A 61-year-old man with no previous cancer history attended the dermatology clinic with a three-year history of asymptomatic swelling on the posterior aspect of the left elbow. Physical examination revealed a subcutaneous nodule of 1cm in diameter, with no epidermal changes. A Doppler ultrasound was requested, which revealed a predominantly dermal hypodermal cystic lesion with hypoechogenic content, an echogenic rim and small echogenic foci compatible with an epidermal cyst, no solid inner nodule was depicted (Fig. 1). An excisional biopsy was performed, which revealed a trichilemmal-type follicular cyst with a 0.5mm thickness well-differentiated squamous cell carcinoma (SCC) in its wall (Fig. 2). It was presented to the oncology committee that suggested local extent of 1cm The new biopsy did not show signs of residual neoplasia. At six months of follow-up, the patient did not present clinical or dermoscopic signs of recurrence.
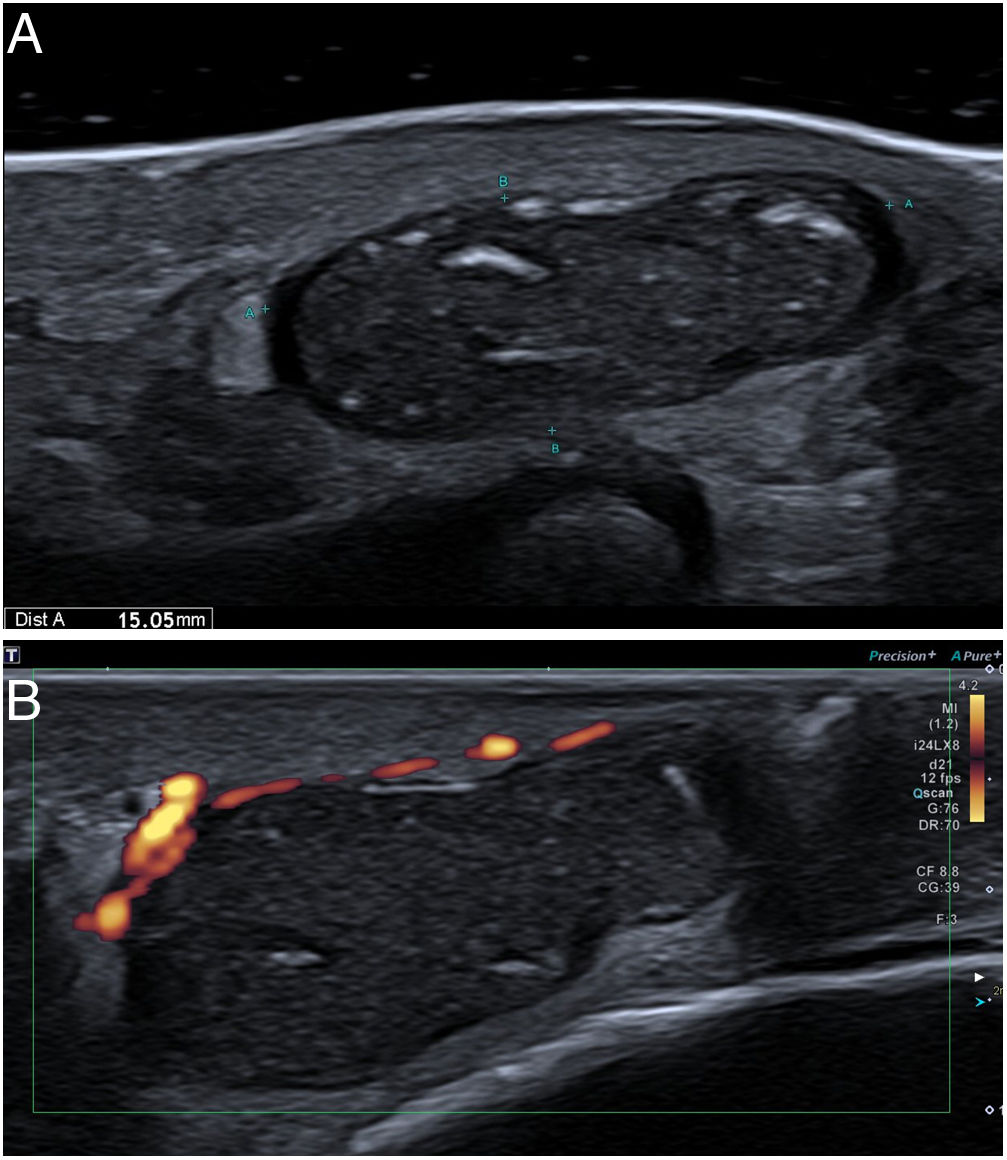
High resolution ultrasound of the posterior aspect of the elbow. Well-defined, predominantly cystic, 15-mm lesion. It is anechoic in the periphery with heterogeneous content and internal focal echoic areas suggestive of keratin (A). Lesion appears avascular, without evident internal vessels (B).
