | Case series | 4 |
| Tian T et al.72 | RF vs tretinoin vs combination vs control | RF: 3 sessions every 3 months; tretinoin daily ×1 week | Rubra and alba | Abdomen | 18 | F | Significant improvement with combined treatment | Mild pain, erythema, edema (RF-related) | Controlled comparative | 1 |
| Luis-Montoya P et al.39 | Subcision vs tretinoin 0.1% vs combination | N/S | Alba | N/S | 14 | N/S | Reduction in width and clinical improvement in all 3 groups; no significant inter-group differences | Necrosis (3) with subcision | Non-randomized comparative | 3 |
| Sadick NS et al.40 | Narrowband UVB/UVA1 | 10 sessions, twice weekly | Alba | N/S | 14 | F/M | > 51% repigmentation> 50% hyperpigmentation | Erythema, hyperpigmentation | Case series | 4 |
| Costa DC de O et al.73 | Microneedling+5-FU vs 5-FU vs microneedling | 1 session, evaluated at 180 days | Alba | Buttocks | 18 | F/M, phototype III–V | Partial improvement | PIH with all treatments | Randomized comparative | 2 |
| Lima EVA de A et al.74 | Fractional microneedling RF | One session, 60-day follow-up | N/S | N/S | 8 | F | Partial improvement; high patient satisfaction | Transient PIH in 6 patients | Case series | 4 |
PDL, pulsed dye laser; IPL, intense pulsed light; RF, radiofrequency; N, number of participants; F, female; M, male; N/R, not reported; N/S, not specified. Note: References outside the range [1–41] are included as Supplementary data.
Two studies assessed PDL. The first31 showed modest improvement in red striae and no change in white striae. The second32 demonstrated improvement in white striae (red striae not included), with better outcomes using larger spot sizes and higher energies (10mm, 3J).
Shokeir et al.33 compared the outcomes of PDL vs IPL (565nm). Although PDL showed slightly greater improvement, both light sources demonstrated clinically significant improvement in striae width, with greater effects in more recent (red) and smaller striae. Al Dhalimi et al.34 compared 2 different IPL wavelengths (650nm and 590nm) for the management of striae rubra. Lower fluences were used at 590nm (up to 14.5J with 590nm and up to 15.5J with 650nm) to avoid adverse effects. They achieved greater improvement with 590nm, although with a higher rate of adverse events (erythema, pain, and post-inflammatory hyperpigmentation), since melanin acts as a competing chromophore for light devices with affinity for hemoglobin. Finally, Alexiades-Armenakas et al.35 studied the 308-nm excimer lamp for the treatment of striae alba, demonstrating improvement vs the untreated side using colorimetric analysis. These favorable results progressively approached those of the control group during 6-month follow-up, suggesting that maintenance treatment would be necessary.
