Atopic dermatitis affects a patient’s quality of life in many ways. Analysis of the effects of this disease on the lives of adult patients is therefore important for the purpose of better defining their care needs.
Patients and methodsWe interviewed 14 adult patients with atopic dermatitis in this qualitative study. The interviews were semistructured according to a simple outline to allow for completeness and flexibility and afford greater depth and richness of information.
ResultsAtopic dermatitis affected the patients’ lives in 6 spheres of activity: economic, occupational, personal, psychosocial, clinical, and relational. A clear finding was that the disease has a considerable psychosocial effect on adult patients, altering their interpersonal relationships and leading to rejection, stigmatization, and social isolation. It limits the patient in various spheres of life and in activities of daily living, causing sleep alterations among other effects. The patients were very concerned about appearance, the itch–scratch cycle, poor understanding and lack of awareness of their disease, the absence of a definitive treatment, and the adverse effects of some treatments.
ConclusionsThe quality of life of adults with atopic dermatitis is negatively affected. This disease requires a professional, holistic, multidisciplinary management approach that attempts to mitigate the adverse effects.
La dermatitis atópica afecta a la calidad de vida del paciente de muchas maneras. Por tanto, es importante analizar los efectos que la enfermedad produce en la vida del paciente al objeto de definir mejor las necesidades de atención de los pacientes adultos con dermatitis atópica.
Pacientes y métodosSe realizaron entrevistas a 14 pacientes adultos con dermatitis atópica. Las entrevistas cualitativas fueron semi-estructuradas apoyadas en un guion simple, lo que permitió una entrevista completa y flexible para un mayor nivel de profundidad y riqueza de datos.
ResultadosSe identificaron 6 esferas afectadas de la vida del paciente con dermatitis atópica: económica, laboral, personal, psicosocial, clínica y relacional. Se destaca que la dermatitis atópica tiene un gran impacto psicosocial en el paciente adulto, ya que altera las relaciones interpersonales, genera rechazo, estigmatización y aislamiento social, limita al paciente en diversas áreas y actividades de su vida cotidiana o altera el sueño, entre otros. Preocupan mucho el aspecto visible, el ciclo picor-rascamiento, la falta de concienciación y desconocimiento de la enfermedad, la ausencia de una solución definitiva entre los tratamientos y los efectos secundarios de algunos de ellos.
ConclusionesLa calidad de vida de los pacientes con dermatitis atópica se ve afectada negativamente y se hace necesaria una intervención profesional desde un abordaje multidisciplinar holístico que intente mitigar el impacto negativo de la enfermedad.
Atopic dermatitis (AD) is a chronic, recurrent disease. It is characterized by eczema and pruritus and patients often have a personal and/or family history of other diseases such as rhinitis and asthma.1,2 AD is not rare. It has an estimated prevalence of 5% to 15% in children of schoolgoing age and of 2% to 10% in adults.3 Persistence into adult age has been reported in approximately 50% of patients diagnosed with AD in childhood.4 AD, and particularly moderate or severe AD, has a considerable psychological impact and negatively affects patient quality of life.5–7
We designed a qualitative study to explore the experiences of patients with AD, as first-hand accounts can contribute to our understanding of how AD affects everyday lives.
The aim was to determine how AD affects different spheres of adult life to increase awareness among healthcare providers and encourage them to ask their patients about the impact of AD on their lives in order to tailor treatment to individual needs and circumstances and improve patient satisfaction.
The specific aims of this study were to 1) to determine how AD affects adult patients’ lives in different spheres of activity (occupational, family, relational, and social) and 2) to increase the visibility of adult AD.
Material and MethodsWe studied 14 men and women aged 18 years or older with AD. The patients were selected by simple randomization from among all patients with AD registered with the Dermatology Department at Hospital de Alcañiz in Aragón, Spain. They had all been diagnosed with AD using the classic criteria published by Hanifin and Rajka in 1980.8
The purpose of the study was described to the patients by a dermatologist and they all provided signed informed consent before the study started.