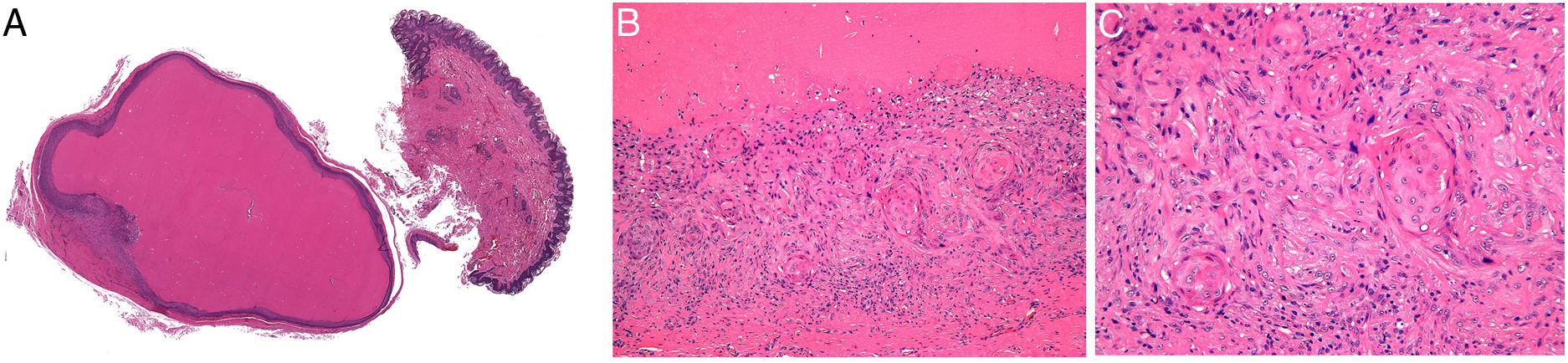
Histopathology (H&E). Scanning power shows a well-circumscribed hypodermal cyst lined by several layers of keratinocytes containing compact orthokeratotic keratin. A small intramural nodule is observed in the lower left area (A). At higher magnification, the nodule is composed of atypical keratinocytes with abundant eosinophilic cytoplasm, dyskeratosis, and pleomorphic hyperchromatic nuclei (B and C).
Trichilemmal cysts are benign adnexal tumors that develop from the outer root sheath of the hair follicle. Unlike infundibular cysts, they have a stratified epithelial lining without a granular layer and contain compact eosinophilic keratin.1–3 There are reports of squamous cell carcinoma and basal cell carcinoma arising in infundibular cysts.4 No reports of squamous cell carcinoma originating from a trichilemmal cyst were found on the reviewed literature.
Cysts complicated by wall rupture exhibit an inflammatory stromal response with foreign-body giant cells and often a proliferation of the lining epithelium with the formation of secondary cystic cavities, in these cases no atypia is observed. The differential diagnosis includes a proliferating trichilemmal tumor. This lesion is a solid neoplasm that mimics squamous cell carcinoma. It consists of multiple epithelial lobules delimited by a thick basement membrane that presents trichilemmal-type central keratinization.3,5 Although atypia is not generally a feature, foci with mitotic figures, hyperchromasia, and mild nuclear pleomorphism may be present.3,6 Some authors maintain that it represents a low-grade squamous cell carcinoma.7
The collision of a squamous cell carcinoma and a trichilemmal cyst has been reported.1 A collision tumor corresponds to two independent adjacent neoplasms in the same organ. In our case the atypical squamous proliferation was part of the cyst wall, what favors a squamous cell carcinoma originating from a trichilemmal cyst.
Risk factors for malignant transformation include large size, rapid growth, ulceration, fistulization with removal of cystic content, no response to medical treatment and recurrence.4 The presented case does not fulfill the aforementioned risk factors, probably due to the early excision performed.
This case is presented to emphasize the importance of performing a histopathological study of all excised cystic lesions, regardless of whether the symptoms and images indicate a lesion of benign etiology. In this case the small thickness of the tumor was probably missing at ultrasound by the inner content of the cyst.
Conflict of InterestThe authors declare that they have no conflict of interest.