Plaque psoriasis (Pso) and hidradenitis suppurativa (HS) are chronic inflammatory diseases associated with multiple comorbidities, including cardiovascular conditions, which may negatively impact survival. The aim of this study was to analyze mortality in patients with Pso and HS vs the general population and to each other, as well as the potential impact of biologic therapy on mortality.
Materials and methodsWe conducted a retrospective cohort study based on electronic health records retrieved from the TriNetX platform. Patients diagnosed with Pso or HS, with or without biologic therapy, were compared with matched cohorts from the general population and with each other. Cohorts were matched using propensity score matching (PSM) and adjusted for age, sex, and comorbidities potentially affecting mortality, including smoking, diabetes, hyperlipidemia, hypertension, overweight and obesity, cardiovascular disease, pulmonary embolism, venous thrombosis, ischemic heart disease, and cerebrovascular disease. The mortality incidence rate was assessed using risk ratio (RR) and hazard ratio (HR), with 95% confidence intervals (CIs) during a 10-year follow-up.
ResultsAfter adjustment, 76,191 patients with Pso and 52,354 with HS were included. Compared to the general population, patients with Pso showed a higher mortality risk (RR, 2.25; 95%CI, 2.18–2.32; HR, 2.02; 95%CI, 1.95–2.08), with a significant reduction in those treated with biologics (RR, 0.76; 95%CI, 0.70–0.83; HR, 0.62; 95%CI, 0.57–0.67). Similarly, patients with HS also exhibited a higher mortality risk (RR, 2.25; 95%CI, 2.14–2.37; HR, 2.28; 95%CI, 2.16–2.40), which was attenuated in those treated with biologics (RR, 0.80; 95%CI, 0.65–0.99; HR, 0.62; 95%CI, 0.49–0.77). When comparing both diseases, patients with HS had a higher mortality risk vs those with Pso (HR, 1.16; 95%CI, 1.11–1.22). The same trend was observed in biologic-treated subgroups (RR, 1.30; 95%CI, 1.00–1.68; HR, 1.45; 95%CI, 1.12–1.90).
ConclusionsBoth psoriasis (pso) and hidradenitis suppurativa (hs) are associated with an increased risk of mortality, which appears to be mitigated by biologic therapy. Early and comprehensive management of these conditions, including systemic inflammation control and comorbidity screening, may improve survival outcomes.
Plaque psoriasis (PsO) and hidradenitis suppurativa (HS) are chronic inflammatory diseases that extend beyond the skin and are associated with multiple systemic comorbidities. In PsO, several studies have demonstrated an increased mortality compared with the general population, with an estimated reduction in life expectancy of approximately 5 years.1,2 However, uncertainty remains as to whether this excess mortality is attributable to the disease itself, its comorbidities, or the treatments used.
Regarding the disease per se, chronic inflammation has been proposed as an independent risk factor for mortality. Some studies show increased mortality in patients with longer disease duration3 or moderate to severe forms, but not in those with mild disease after adjusting for known cardiovascular (CV) risk factors.4 Similarly, a high Systemic Immune-inflammation Index (SII) has been associated with increased mortality risk in patients with PsO.5
On the other hand, comorbidities play a prominent role. Patients with PsO have a higher prevalence of CV disease, metabolic syndrome (MetS), psychiatric disorders, pulmonary and renal diseases, cancer, and other autoimmune conditions.1 Comorbidities such as obesity, hypertension, dyslipidemia, diabetes mellitus, and CV disease significantly contribute to the elevated mortality risk in these patients.3,6 The presence of MetS in patients with PsO further increases mortality risk,7 both all-cause and CV-related.3 Nevertheless, some studies report no differences in mortality after adjusting for age, sex, and comorbidities in patients without MetS.7,8
Regarding treatment, certain studies suggest that the use of biological agents may be associated with lower mortality in PsO, with hazard ratios (HR) of approximately 0.54.2
In HS, data on mortality are scarcer and more contradictory. Some studies show a higher risk of death vs the general population and even vs patients with PsO,9,10 particularly among smokers.11 A Finnish population-based study reported a 15-year reduction in life expectancy in patients with HS vs controls, and a 10-year reduction vs PsO patients.12 However, other studies identify increased mortality only in patients with HS with specific comorbidities.13 The effect of biologics on mortality in HS remains unclear.