The interviews were conducted by the same interviewer (JCR) on March 21 and 22, 2016. They were video- and audio-recorded and subsequently transcribed verbatim with minimal editing.9 The project was approved by the research ethics committee of Aragon (code PI16/0029, February 24, 2016).
The interview format was semistructured and guided by a simple script (Appendix B supplementary material I). Semistructured interviews provide both the interviewer and interviewee with greater freedom and ensure that the most relevant topics are addressed.10 The interviews lasted for an average of 60 minutes (range, 30-90 minutes).
The data were analyzed using the Framework Method, which is a common technique for the thematic analysis of data in qualitative research.11 The data were coded using the qualitative data and research software program ATLAS.ti version 8 (Scientific Software Development GmbH).12 Coding was manual13 and the results were analyzed and interpreted.
ResultsSociodemographic and Clinical VariablesFourteen patients (8 men [57%] and 6 women [43%]) with a mean age of 51 years (range, 20-82 years) were interviewed. They had a mean disease duration of 29.9 years (range, 1-57 years) and a mean SCORAD score of 21.8 points (range, 0-64.3 points); 86% had received systemic treatment.
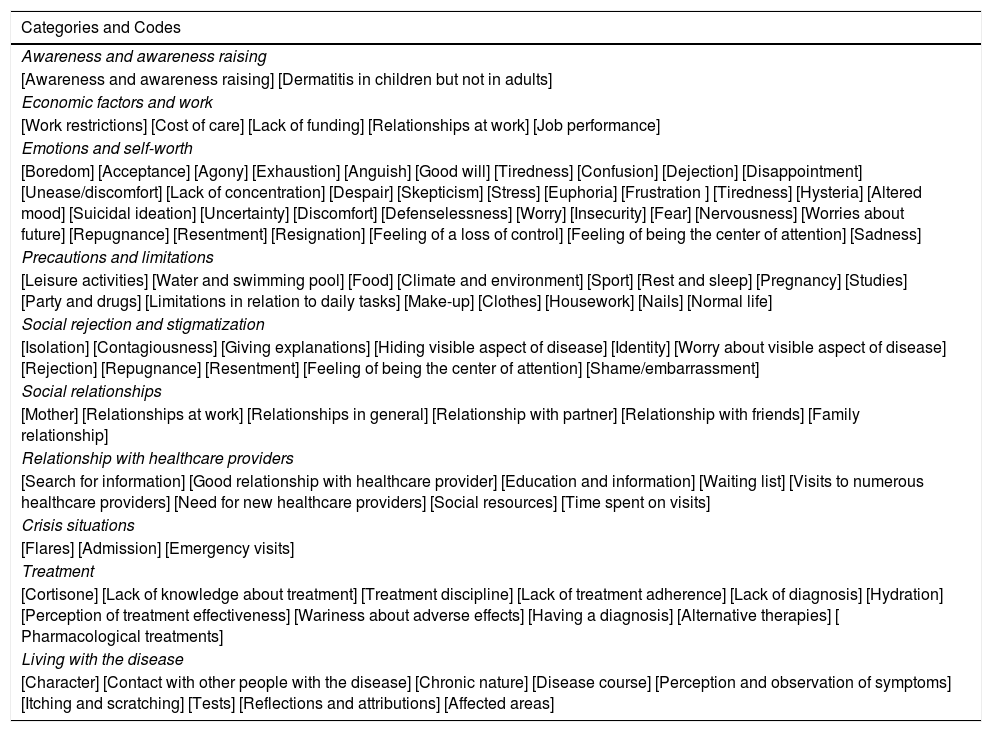
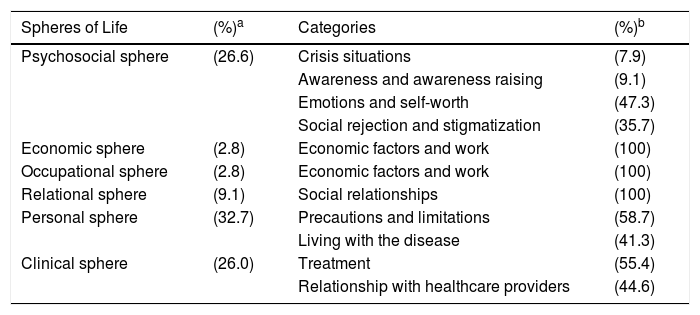
Semistructured interviewsThe findings of the semistructured interviews are summarized below according to the 6 spheres of activity analyzed (Tables 1 and 2).
