Erythropoietic protoporphyria (EPP, OMIM: 177000) is an innate error of the metabolism caused by autosomal recessive hereditary mutations in the gene FECH (Gene ID: 2235), which cause a ferrochelatase enzyme deficiency (EC 4.99.1.1) (<30% of normal). Ninety-six percent of affected individuals have composite heterozygotic mutations: from one parent, they inherit an allele with a loss of function that leads to almost no ferrochelatase activity and from the other parent, they inherit an allele with low expression, which produces ferrochelatase activity that is less than 50% of normal (c.315-48T > C; also known as IVS3-48T > C). Four percent of cases inherit 2 FECH alleles with complete loss of function. Some rarer erythropoietic porphyrias are caused by hereditary mutations linked to the X chromosome (OMIM: 300752) or by mutations in the gene CLPX (OMIM: 618015), which explain less than 10% of cases. These diseases are characterized by acute, painful, and burning nonampullary lesions that appear within less than 30 minutes of exposure to light. The lesions are caused by the accumulation of protoporphyria IX in the endothelium of the blood vessels close to the surface of the skin, which absorbs light in the Soret band and passes into an excited state that generates free radicals, which, in turn, damage the surrounding cutaneous tissue.1 To prevent these lesions, patients develop an aversion to light and a preference for enclosed spaces, which significantly affects their style and quality of life.2 Most available treatments (e.g., beta-carotene, N-acetyl-L-cysteine, and vitamin C) have shown no clear benefit supported by clinical trials.3 Afamelanotide (Scenesse, Clinuvel Pharmaceuticals) is a potent analogue of α-melanotide stimulating hormone, which has been shown to reduce the incidence and severity of phototoxic reactions and to improve quality of life in the long term.4,5 This drug, however, is not yet available in many countries.
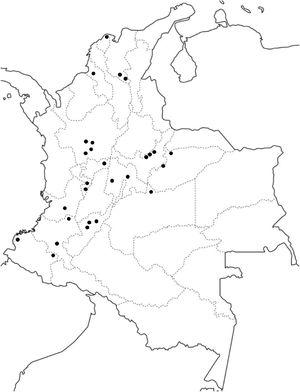
The prevalence and incidence of EPP have not been estimated in Colombia or in many other Latin-American countries (Fig. 1). This information is important for evaluating the burden of this disease on the population and the associated health care service requirements. This information is also essential for introducing new therapies into the national health service and coverage by the insurance companies. Finally, the lack of information available on EPP is one of the biggest concerns for patients and their family members.2 We therefore performed a study based on prospective information from the Colombian Comprehensive Social Protection Information System database for the period between 2014 and 2018. We identified patients suffering from EPP by means of the international classification of diseases code E80.1 and only included those with a confirmed new diagnosis. The reference population was obtained from the database of the Colombian National Statistics Administrative Department. The annual incidence was calculated as the number of new cases in a year over the total population for that year. Prevalence was estimated from the incidence, assuming a mean duration of EPP of 77 years (prevalence = incidence × mean duration of EPP).6 All of this assumes that, during the study period, the population of the country remained relatively stable and the annual incidence was constant.
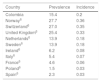
The study showed that the annual incidence (0.2 new cases per million inhabitants) and the estimated prevalence (15.4 cases per million inhabitants) of EPP in Colombia are similar to those reported for the Netherlands and Sweden but differ from those of many other countries6 (Tables 1 and 2). Considerable variability has previously been reported in the epidemiology of EPP between countries in comparison with acute hepatic porphyria. The prevalence of EPP may vary depending on the frequency of the low expression allele (c.315-48T>C) in the population, which may range from 1% in Africans to 43% in Japanese.1 The frequency of this allele in Colombians in unknown. Moreover, expression of the disease may change in relation to the degree of skin pigmentation, such that greater melanin deposits lead to less pronounced symptoms.6 EPP affects men and women relatively equally in Colombia, which agrees with observations in other populations. The symptoms of EPP usually start in childhood and advanced age at the time of diagnosis may therefore indicate a long delay in diagnosis. This is in the context of the fact that most patients in developed countries with ample experience in treating this disease report delays in diagnosis of up to 18 years.2,7 Deficiencies have been shown in the diagnosis of porphyria in Colombia and a greater delay in diagnosis is therefore to be expected.8 Furthermore, it is likely that the predominance of mixed-race people in Colombia is linked to a higher proportion of mild cases. One limitation of this study is that, although the database queried made it possible to identify cases with a confirmed diagnosis of EPP, it is not possible to verify the methods used to confirm the diagnosis. Situations such as coding errors and limits to the number of diagnostic codes available may affect the accuracy of epidemiologic estimates based on administrative sources. An overestimation of the incidence and prevalence of EPP cannot therefore be ruled out in this study.
Annual Incidence, Estimated Prevalence, and Sociodemographic Characteristics of Erythropoietic Protoporphyria in Colombia, 2014-2018.
| EPPa | |
|---|---|
| Patients | 40 |
| Sex, female; n, % | 23, 57.5 |
| Mean (SD) age | 32.4 (23.1) |
| Mean annual incidence (95% CI)b | 0.2 (0.1-0.4) |
| Prevalence (95% CI)b | 15.4 (14.3-16.5) |
Abbreviations: SD indicates standard deviation; 95% CI, 95% confidence interval.
Prevalence and Incidence of Erythropoietic Protoporphyria in Colombia Compared to Other Countries.
| Country | Prevalence | Incidence |
|---|---|---|
| Colombia | 15.4 | 0.2 |
| Norway6 | 27.7 | 0.36 |
| Switzerland6 | 27.0 | 0.35 |
| United Kingdom6 | 25.4 | 0.33 |
| Netherlands6 | 13.9 | 0.18 |
| Sweden6 | 13.9 | 0.18 |
| Ireland6 | 6.2 | 0.08 |
| Italy6 | 5.4 | 0.07 |
| France6 | 4.6 | 0.06 |
| Poland6 | 1.5 | 0.03 |
| Spain6 | 2.3 | 0.03 |
Reference population: 45,000,000 inhabitants, estimated per million inhabitants.
The authors declare that they have no conflicts of interest.
Please cite this article as: Jaramillo-Calle DA. Incidencia y prevalencia de la protoporfiria eritropoyética en Colombia, 2014-2018. Actas Dermosifiliogr. 2021;112:186–188.