A 93-year-old man who had recently undergone surgery for a squamous cell carcinoma in the supraclavicular region was found to have, as an incidental finding, a pedunculated nodule with a broad base measuring approximately 5cm in diameter. The lesion was skin-colored with pink areas and visible telangiectasias, located on the distal third of the left lower extremity (Fig. 1). The lesion was soft and rubbery on palpation, and internal septations could be appreciated, giving it a lobulated appearance. The patient reported that the lesion had been present for many years and had progressively increased in size. It was asymptomatic, with no pain, bleeding, or other associated symptoms.
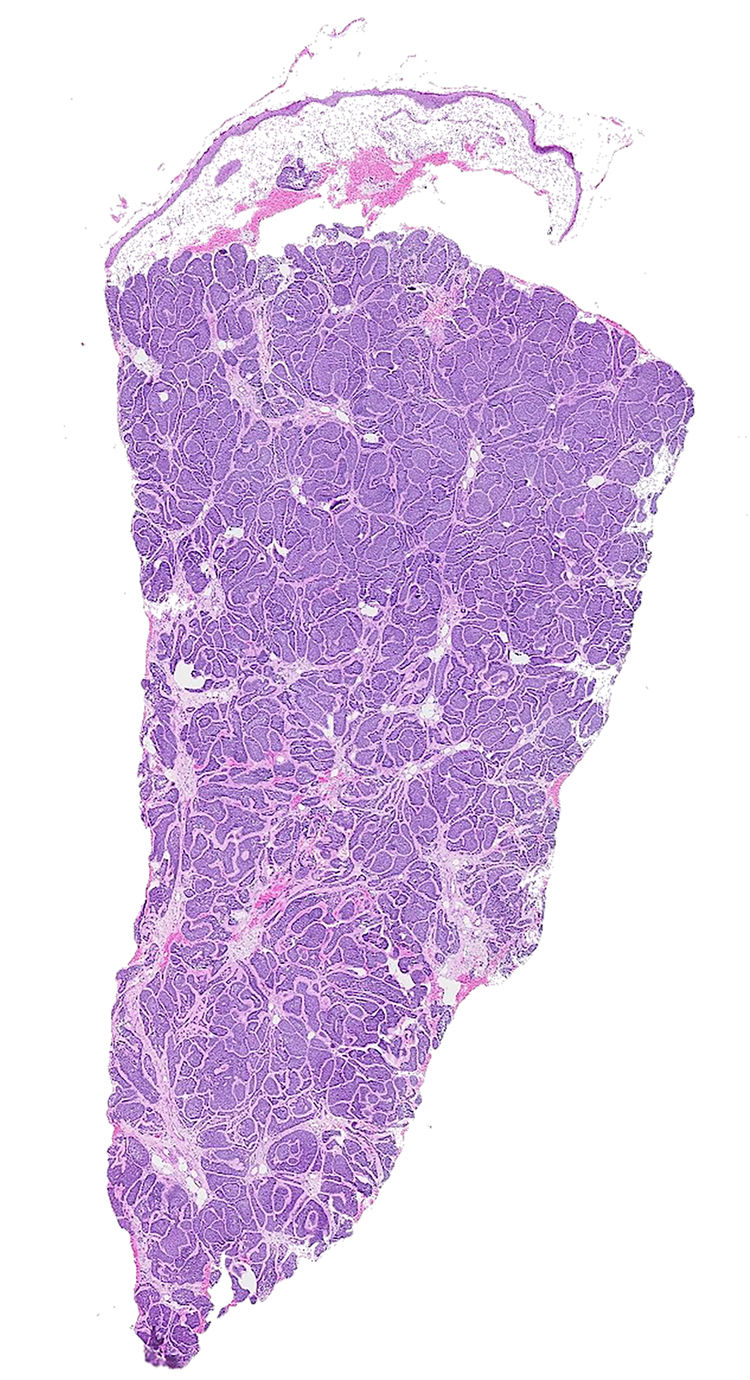
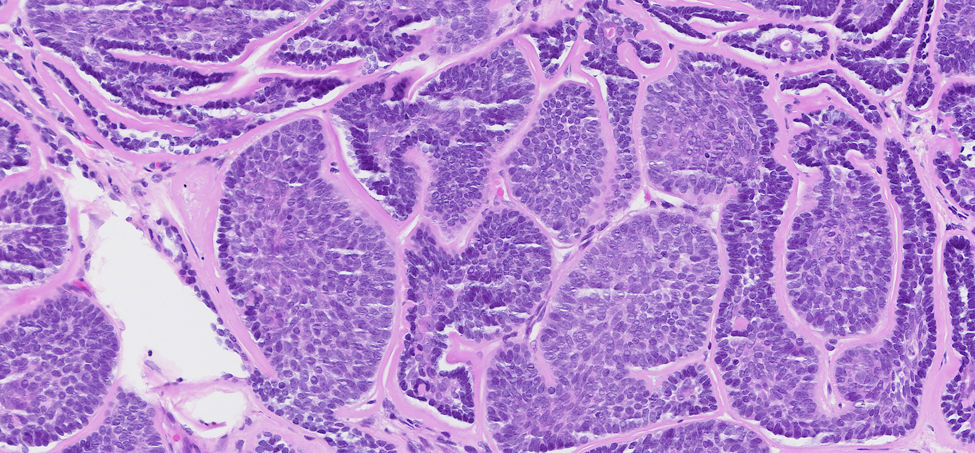
A 4-mm punch biopsy was performed. Histopathology revealed a lesion located in the mid and deep dermis composed of cellular proliferations surrounded by a thick eosinophilic basement membrane, forming polygonal-shaped nests. Cytologically, 2 cell populations were identified: peripheral basaloid cells arranged in palisading with hyperchromatic nuclei and scant cytoplasm, and central cells with abundant pale cytoplasm, vesicular nuclei, and coarse chromatin. No mitotic figures or cellular pleomorphism were observed (Figs. 2 and 3).
What is your diagnosis?
DiagnosisCylindroma.
TreatmentA decision was made jointly with the patient to pursue clinical observation without intervention.
CommentCylindromas are benign adnexal tumors, more common in women, which may occur as solitary lesions or in the context of Brooke–Spiegler syndrome or autosomal dominant familial cylindromatosis, in which cylindromas, spiradenomas, and trichoepitheliomas may all arise.1,2
Clinically, they appear as papules, nodules, or pedunculated lesions—similar to the present case—most often located on the head (90%). They may be skin-colored, red, or bluish and typically measure<1cm, although cylindromas as large as 20cm have been reported.1,3 Only 3 cases involving the lower extremities have been published, 1 presenting with multiple linear lesions on the distal leg, and 0 associated with cylindromas at other sites.2–4
