We present the case of a 55-year-old man who came to our clinic with asymptomatic lesions on the legs that had appeared gradually over the previous year. The patient had no personal history of interest and was not taking medication. Physical examination revealed nonfollicular erythematous papules measuring 1 to 2mm that were distributed symmetrically on the anterior and internal aspects of the legs (Fig. 1). Some were covered with fine whitish scale (Fig. 2). The lesions were isolated and did not coalesce to form plaques.
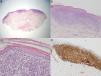
The lesions on the anterior surface of the legs were biopsied, and the results revealed lymphocyte aggregates in the superficial dermis (Fig. 3A) interspersed with infiltrate-free areas. The infiltrate was composed of atypical small-to-medium lymphocytes, with an irregular nucleus. There was marked epidermotropism (Fig. 3B and C), and isolated areas of the basement membrane had been destroyed. Immunohistochemistry (Fig. 3D) revealed a particularly intense infiltrate composed of CD3+ and CD4+ cells, with less intense staining of CD8+ cells and CD30– cells. The hair follicles and eccrine glands were not involved, and no dermal mucin deposits were found. Polymerase chain reaction assay of gene rearrangement in the T-cell receptor from the skin biopsy revealed monoclonal T-cell proliferation. These findings confirmed a diagnosis of papular mycosis fungoides.
A, Focal lymphocytic infiltrates in the superficial dermis interspersed with infiltrate-free hypodermis and dermis (hematoxylin-eosin [H-E], original magnification ×2). B, Detail of well-defined lymphocytic infiltrate in the dermis (H-E, original magnification ×10). C, Small and medium atypical lymphocytes and visible epidermotropism (H-E, original magnification ×40). D, CD3+ cells are visible throughout the infiltrate (CD3, original magnification, ×10).
Laboratory tests disclosed mild hypercholesterolemia; the remaining values, including lactate dehydrogenase and ß2-microglobulin were within the reference range. There were no palpable lymph nodes in the groin or axillas. Chest radiograph and abdominal ultrasound findings were normal.
The patient was treated with high-potency local topical corticosteroids (clobetasol cream 0.05%) once daily for 3 weeks. Since his condition improved only slightly, treatment with psoralen-UV-A (PUVA) (18 sessions) was started (oral methoxsalen at 20mg before PUVA). The cutaneous symptoms disappeared almost completely with this treatment. Today, 18 months later, the patient is free of lesions and other signs of mycosis fungoides.
Mycosis fungoides is considered to be the most common form of cutaneous T-cell lymphoma. It tends to takes the form of blotches that appear on areas of the body usually not exposed to sunlight. However, the clinical manifestations of mycosis fungoides vary considerably,1 and up to 50 variants have been described.2 One such variant is papular mycosis fungoides, an uncommon entity first described by Kodama et al.3 in 2005; only 11 cases have been published in the literature.
Mycosis fungoides usually presents as an asymptomatic persistent eruption of reddish papules generally affecting the trunk in middle-aged patients. The clinical, histopathological, and immunohistochemical findings in our case are similar to those reported for previously published cases.3–7 All those authors3–6 concur that this presentation of mycosis fungoides is not very aggressive but also agree that patients should be followed up, because in 1 case it has been reported to progress to plaque-phase mycosis fungoides .3 Prognosis is favorable in this subtype, except in patients with previous symptoms of mycosis fungoides, in whom it indicates disease progression.5
The differential diagnosis can be made with lymphomatoid papulosis, especially type B,3–5,8 which usually manifests with ulcerated and crusted lesions that tend to resolve spontaneously. It can also be made with pityriasis lichenoides et varioliformis acuta and pityriasis lichenoides chronica, both of which usually yield intraepidermal neutrophils and necrotic keratinocytes5 in the histopathology study. Diagnosis can even be made with follicular mycosis fungoides, which is characterized by infiltrate in the follicular epithelium, a certain degree of syringotropism, or both.9 Neri et al.7 proposed a differential diagnosis with aggressive epidermotropic CD8 cytotoxic T-cell lymphoma, after detecting an infiltrate composed of CD8+CD4– cells in the case of papular mycosis fungoides they report.
The main therapeutic option for papular mycosis fungoides is PUVA, which is generally successful.3,5 Other options that have been applied in the initial stages10 include coadjuvant topical retinoids,7 UV-B radiation,4 and topical corticosteroids in monotherapy.6 Given the good response with PUVA in the present case and the evidence provided by previously published cases (improvement in 8 out of 12 patients treated), we propose PUVA as the most appropriate alternative, although we do recognize that the small population could limit interpretation of our results.
Finally, we would like to highlight the wide clinical variability of mycosis fungoides, an entity that can go unnoticed and present in an unremarkable manner over several months as a papular eruption, which is often asymptomatic.
Please cite this article as: Santamarina-Albertos A, Muñoz-Martínez R, Alvarez-Gago T, Miranda-Romero A. Micosis fungoide papular en las piernas, a propósito de un caso. Actas Dermosifiliogr. 2014;105:87–89.








![A, Focal lymphocytic infiltrates in the superficial dermis interspersed with infiltrate-free hypodermis and dermis (hematoxylin-eosin [H-E], original magnification ×2). B, Detail of well-defined lymphocytic infiltrate in the dermis (H-E, original magnification ×10). C, Small and medium atypical lymphocytes and visible epidermotropism (H-E, original magnification ×40). D, CD3+ cells are visible throughout the infiltrate (CD3, original magnification, ×10).](https://static.elsevier.es/multimedia/15782190/0000010500000001/v1_201401220123/S1578219013002746/v1_201401220123/en/main.assets/thumbnail/gr3.jpeg?xkr=ue/ImdikoIMrsJoerZ+w9/t1/zx4Q/XH5Tma1a/6fSs=)