- C)
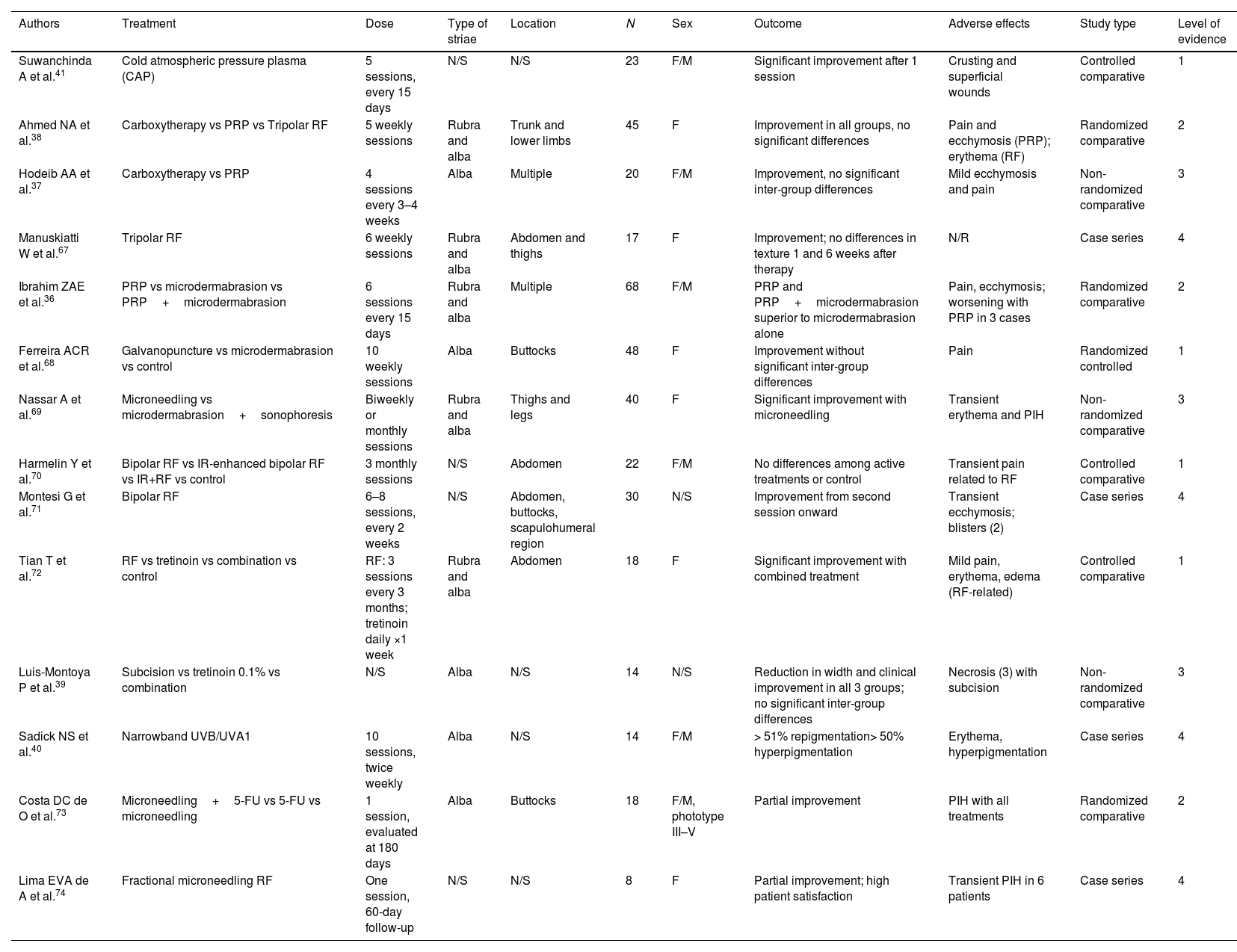
Other treatments (Table 7):
- 1)
Platelet-rich plasma (PRP), which contains a high concentration of growth factors and cytokines, has also been used for this indication, generally in combination with other techniques.