Given this context, we designed a real-world data (RWD) study to analyze mortality risk in patients with PsO and HS vs the general population and between both diseases, as well as to evaluate the potential effect of biological therapy on this risk.
Material and methodsWe conducted a retrospective cohort study using the TriNetX platform, a global collaborative RWD network. This tool enables clinical research through the analysis of large volumes of health data. It provides access to anonymized, standardized data from 131 healthcare organizations across 17 countries, representing information from >200 million patients.
A total of 10 adult patient cohorts (≥18 years) with follow-up from January 2013 through January 2023 were defined. Control cohorts included patients with at least 1 recorded medical visit 6 months before and 3 months after the index event (defined as the first physical examination; ICD-10: Z00). Patients with a diagnosis of PsO (ICD-10: L40.0) or HS (ICD-10: L73.2) were excluded from control cohorts comparing with PsO or HS respectively, as were patients who died before the index event (ICD-10: R99).
Exposure cohorts included patients with a confirmed diagnosis of PsO or HS, with at least 1 medical visit 3 months after the first documentation of the diagnosis (index event). These cohorts were further subdivided according to exposure to biological treatment. Biological therapy included inhibitors of TNF, IL-12/23, IL-23, or IL-17.
To minimize selection bias, cohorts were matched using 1:1 propensity score matching (PSM). Matching variables included age, sex, and comorbidities potentially associated with higher mortality: smoking, diabetes mellitus, dyslipidemia, hypertension, obesity/overweight, cardiovascular disease (CVD), pulmonary embolism, venous thrombosis, ischemic heart disease, and stroke. The Charlson Comorbidity Index (CCI) was also calculated.
The primary endpoint was all-cause mortality (ICD-10: R99), with a follow-up window of 10 years from the index event. Hazard ratios (HR) were estimated using Kaplan–Meier survival analysis and the log-rank test. Relative risks (RR) and 95% confidence intervals (95%CI) were also calculated. Statistical significance was set at p<0.01. Analyses were performed with the statistical tools integrated into TriNetX.
To examine mortality and estimate survival probabilities in patients with HS, Kaplan–Meier analyses were used. These analyses return parameters such as HR, (95%CI), No. of patients reaching the outcome (death), survival percentage, and results of the log-rank test.
ResultsThe TriNetX search identified 6,538,180 patients for the HS control cohort and 6,514,482 patients for the PsO control cohort. A total of 52,354 patients with HS were identified, of whom 2434 received biological therapy and 49,920 did not. For PsO, 76,191 patients were identified, including 10,545 treated with biologics and 65,646 untreated.
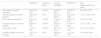
Table 1 illustrates the baseline characteristics of PsO and HS cohorts before and after PSM adjustment. Before matching, patients with HS were younger, had a higher proportion of women, and exhibited a greater burden of metabolic comorbidities vs patients with PsO. Both PsO and HS cohorts had more comorbidities than the general population. After matching, both disease cohorts were balanced in age, sex, and comorbidities. The CCI was higher in HS (0.68) and PsO (0.54) vs controls (0.30).
Baseline characteristics of patients with hidradenitis suppurativa (HS) and psoriasis (PsO) before and after propensity score matching.
| Variable | HS(before matching) | PsO(before matching) | p-Value | HS(after matching) | PsO(after matching) | p-Value |
|---|---|---|---|---|---|---|
| Number of patients | 52,354 | 76,191 | – | 35,456 | 35,456 | – |
| Mean age (years) | 41.3±14.1 | 54.3±15.0 | <0.001 | 45.6±14.0 | 45.6±14.3 | 0.859 |
| Female sex (%) | 73.0 | 46.3 | <0.001 | 63.4 | 63.0 | 0.283 |
| Smoking (%) | 24.2 | 11.9 | <0.001 | 18.4 | 18.8 | 0.189 |
| Diabetes (%) | 19.0 | 17.8 | <0.001 | 18.7 | 19.0 | 0.237 |
| Hyperlipidemia (%) | 22.3 | 31.1 | <0.001 | 25.2 | 25.4 | 0.660 |
| Hypertension (%) | 33.4 | 39.2 | <0.001 | 34.9 | 35.0 | 0.931 |
| Obesity (%) | 37.3 | 20.4 | <0.001 | 28.8 | 28.2 | 0.084 |
| AMI (%) | 1.8 | 2.0 | 0.004 | 2.0 | 1.8 | 0.015 |
| Stroke (%) | 4.1 | 6.2 | <0.001 | 4.6 | 4.5 | 0.330 |
Clinical and demographic characteristics of patients with hidradenitis suppurativa (HS) and psoriasis (PsO), before and after 1:1 propensity score matching (PSM) based on age, sex, and relevant cardiovascular comorbidities. Continuous variables are expressed as mean±standard deviation, and categorical variables as percentages.
