Epidermal growth factor receptor (EGFR) inhibitors have revolutionized the treatment of cancer. Skin involvement is one of their most prevalent adverse effects. These agents often have a considerable impact on the patient's quality of life and constitute a common reason for consulting a dermatologist.
EGFR plays an important role in epidermal and pilosebaceous homeostasis and restricts interleukin 1–dependent inflammation at the level of the hair follicle.1 Its inhibition frequently causes a folliculocentric papulopustular reaction, mainly affecting sebaceous areas (face, neck, retroauricular area, shoulders, intermammary space, and scalp), with no palmoplantar involvement. The term “acneiform”, which is widely used to describe these reactions, is erroneous because of the absence of comedones, nodules, and cysts, as well as the pruriginous character of the reactions.2 Papulopustular reaction occurs early, typically during the first 2weeks after starting the drug. The reaction is dose-dependent and is more severe with monoclonal antibodies than with tyrosine-kinase inhibitors. Severity is associated with antitumor effectiveness and with survival rates.3
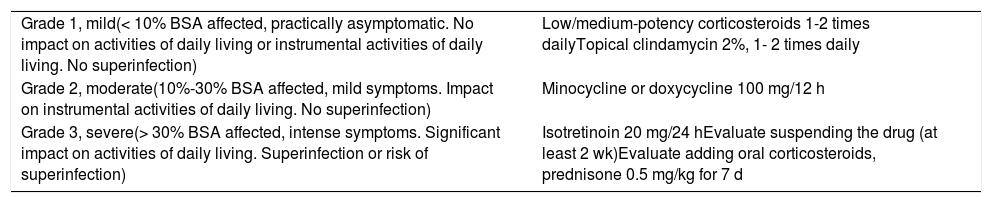
Reactions are classified into different grades depending on their intensity, impact on patient quality of life, extension, and whether or not they affect activities of daily living. Despite the absence of clinical trials in this area, various case series and experience based on clinical practice have made it possible to draw up a series of guidelines for treatment.4,5Table 1 shows recommendations for management of papulopustular rash, according to the latest clinical practice guidelines and criteria used to define the intensity of the reaction.
Recommendations for the Management of Papulopustular Rash Caused by Epidermal Growth Factor Receptor Inhibitors.
| Grade 1, mild(< 10% BSA affected, practically asymptomatic. No impact on activities of daily living or instrumental activities of daily living. No superinfection) | Low/medium-potency corticosteroids 1-2 times dailyTopical clindamycin 2%, 1- 2 times daily |
| Grade 2, moderate(10%-30% BSA affected, mild symptoms. Impact on instrumental activities of daily living. No superinfection) | Minocycline or doxycycline 100 mg/12 h |
| Grade 3, severe(> 30% BSA affected, intense symptoms. Significant impact on activities of daily living. Superinfection or risk of superinfection) | Isotretinoin 20 mg/24 hEvaluate suspending the drug (at least 2 wk)Evaluate adding oral corticosteroids, prednisone 0.5 mg/kg for 7 d |
Abbreviation: BSA, body surface area.
However, we do have more solid evidence on preventive treatment. The Skin Toxicity Evaluation Protocol with Panitumumab (STEPP) study revealed a statistically significant decrease in the incidence of grade ≥2 reactions in more than 50% of patients and in the time to onset of reactions, with no added adverse effects in the arm that received preventive treatment with a combination of low-potency topical corticosteroids, skin moisturizers, sunscreen, and doxycycline 100mg/12h with respect to reactive treatment (any treatment considered by the investigator, from 1 to 6weeks).6 A subsequent study that compared the preventive efficacy of minocycline with placebo revealed statistically significant findings after 8 weeks of treatment. Various studies have been performed to evaluate the preventive efficacy of tetracycline, tazarotene, pimecrolimus, and sunscreen in monotherapy, although none revealed statistically significant results.
Given the increasing use of these agents and their predominantly cutaneous toxicity and considerable impact on quality of life, which may even lead to suspension of a treatment that is essential for the patient, dermatologists should know how to recognize and manage these reactions.
Please cite this article as: Andrés-Lencina JJ, Aragón-Miguel R, Calleja-Algarra A. FR - Inhibidores del factor de crecimiento epidérmico y toxicidad cutánea: en busca de un protocolo de manejo. Actas Dermosifiliogr. 2019;110:499–500.