Hidradenitis suppurativa (HS) is an inflammatory disease of the pilosebaceous follicle. It is a chronic disease, characterized by the appearance of inflammatory lesions (nodules, fistulas, and abscesses) in the apocrine gland-bearing regions, which affects the quality of life.
Its treatment constitutes a significant therapeutic challenge and often requires surgical intervention. To this end, several surgical techniques have been described, ranging from incision and drainage, deroofing, to localized or wide excision, which may require grafts or flaps for the reconstruction of the resulting defects when resections are large, leading to scars with aesthetic and functional repercussions.1,2 Therefore, an important objective is to find a surgical technique that allows for simpler interventions without requiring grafts and flaps, which would reduce sequelae.
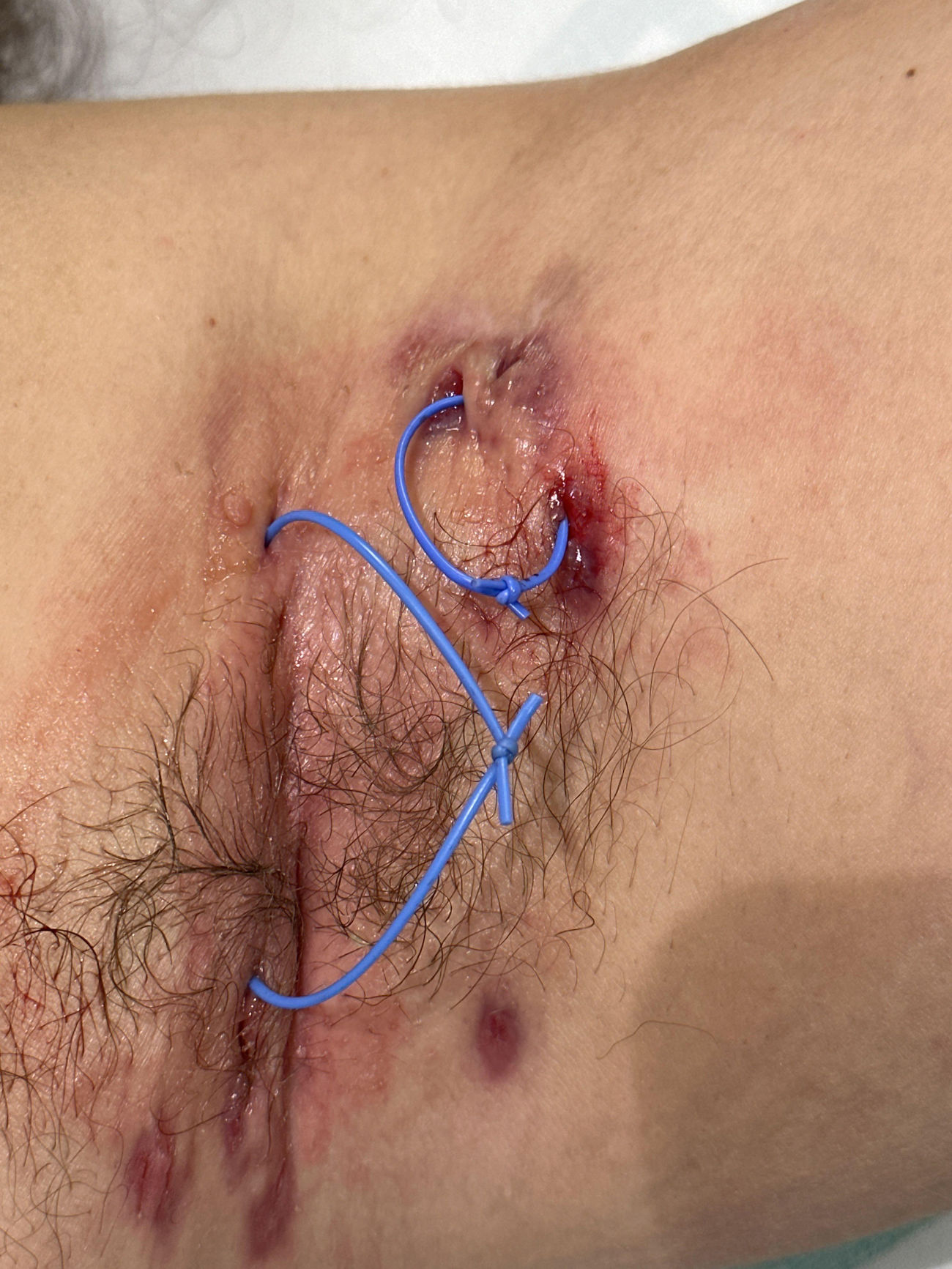
The use of setons (Fig. 1) is a conservative surgical technique used in the treatment of fistulas in perianal inflammatory disease. To date, the literature is scarce regarding its use in the treatment of fistulas of hidradenitis suppurativa.3,4 Therefore, this prospective before-and-after study was designed, whose primary endpoint was to evaluate the efficacy profile of the use of setons in controlling pain associated with fistulas in patients with hidradenitis suppurativa. Secondarily, its impact on quality of life and the number of flares per month was evaluated.