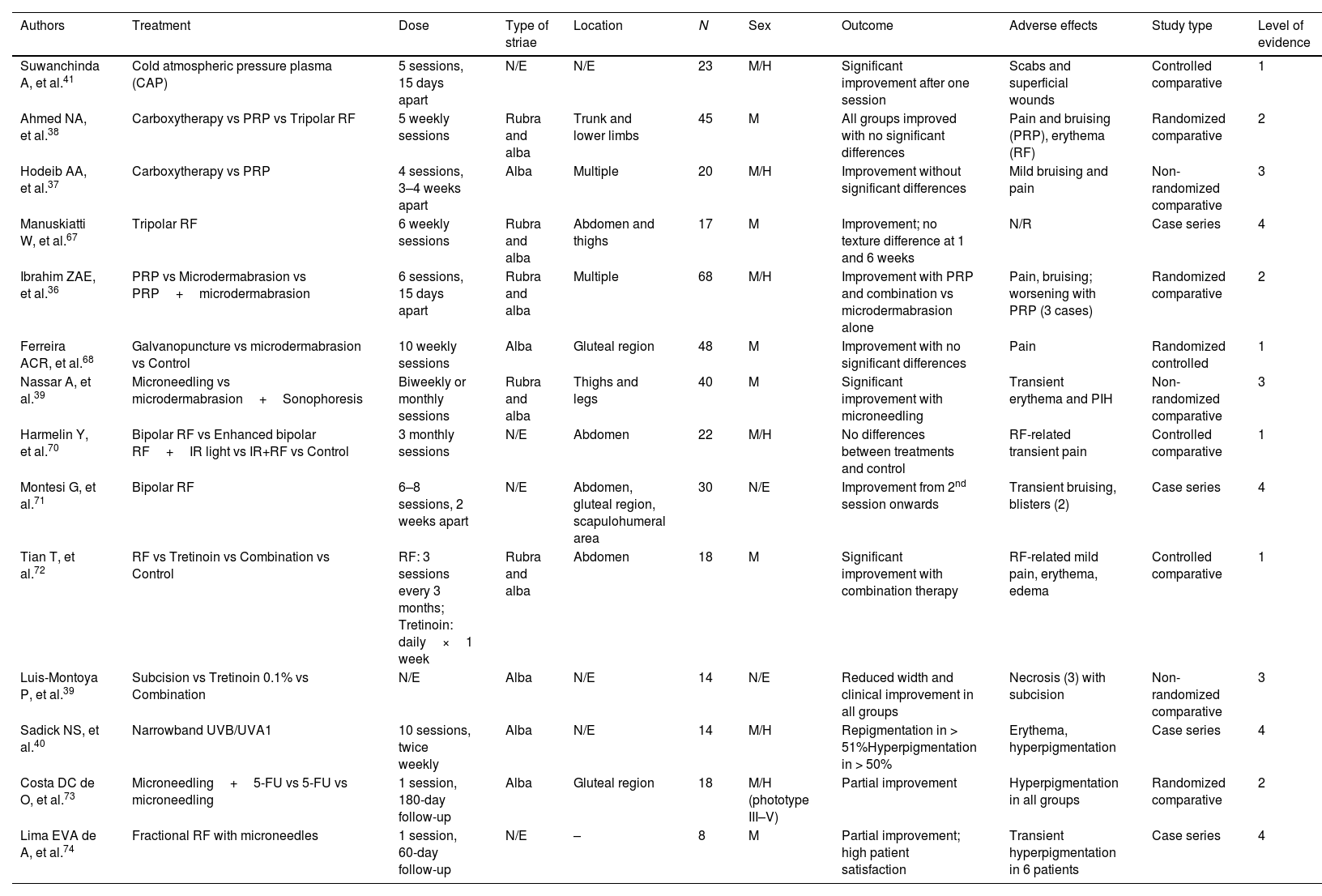
Table 7.Summary of studies on the treatment of striae with other therapies.