Solitary cylindromas frequently harbor the MYB–NFIB fusion gene, which acts as an oncoprotein that promotes neoplastic proliferation, whereas familial cylindromatosis syndromes exhibit mutations in the CYLD tumor suppressor gene.1,5 Immunohistochemical studies show strong nuclear MYB expression in both settings, suggesting that this oncoprotein may play a key role in the pathogenesis of both sporadic and familial cylindromas.1,5
Histopathology shows nests of basaloid cells typically located in the dermis, sometimes extending into the hypodermis, surrounded by an eosinophilic basement membrane that imparts the characteristic “jigsaw puzzle” appearance.1 Within the tumor nests, 2 distinct cellular populations can be identified: smaller peripheral cells with hyperchromatic nuclei arranged in palisading, and larger central cells with paler nuclei and abundant cytoplasm resembling secretory or ductal cells, suggesting a possible apocrine or eccrine lineage.1
The histologic differential diagnosis includes trichoepithelioma, spiradenoma, basal cell carcinoma, and malignant adnexal tumors such as adenoid cystic carcinoma, which may exhibit cylindroma-like areas. Trichoepitheliomas show basaloid cell nests with internal mucin deposits and a dense fibrous stroma with spindle cells. A retraction artifact (cleft) may be observed between the tumor stroma and the surrounding normal dermal stroma, which distinguishes it from basal cell carcinoma, in which the retraction cleft appears between the tumor epithelium and its own tumor stroma. Spiradenoma may occur in association with cylindroma and presents as nests of tumor cells forming lobules surrounded by a fibrous stroma containing blood vessels.1,3
Although the treatment of cylindromas is surgical, particularly for solitary lesions, recurrences are common. Malignant transformation is rare and typically occurs in patients with Brooke–Spiegler syndrome. In fact, <50 cases of malignant transformation have been reported, of which only 9 involved solitary cylindromas.5,6 Rapid growth, color change, pain, ulceration, or bleeding may suggest malignancy.5,6 Histologically, cylindrocarcinomas appear as poorly differentiated tumors with pleomorphic nuclei and numerous mitoses; the distinction between peripheral and central cell populations is lost, as is the hyaline membrane, resulting in the disappearance of the characteristic “jigsaw puzzle” pattern.5,6 On the face, cylindrocarcinomas may be mistaken for basal cell adenocarcinomas of the salivary glands.6
Conflict of interestThe authors declare that they have no conflict of interest.