AMI: acute myocardial infarction.
Survival analyses, shown in Table 2, revealed that patients with PsO had a significantly higher mortality risk compared with the general population (RR, 2.25; 95%CI, 2.18–2.32; HR, 2.02; 95%CI, 1.95–2.08). Biological therapy was associated with a significant reduction in mortality risk (RR, 0.76; 95%CI, 0.70–0.83; HR, 0.62; 95%CI, 0.57–0.67).
Mortality outcomes: cohort comparisons by hazard ratio (HR), risk ratio (RR), and absolute risk difference.
| HR(95%CI) | Log-rank p-value | Survival probability | RR(95%CI) | Risk difference(95%CI)/p-value | |
|---|---|---|---|---|---|
| HS (overall) vs general population | 2.28 (2.16–2.40) | <0.0001 | 84.8% vs 93.1% | 2.25 (2.14–2.37) | 4.5% (4.2–4.7%) |
| HS with biologics vs without biologics | 0.62 (0.49–0.77) | 0.018 | 88.9% vs 85.4% | 0.80 (0.65–0.99) | −1.5% (−2.9 to 0.1%) |
| PsO vs general population | 2.02 (1.95–2.08) | <0.0001 | 77.9% vs 88.9% | 2.25 (2.18–2.32) | 7.6% (7.3–7.9%) |
| PsO with biologics vs without biologics | 0.62 (0.57–0.67) | <0.0001 | 86.9% vs 81.9% | 0.76 (0.70–0.83) | −2.7% (−3.4 to −1.9%) |
| HS (overall) vs PsO | 1.16 (1.11–1.22) | <0.0001 | 82.1% vs 84.1% | 1.01 (0.97–1.06) | 0.1% (−0.3 to 0.6%) |
| HS with biologics vs PsO with biologics | 1.45 (1.12–1.90) | 0.005 | 88.6% vs 92.7% | 1.3 (1.00–1.68) | 1.4% (0.02–2.8%) |
Comparisons of 10-year mortality between adjusted cohorts based on hazard ratio (HR), risk ratio (RR), and absolute risk difference. Values include 95% confidence intervals (95%CI) and p-values from the log-rank test. Survival probabilities represent estimated survival at the end of follow-up.
HS: hidradenitis suppurativa; PsO: psoriasis.
Similarly, patients with HS exhibited increased mortality risk vs controls (RR, 2.25; 95%CI, 2.14–2.37; HR, 2.28; 95%CI, 2.16–2.40). Biological therapy also reduced mortality in HS (RR, 0.80; 95%CI, 0.65–0.99; HR, 0.62; 95%CI, 0.49–0.77), though the effect was less pronounced than in patients with PsO.
When comparing diseases, patients with HS showed higher mortality risk vs patients with PsO (HR, 1.16; 95%CI, 1.11–1.22), although the RR, did not reach significance (RR, 1.01; 95%CI, 0.97–1.06). This difference increased in the biologics-treated cohorts: patients with HS showed greater mortality risk vs patients with PsO on biologics (RR, 1.30; 95%CI, 1.00–1.68; HR, 1.45; 95%CI, 1.12–1.90).
Fig. 1 illustrates the HRs for mortality risk across the adjusted PsO, HS, biologic-treated, non-treated, and general population cohorts.
Mortality risk analysis by compared cohorts. Forest plot of hazard ratios (HR) with 95% confidence intervals (95%CI) comparing mortality across different cohorts of patients with hidradenitis suppurativa (HS), plaque psoriasis (PsO), and the general population. A reduction in mortality risk associated with biological therapy is observed for both HS and PsO, as well as a higher mortality risk in HS vs PsO, particularly in the biologic-treated cohorts. The vertical dashed line indicates the null value (HR, 1.0).