Authors Treatment Dose Type of striae Location N Sex Outcome Adverse effects Study type Level of evidence Suwanchinda A, et al.41 Cold atmospheric pressure plasma (CAP) 5 sessions, 15 days apart N/E N/E 23 M/H Significant improvement after one session Scabs and superficial wounds Controlled comparative 1 Ahmed NA, et al.38 Carboxytherapy vs PRP vs Tripolar RF 5 weekly sessions Rubra and alba Trunk and lower limbs 45 M All groups improved with no significant differences Pain and bruising (PRP), erythema (RF) Randomized comparative 2 Hodeib AA, et al.37 Carboxytherapy vs PRP 4 sessions, 3–4 weeks apart Alba Multiple 20 M/H Improvement without significant differences Mild bruising and pain Non-randomized comparative 3 Manuskiatti W, et al.67 Tripolar RF 6 weekly sessions Rubra and alba Abdomen and thighs 17 M Improvement; no texture difference at 1 and 6 weeks N/R Case series 4 Ibrahim ZAE, et al.36 PRP vs Microdermabrasion vs PRP+microdermabrasion 6 sessions, 15 days apart Rubra and alba Multiple 68 M/H Improvement with PRP and combination vs microdermabrasion alone Pain, bruising; worsening with PRP (3 cases) Randomized comparative 2 Ferreira ACR, et al.68 Galvanopuncture vs microdermabrasion vs Control 10 weekly sessions Alba Gluteal region 48 M Improvement with no significant differences Pain Randomized controlled 1 Nassar A, et al.39 Microneedling vs microdermabrasion+Sonophoresis Biweekly or monthly sessions Rubra and alba Thighs and legs 40 M Significant improvement with microneedling Transient erythema and PIH Non-randomized comparative 3 Harmelin Y, et al.70 Bipolar RF vs Enhanced bipolar RF+IR light vs IR+RF vs Control 3 monthly sessions N/E Abdomen 22 M/H No differences between treatments and control RF-related transient pain Controlled comparative 1 Montesi G, et al.71 Bipolar RF 6–8 sessions, 2 weeks apart N/E Abdomen, gluteal region, scapulohumeral area 30 N/E Improvement from 2nd session onwards Transient bruising, blisters (2) Case series 4 Tian T, et al.72 RF vs Tretinoin vs Combination vs Control RF: 3 sessions every 3 months; Tretinoin: daily×1 week Rubra and alba Abdomen 18 M Significant improvement with combination therapy RF-related mild pain, erythema, edema Controlled comparative 1 Luis-Montoya P, et al.39 Subcision vs Tretinoin 0.1% vs Combination N/E Alba N/E 14 N/E Reduced width and clinical improvement in all groups Necrosis (3) with subcision Non-randomized comparative 3 Sadick NS, et al.40 Narrowband UVB/UVA1 10 sessions, twice weekly Alba N/E 14 M/H Repigmentation in > 51%Hyperpigmentation in > 50% Erythema, hyperpigmentation Case series 4 Costa DC de O, et al.73 Microneedling+5-FU vs 5-FU vs microneedling 1 session, 180-day follow-up Alba Gluteal region 18 M/H (phototype III–V) Partial improvement Hyperpigmentation in all groups Randomized comparative 2 Lima EVA de A, et al.74 Fractional RF with microneedles 1 session, 60-day follow-up N/E – 8 M Partial improvement; high patient satisfaction Transient hyperpigmentation in 6 patients Case series 4 PRP, platelet-rich plasma; RF, radiofrequency; N, number of participants; F, female; M, male; N/R, not reported; N/S, not specified. Note: References outside the range [1–41] are included as Supplementary data.
Ibrahim et al.36 used local PRP injections, microdermabrasion with aluminum oxide crystals (a resurfacing technique that theoretically improves the dermal matrix and promotes re-epithelialization), and the combination of both. They observed better results with both techniques than with 1 technique only.
Hodeib et al.37 and Ahmed et al.38 compared PRP with carboxytherapy, and PRP with carboxytherapy plus tripolar RF, respectively. In both studies, all groups improved, without significant differences across treatments. In Ahmed et al., PRP was more effective in striae rubra.
- 2)
Subcision, a minimally invasive technique in which a cannula or blunt needle is introduced beneath the skin to break fibrous tracts that create surface depressions, was used alone or vs 0.1% tretinoin, or in combination with it, in the study by Luis-Montoya et al.39 No significant differences in efficacy were found across the 3 groups. However, subcision produced more adverse effects, including cutaneous necrosis in 3 patients.
- 3)
One study employed combined UVB (296–315nm) and UVA1 (360–370nm)40 for up to 10 sessions to repigment striae alba. More than half of patients achieved repigmentation, with hyperpigmentation as the most frequent adverse effect.