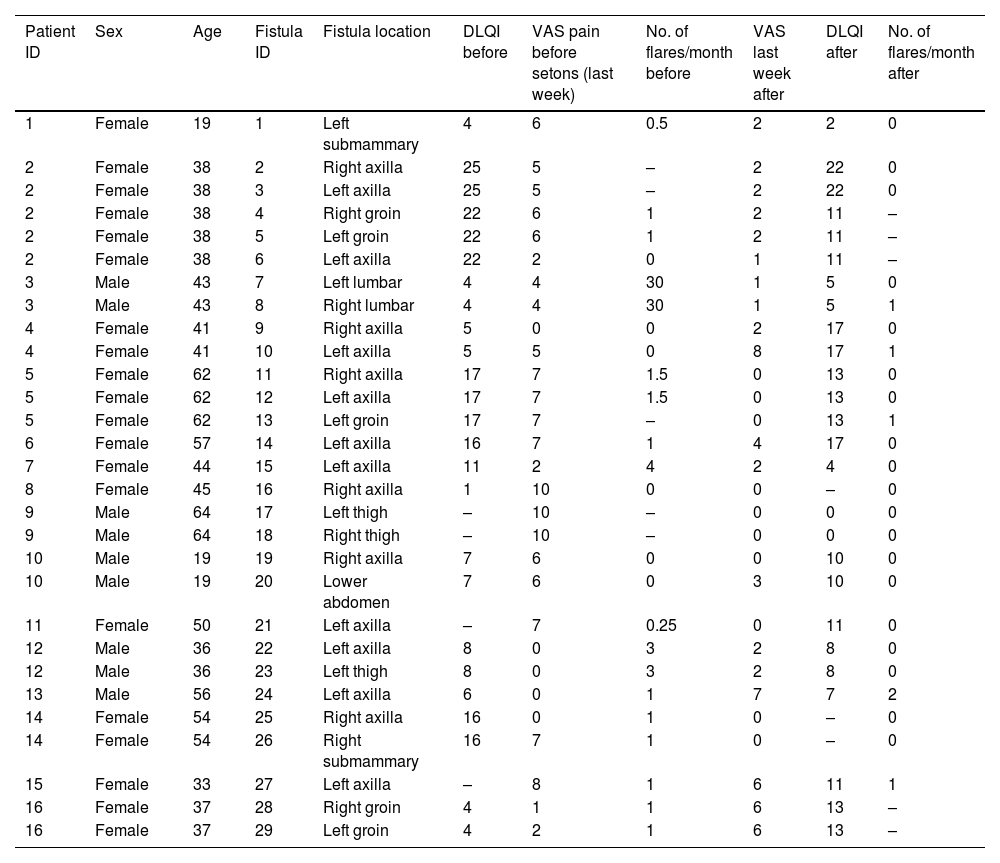
A total of 16 consecutive patients were included without randomization or blinding, 11 of whom (69%) were women, with a total of 29 fistulas. Each of the fistulas was analyzed separately (Table 1). The patients’ mean age was 43 (±13.42) years. A total of 16 fistulas (55%) were axillary.
Baseline data of the patients and baseline and post 4–6 weeks clinical data after seton placement.