Psychosocial Impact of Atopic Dermatitis on Patients Interviewed.
| Categories and Codes |
|---|
| Awareness and awareness raising |
| [Awareness and awareness raising] [Dermatitis in children but not in adults] |
| Economic factors and work |
| [Work restrictions] [Cost of care] [Lack of funding] [Relationships at work] [Job performance] |
| Emotions and self-worth |
| [Boredom] [Acceptance] [Agony] [Exhaustion] [Anguish] [Good will] [Tiredness] [Confusion] [Dejection] [Disappointment] [Unease/discomfort] [Lack of concentration] [Despair] [Skepticism] [Stress] [Euphoria] [Frustration ] [Tiredness] [Hysteria] [Altered mood] [Suicidal ideation] [Uncertainty] [Discomfort] [Defenselessness] [Worry] [Insecurity] [Fear] [Nervousness] [Worries about future] [Repugnance] [Resentment] [Resignation] [Feeling of a loss of control] [Feeling of being the center of attention] [Sadness] |
| Precautions and limitations |
| [Leisure activities] [Water and swimming pool] [Food] [Climate and environment] [Sport] [Rest and sleep] [Pregnancy] [Studies] [Party and drugs] [Limitations in relation to daily tasks] [Make-up] [Clothes] [Housework] [Nails] [Normal life] |
| Social rejection and stigmatization |
| [Isolation] [Contagiousness] [Giving explanations] [Hiding visible aspect of disease] [Identity] [Worry about visible aspect of disease] [Rejection] [Repugnance] [Resentment] [Feeling of being the center of attention] [Shame/embarrassment] |
| Social relationships |
| [Mother] [Relationships at work] [Relationships in general] [Relationship with partner] [Relationship with friends] [Family relationship] |
| Relationship with healthcare providers |
| [Search for information] [Good relationship with healthcare provider] [Education and information] [Waiting list] [Visits to numerous healthcare providers] [Need for new healthcare providers] [Social resources] [Time spent on visits] |
| Crisis situations |
| [Flares] [Admission] [Emergency visits] |
| Treatment |
| [Cortisone] [Lack of knowledge about treatment] [Treatment discipline] [Lack of treatment adherence] [Lack of diagnosis] [Hydration] [Perception of treatment effectiveness] [Wariness about adverse effects] [Having a diagnosis] [Alternative therapies] [ Pharmacological treatments] |
| Living with the disease |
| [Character] [Contact with other people with the disease] [Chronic nature] [Disease course] [Perception and observation of symptoms] [Itching and scratching] [Tests] [Reflections and attributions] [Affected areas] |
Design and Identification of the 6 Spheres of Activity and Associated Categories in the Lives of Patients With Atopic Dermatitis.
| Spheres of Life | (%)a | Categories | (%)b |
|---|---|---|---|
| Psychosocial sphere | (26.6) | Crisis situations | (7.9) |
| Awareness and awareness raising | (9.1) | ||
| Emotions and self-worth | (47.3) | ||
| Social rejection and stigmatization | (35.7) | ||
| Economic sphere | (2.8) | Economic factors and work | (100) |
| Occupational sphere | (2.8) | Economic factors and work | (100) |
| Relational sphere | (9.1) | Social relationships | (100) |
| Personal sphere | (32.7) | Precautions and limitations | (58.7) |
| Living with the disease | (41.3) | ||
| Clinical sphere | (26.0) | Treatment | (55.4) |
| Relationship with healthcare providers | (44.6) |
Some of the psychosocial impacts of AD that emerged in the interviews were related to itching, the visibility of the disease, a lack of information about AD, the search for an effective treatment, and feelings of frustration and helplessness when expected solutions did not work.
