Pemphigus foliaceus is a superficial vesiculobullous disease that typically presents with widespread lesions. Localized presentations are less frequent, and they typically occur in middle-aged patients, following exposure to topical medications, and later on, become more disseminated. We present a case of a 19-year-old female with a localized presentation of pemphigus foliaceus unrelated to previous topical medications, that was a diagnostic and therapeutically challenging case. We also discuss the literature on localized cases, differences in presentations and responses to various treatment modalities.
El pénfigo foliáceo es una enfermedad vesículo-ampollosa superficial caracterizada por la aparición de lesiones generalizadas. Las presentaciones localizadas son menos frecuentes y suelen observarse en pacientes de mediana edad tras la exposición a medicamentos tópicos que posteriormente evolucionan a formas más diseminadas. Presentamos el caso de una mujer de 19 años de edad con pénfigo foliáceo localizado no asociado a medicamentos tópicos previos cuyo diagnóstico y tratamiento han supuesto un reto. También analizamos la literatura existente sobre los casos de pénfigo foliáceo localizado, las diferencias en las presentaciones clínicas y las respuestas a distintos tipos de tratamientos.
Pemphigus foliaceus (PF) is a superficial vesiculobullous disease characterized by production of IgG4 antibodies targeting desmoglein 1, a protein important for epidermal cell–cell adhesion.1,2 Disruption of cell–cell adhesion causes acantholysis resulting in superficial, fragile blisters that are prone to rupture. Consequently, patients typically present with erosions rather than blisters.3 Typically, the lesions are well-demarcated and occur on the face or trunk. They tend to be disseminated, and localized presentations are rare. The incidence of PF varies between different populations, and the average age of onset is between 50 and 60 years.3 The pathogenesis of PF is not completely understood, but environmental exposure appears to be involved.2,4,5 We present an interesting case of a young woman with a difficult-to-treat, localized form of PF that was unrelated to any known triggers.
Clinical caseThe patient was a 19-year-old Cuban-American woman who presented to our clinic with a 6-month history of eroded, erythematous, crusted lesions on the right side of her face. The lesions had been treated unsuccessfully with topical antifungals, antibiotics, and oral antibiotics for a presumed diagnosis of tinea or impetigo. The patient had no significant past medical history, and her only medications included oral contraceptives and occasional ibuprofen.
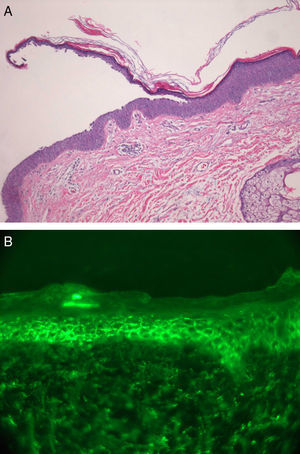
A physical examination revealed faint erythematous, eroded impetiginized patches on the right cheek and temple (Fig. 1). A culture from 1 lesion grew methicillin-sensitive staphylococcus aureus. Further laboratory studies were undertaken to screen for antinuclear antibodies, including anti-double-stranded DNA antibodies, and antibodies against the extractable nuclear antigens Smith, Ro, and La, and the histone proteins; the results were negative in all cases. A biopsy revealed superficial acantholysis and hyperchromatic nuclei in the granular layer, consistent with PF. Direct immunofluorescence studies demonstrated segmental intercellular staining with immunoglobulin (Ig) G and C3 (Fig. 2a and b). Enzyme-linked immunosorbent assay (ELISA) was negative for desmogleins 1 and 3. Based on these results, a diagnosis of PF was confirmed and the patient was started on clobetasol propionate 0.05% ointment with partial response. A trial of dapsone 100mg daily for 2 months resulted in no benefit. Prednisone 60mg daily with gradual taper induced clinical remission with no relapse during a follow-up of 18 months, except for a recent development of a single erythematous patch on the right cheek with confirmation of PF by direct immunofluorescence testing.
Localized PF is rare, and only 12 cases have been reported in the literature (Table 1)4,6–12; moreover, some of these cases later developed widespread lesions.6,7,12 Topical medications, such as imiquimod and nonsteroidal anti-inflammatory drugs, have been implicated in localized PF (Table 1).4,5 In contrast, to other cases reported, our patient was younger, she denied application of any topical medications, and the lesions did not become disseminated.