Our results confirm an increased mortality in patients with PsO and in those with HS vs the general population, which is consistent with former studies.1,2,9,11 In PsO, we observed an approximately 2-fold increase in mortality risk (RR, 2.25), even after adjusting for age, sex, and cardiovascular (CV) comorbidities. Notably, patients with HS showed an identical increased risk of mortality vs the general population (RR, 2.25), despite typically having a higher comorbidity burden. As previously noted, a multivariable adjustment was applied, including the main comorbidities associated with mortality. These findings reinforce the hypothesis that chronic inflammation may contribute to the excess mortality observed in both diseases.3,5
Given the absence of direct disease activity variables in the TriNetX platform, the use of biologics was employed as a surrogate marker for moderate-to-severe disease. Even so, patients treated with biologics showed a lower mortality risk vs those who did not receive biologics – who likely also included mild cases – with a more marked impact in PsO. This may suggest that, despite representing patients with more severe disease, biological therapy enables better control of systemic inflammation, more so in PsO than in HS, which aligns with previous reports.2,7 However, additional unmeasured confounders must be considered, including better access to health care resources, closer follow-up, or socioeconomic differences in patients eligible for biologic therapy – especially in certain health care systems. Moreover, biologic use may reflect both greater disease severity and higher-quality medical care, preventing the establishment of a direct causal relationship.
In HS, we also observed a significant reduction in mortality associated with biologic therapy, although to a lesser extent. This difference may relate to multiple factors, including lower therapeutic efficacy overall, delayed access to treatment, or a higher comorbidity burden in this population.10,13 When directly comparing the two diseases, patients with HS showed a higher mortality risk vs patients with PsO (HR, 1.16), a difference that became more pronounced (HR, 1.45) in biologic-treated cohorts. These data echo former studies reporting a greater reduction in life expectancy in HS compared with PsO.12
Of note, after adjusting for comorbidities, the mortality difference persisted, suggesting that systemic inflammation and possibly other factors not captured in large databases (e.g., socioeconomic determinants, diagnostic delays, unequal access to therapies, adherence) may play a key role. These findings also underscore the need for comprehensive management of associated comorbidities, which were more frequent in patients with PsO and HS vs the general population – conditions that, under usual circumstances, would further increase the mortality risk beyond what our adjusted data show.
Strengths of this study include the use of real-world clinical data, the large sample size, and adjustment for multiple relevant variables. However, limitations include its retrospective design and the absence of information regarding disease severity, specific causes of death, socioeconomic factors, and access to treatments, all of which constrain interpretation.
Despite these limitations, our findings provide evidence of excess mortality in patients with PsO and HS and suggest an association between biologic therapy and reduced mortality in both diseases – though causality cannot be inferred. They reinforce the importance of a comprehensive approach focused on controlling inflammation and optimizing the management of comorbidities and modifiable risk factors.
ConclusionsThis real-world clinical data study confirms that both plaque psoriasis (PsO) and hidradenitis suppurativa (HS) are associated with a significant increase in mortality compared with the general population, even after adjusting for age, sex, and cardiovascular comorbidities.
Treatment with biological agents was associated with a reduction in mortality risk in both conditions, with a more pronounced effect in PsO. This finding supports the potential role of systemic inflammation as a contributor to excess mortality and suggests that effective immunologic modulation may have a favorable impact on survival. However, this association must be interpreted with caution, as confounding factors – such as access to healthcare, treatment adherence, or socioeconomic profile – cannot be excluded. Additionally, the lack of information on clinical severity and the specific biologic used limits the generalizability of the findings.
Overall, these results highlight the need for early, integrated management strategies aimed at effectively controlling systemic inflammation and identifying and treating associated comorbidities. Such strategies may contribute to improved survival in both diseases.
Conflicts of interestRaquel Rivera-Díaz has participated in advisory boards, as a speaker, as an investigator, and has received support to attend conferences from AbbVie, Almirall, Amgen, Boehringer, BMS, INCYTE, Johnson & Johnson, Leo Pharma, Lilly, Novartis, UCB.
Beatriz Joven has participated in advisory boards, as a speaker, as an investigator, and has received support to attend conferences from AbbVie, Amgen, BMS, Johnson & Johnson, Lilly, Novartis, UCB.
The remaining authors declared no conflicts of interest whatsoever.