- 4)
Finally, cold atmospheric plasma therapy involves applying an ionized gas directly to the skin. This plasma produces a combination of reactive oxygen and nitrogen species, along with electrons, ions, and free radicals, promoting collagen and elastin synthesis, improving blood circulation, and accelerating wound healing. Only 1 study with 23 participants applied it to striae,41 showing improvement in all evaluated scales from the first session, with mild adverse effects.
In developing this work, it became evident that the scientific literature on the treatment of stretch marks is limited, as are the sample sizes and the strength of the conclusions that can be drawn from the highly variable results reported. The multitude of available options, with diverse mechanisms of action (collagen stimulation, increased skin elasticity, enhanced cellular proliferation, anti-inflammatory effects, emollient capacity, etc.), makes it difficult to recommend a single treatment.
Among topical therapies, tretinoin 0.1% and glycolic acid—both as 70% peeling and 20% daily application—stand out, as both have demonstrated improvement in the clinical appearance of striae. In studies comparing striae rubra and alba, more favorable responses were consistently seen in striae rubra, likely due to their more recent onset. Early interventions may minimize the structural epidermal and dermal changes that lead to persistent lesions. Nevertheless, in some studies, it is unclear how much of the benefit is due to massage during application rather than the topical agent per se.
Ablative and non-ablative lasers and MRF have demonstrated usefulness in treating all types of striae. Lasers or light sources targeting hemoglobin make more sense for striae rubra; however, studies evaluating both types of striae also demonstrated improvement in striae alba. Histologically, these devices increase dermal collagen and elastic fibers, helping regenerate the cutaneous surface.
Regarding PRP and similar techniques that stimulate cellular regeneration and collagen synthesis through growth factor release, their role continues to expand, particularly in combination therapies.
This review included several studies on combination treatments, including CO2+MRF15,47; CO2+PRP57; RF+PDL66; infrared light+RF70; RF+tretinoin72; subcision+tretinoin39; microneedling RF+5-FU73; and microdermabrasion+PRP.36 In most cases, combinations yielded better results than monotherapies.