Previous reported cases of localized pemphigus foliaceus.
| Author | Age | Location of lesions | Presumed triggers | Pathology findings | DIF, IIF, and/or ELISA | Therapy and response | Dissemination |
| Newton et al.6 | 27 | Left side of nose | ND | Subcorneal bulla with considerable acantholysis | • DIF: intercellular IgG and C3• IIF: positive | Unresponsive to topical steroids | No |
| 62 | Nose | ND | Acantholysis in granular layer | • DIF: intercellular C3• IIF: positive at a titre of 1:320 | Unresponsive to topical steroids; controlled with cyclophosphamide | Yes | |
| 43 | Nose | ND | N/A | N/A | Oral prednisone 5–15mg/d prevented relapse | N/A | |
| Paramsothy et al.7 | 34 | Tip of nose, external nares and nasolabial fold | ND | Subcorneal blister which was partially intra- and partially infra-granular with acantholytic cells | • DIF: IgG between epidermal cells• IIF: positive at a titre of 1:40 | Prednisolone 30mg/day cleared rash but discontinued due to side effects | Yes |
| 65 | Nose and behind left ear | ND | Intraepidermal bulla formation below the granular layer; marked acantholysis | • DIF: IgG between epidermal cells and granular IgM in basement membrane• IIF: negative | Lesions improved after topical clobetasol propionate | N/A | |
| Yamamoto et al.8 | 81 | Right cheek | ND | Intraepidermal cleft in granular layer and acantholytic cells within the cleft | • DIF: IgG in intercellular spaces of upper cell layers• IIF: negative | Received minocycline 100mg daily, nicotinamide 9.0g daily and betamethasone valerate 2.0g daily; lesion cleared in 14 days | No |
| Termeer et al.9 | 83 | Scalp | Appeared following small local injury | Split in upper granular layer of epidermis and superficial bulla filled with acantholytic keratinocytes and fibrin | • DIF: IgG in upper epidermal layers | Treated with tacrolimus 0.1% twice daily and it significantly improved after 1 month | No |
| Lin et al.4 | 53 | Left side of face | Topical 5% imiquimod cream | Superficial acantholytic vesicular dermatitis | • DIF: IgG at keratinocyte cell surface in granular layer | IM 0.1% TAC and topical clobetasol propionate resulted in improvement, required oral prednisone to maintain clinical remission | No |
| Kishibe et al.10 | 63 | Tip of nose | ND | Subcorneal acantholysis, especially of follicular infundibulum | • DIF: IgG deposition• IIF: negativeELISA: negative for anti-desmogleins 1 and 3 antibodies | Responded to oral prednisolone 40mg daily | No |
| Zaraa et al.11 | 42 | Scalp | ND | Acantholytic cells were present | • DIF: positive• IIF: positiveELISA: positive for anti-desmoglein 1 antibodies | Topical clobetasol propionate and infiltration of triamcinolone acetonide resulted in complete healing | No |
| 34 | Right cheek | ND | Acantholytic cells were present | • DIF: positive• IIF: positive | Treated with oral prednisone and cyclophosphamide | No | |
| Ohata et al.12 | 68 | Right cheek | ND | Dyskeratotic acantholytic cells in infundibulum of hair follicle | • ELISA: positive for anti-desmoglein 1 antibody | Did not receive immediate treatment and lesions spread; later treated with prednisolone 30mg/d | Yes |
| Our case | 19 | Right cheek and temple | ND | Intercellular staining with IgG and C3 | • DIF: positive• ELISA: negative for desmogleins 1 and 3 | Partial response to clobetasol 0.05% ointment; failure of response to dapsone 100mg daily; prednisone 60mg with gradual taper induced remission | No |
Abbreviations: DIF, direct immunofluorescence; ELISA, enzyme-linked immunosorbent assay; IgG, immunoglobulin G; IIF, indirect immunofluorescence; ND, not determined; N/A, not available information.
Despite the clinical impression of impetigo, the lack of response to appropriate antibiotic treatment and the persistence of the lesions prompted us to suspect an immunobullous disorder as the source of the secondarily impetiginized lesions. The presence of subcorneal acantholysis and intercellular staining demonstrated by direct immunofluorescence confirmed the diagnosis of PF: the histopathological features of bullous impetigo may be similar to those of PF, but immunopathology would be negative in bullous impetigo.2 In PF, ELISA testing of anti-desmoglein-1 antibodies is usually positive, with sensitivities as high as 97.9%,13 and this test has been found to have greater sensitivity and specificity than conventional indirect immunofluorescence (IIF).14 A positive ELISA was reported in two of the published cases of localized PF, and IIF results in these cases were variable (see Table 1). Interestingly, our patient had a negative ELISA but IIF results were positive.
With regard to management, topical steroids may be used for more localized lesions (see Table 1) but systemic steroids are currently the mainstay of treatment and were required in our patient to induce clinical remission.15 Other treatments, such as dapsone, failed in our case.
In conclusion, immunobullous disease should be suspected in presumed infectious disorders that are refractory to appropriate antimicrobial treatment. This case exemplifies the need for proper pathological and immunopathological studies to establish a diagnosis of this very unusual variant of PF.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that this study was carried out in accordance with the protocols of their institution concerning the publication of patient data, and that all the patients included in the study were properly informed and gave their written informed consent to participation.
Right to privacy and informed consentThe authors obtained the informed consent of the patients and/or subjects referred to in this article. The signed forms are in the possession of the corresponding author.
Conflicts of interestThe authors declare that they have no conflicts of interest.