Economic Sphere (3%)The main source of discontent in the economic sphere was a lack of funding for emollients and moisturizers and the cost of these treatments.
Occupational Sphere (3%)Some of the patients reported difficulties and limitations at work that in some cases resulted in impaired performance.
Relational Sphere (9%)Several patients mentioned that AD had a negative impact on their social relationships. The patients, however, also highlighted the support they received from their family in dealing with the disease.
Personal Sphere (33%)AD had the greatest impact on personal spheres of activity, which was divided into 2 categories: worries and limitations (59%) and living with the disease (41%). The specific issues mentioned most often were itching, pain, physical activity limitations, and worsening of itching and irritation caused by sweat and contact with water.
Clinical Sphere (45%)The 2 categories in the clinical sphere were treatment (55%) and relationship with healthcare providers (45%). Emollients were reported as the most widely used treatments. The patients expressed feelings of despair and helplessness in relation to the lack of an effective treatment. Some of the patients mentioned that they were tired of going from one doctor to another and receiving different diagnoses and treatments.
DiscussionThe findings of this study show that personal and psychosocial factors associated with AD have a considerable impact on the lives of adult patients. The patients highlighted the limitations they experienced as a result of their disease, the precautions they needed to take, and the negative experience of having to live with the disease. Other salient issues were emotional burden, social rejection, stigmatization, and negative self-worth.
Our results are consistent with other findings reported for Spain (eg, the DATOP study14) and by other qualitative studies showing the considerable psychological, social, and emotional impacts of AD.9,15
Patient-reported burden is high in AD, particularly in cases of moderate or severe disease.6
Itching is the most common symptom mentioned. Our findings support previous reports of significant associations between itching intensity and quality of life.15
Similarly to the study by Fivenson et al.,7 the main negative economic impact mentioned in our study was the cost of treatment. Other factors mentioned by the patients were the cost of special diets, clothes, and cleaning products, again supporting previous findings.16
Our findings on the social impacts of AD are also similar to those reported previously.6,11
Impaired sleep has a considerable impact on overall quality of life, and sleep disturbance was a source of major concern among our patients.
A lack of restful sleep due to AD increases daytime fatigue and can cause mood disorders that affect social relationships and performance at work or school.5,13,16 Poor sleep quality would help explain some of the results observed in our study.
Visibility of AD lesions can also have a major impact on patient quality of life. In addition to the many other negative aspects reported for AD, skin disfigurement can lead to stigmatization and social rejection, limitations, and avoidance.16 AD can also have negative occupational impacts. A significant increase in indirect costs associated with presenteeism, absenteeism, sick leave, and productivity loss has been reported for patients with AD versus controls.17,18 Increased direct costs related to greater healthcare service utilization have also been reported.15
Particularly worrying issues mentioned by the patients in our series were related to treatment (14%), skin hydration (13%), and the need to visit various healthcare providers; these findings are in agreement with previous reports.5,19,20 Similarly to other authors,21 we explored the beliefs, experiences, and preferences of patients with the aim of improving treatment adherence and ultimately quality of care.
ConclusionsOur study shows that adult patients with AD experience numerous psychosocial difficulties related to the disease in general, its severity and visibility, and itching intensity. Although our sample was small, we found that AD has a negative impact on numerous spheres of activity in adult patients. The disease limited patient activities, required them to take certain precautions, and had a negative impact on self-worth, with some patients even reporting feelings of rejection and stigmatization. A lack of effective treatments and the need to visit several healthcare providers in order to receive a diagnosis also emerged as sources of discontent.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Marron SE, Cebrian-Rodriguez J, Alcalde-Herrero VM, Garcia-Latasa de Aranibar FJ, Tomas-Aragones L. Impacto psicosocial en adultos con dermatitis atópica: estudio cualitativo. Actas Dermosifiliogr. 2020;111:513–517.