Other reported combinations—such as fractional lasers with vascular lasers (e.g., CO2+PDL42 or IPL+erbium43)—have also shown good outcomes, though they were not included here due to study selection criteria.
Based on level of evidence, the 3 treatments that may be considered most clinically relevant are fractional CO2 laser, 0.1% tretinoin (especially for recent striae), and microneedling RF.
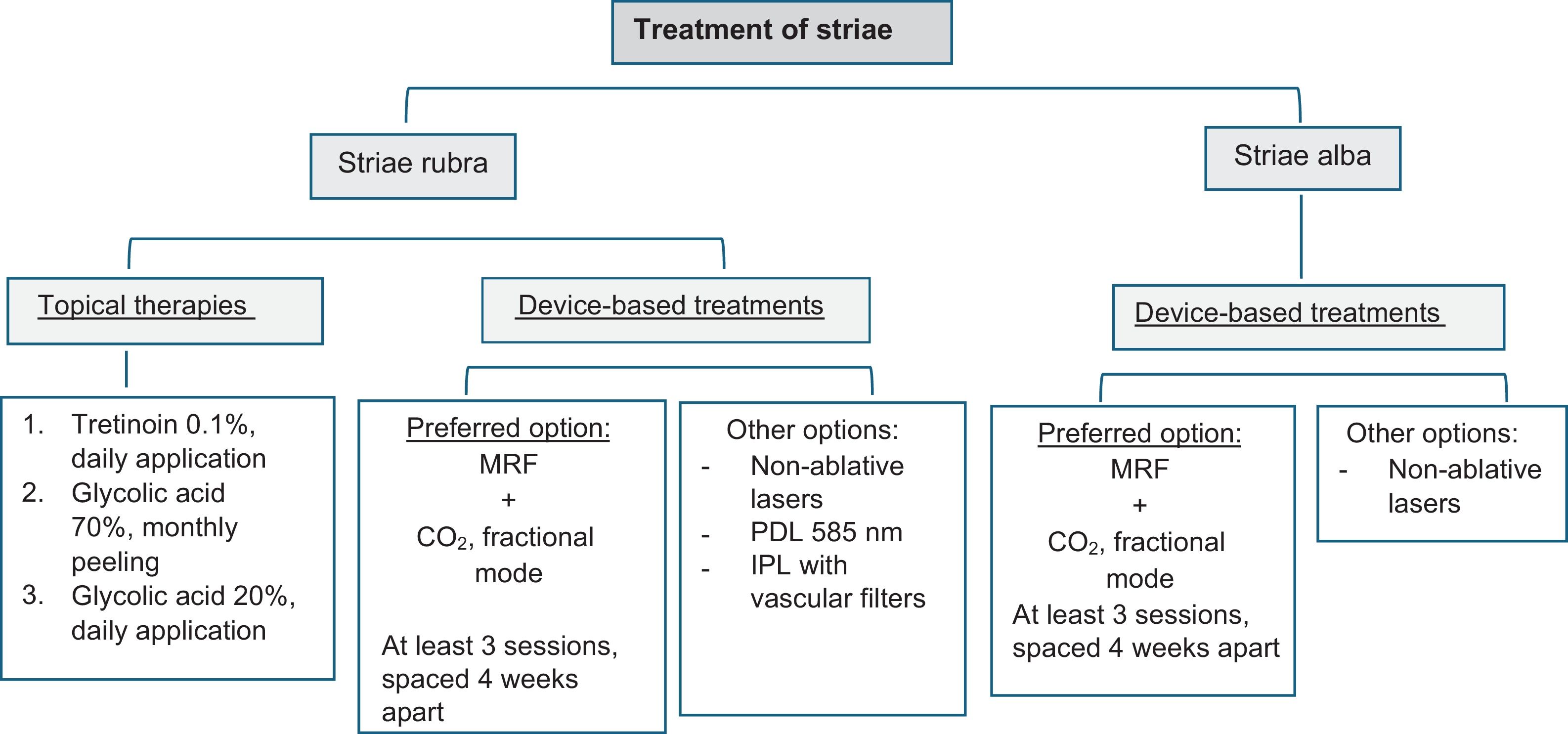
Overall, when treating a patient with stretch mark—and considering the findings of this review—the most reasonable approach is combination therapy (Fig. 1). This must be done considering that, in striae rubra, treatments aimed at reducing pigmentation and erythema should be prioritized, in contrast with the recommendation of therapies with repigmenting potential that may be beneficial in striae alba. In addition, the potential adverse effects associated with certain treatments should be taken into consideration (notably the risk of post-inflammatory hyperpigmentation, which is more common in individuals with higher phototypes).
This study has the strength of its methodology and its broadened inclusion criteria, designed to synthesize clinically relevant information as comprehensively as possible. As relative limitations, we would include the fact that only the LILACS and PubMed databases were searched, as well as the suboptimal quality of most eligible studies, which generally included a small number of patients (with a mean of 39.84 subjects).
Conclusions- 1.
Multiple treatments exist for the management and prevention of stretch marks, with variable results. Tretinoin 0.1% has demonstrated benefit in most studies. Cocoa-butter and olive-oil creams have not proven effective in preventing striae. Fractional ablative and non-ablative lasers and MRF have shown benefit via dermal collagen remodeling. Vascular lasers have greater evidence in striae rubra.
- 2.
Many analyzed studies are low quality, with small sample sizes, and comparative trials are scarce; therefore, a single first-line therapy cannot be recommended.
- 3.
Current literature does not offer clear or unified treatment guidance; however, combination therapy appears reasonable to maximize effectiveness and minimize adverse effects.
The authors declare that they have no conflict of interest.