| Patient ID | Sex | Age | Fistula ID | Fistula location | DLQI before | VAS pain before setons (last week) | No. of flares/month before | VAS last week after | DLQI after | No. of flares/month after |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Female | 19 | 1 | Left submammary | 4 | 6 | 0.5 | 2 | 2 | 0 |
| 2 | Female | 38 | 2 | Right axilla | 25 | 5 | – | 2 | 22 | 0 |
| 2 | Female | 38 | 3 | Left axilla | 25 | 5 | – | 2 | 22 | 0 |
| 2 | Female | 38 | 4 | Right groin | 22 | 6 | 1 | 2 | 11 | – |
| 2 | Female | 38 | 5 | Left groin | 22 | 6 | 1 | 2 | 11 | – |
| 2 | Female | 38 | 6 | Left axilla | 22 | 2 | 0 | 1 | 11 | – |
| 3 | Male | 43 | 7 | Left lumbar | 4 | 4 | 30 | 1 | 5 | 0 |
| 3 | Male | 43 | 8 | Right lumbar | 4 | 4 | 30 | 1 | 5 | 1 |
| 4 | Female | 41 | 9 | Right axilla | 5 | 0 | 0 | 2 | 17 | 0 |
| 4 | Female | 41 | 10 | Left axilla | 5 | 5 | 0 | 8 | 17 | 1 |
| 5 | Female | 62 | 11 | Right axilla | 17 | 7 | 1.5 | 0 | 13 | 0 |
| 5 | Female | 62 | 12 | Left axilla | 17 | 7 | 1.5 | 0 | 13 | 0 |
| 5 | Female | 62 | 13 | Left groin | 17 | 7 | – | 0 | 13 | 1 |
| 6 | Female | 57 | 14 | Left axilla | 16 | 7 | 1 | 4 | 17 | 0 |
| 7 | Female | 44 | 15 | Left axilla | 11 | 2 | 4 | 2 | 4 | 0 |
| 8 | Female | 45 | 16 | Right axilla | 1 | 10 | 0 | 0 | – | 0 |
| 9 | Male | 64 | 17 | Left thigh | – | 10 | – | 0 | 0 | 0 |
| 9 | Male | 64 | 18 | Right thigh | – | 10 | – | 0 | 0 | 0 |
| 10 | Male | 19 | 19 | Right axilla | 7 | 6 | 0 | 0 | 10 | 0 |
| 10 | Male | 19 | 20 | Lower abdomen | 7 | 6 | 0 | 3 | 10 | 0 |
| 11 | Female | 50 | 21 | Left axilla | – | 7 | 0.25 | 0 | 11 | 0 |
| 12 | Male | 36 | 22 | Left axilla | 8 | 0 | 3 | 2 | 8 | 0 |
| 12 | Male | 36 | 23 | Left thigh | 8 | 0 | 3 | 2 | 8 | 0 |
| 13 | Male | 56 | 24 | Left axilla | 6 | 0 | 1 | 7 | 7 | 2 |
| 14 | Female | 54 | 25 | Right axilla | 16 | 0 | 1 | 0 | – | 0 |
| 14 | Female | 54 | 26 | Right submammary | 16 | 7 | 1 | 0 | – | 0 |
| 15 | Female | 33 | 27 | Left axilla | – | 8 | 1 | 6 | 11 | 1 |
| 16 | Female | 37 | 28 | Right groin | 4 | 1 | 1 | 6 | 13 | – |
| 16 | Female | 37 | 29 | Left groin | 4 | 2 | 1 | 6 | 13 | – |
An analysis was performed using the Kolmogorov–Smirnov test to evaluate the normality of the variables collected in the study and, subsequently, since the analyzed variables (VAS score, DLQI, and number of flares per month) did not follow a normal distribution, they were analyzed using the Wilcoxon test for paired data.
The median for pain VAS decreased from a median of 6 (2–7) to 2 (0–2) (p=0.005) after 4–6 weeks since the placement of setons, which was statistically significant. The number of flares per month was significantly reduced from a median of 1 (0.19–1.5) to 0 (0–0) (p=0.007). The DLQI score ranged from a median baseline value of 8 (5–17) to 11 (7–13) (p=0.653).
The use of setons is common in the treatment of patients with inflammatory bowel disease and complex perianal fistulas. Tokunaga and Sasaki3 described their utility in 10 men with hidradenitis suppurativa and complex anal fistulas in whom setons were placed and maintained for about 6–8 months without observed recurrences. Lajevardi and Abeysinghe4 described a patient with hidradenitis suppurativa and axillary fistulas treated with setons. Vilarrasa et al.5 refer to the usefulness of this technique for the treatment of fistulas in these patients, both as definitive treatment and as a bridging treatment to reduce surgical complexity in the management of these lesions. Fernández-Vela et al.6 conducted a retrospective multicenter study that included 27 patients with axillary, inguinal, and gluteal fistulas, demonstrating a statistically significant improvement in both the VAS score and the depth of the fistula and its inflammation after 5–6 weeks of seton placement. The results of this study are consistent with the results obtained in our study, in which a significant improvement in the VAS score was also achieved. The number of flares per month was not recorded by these authors, nor were fistulas in other locations, such as submammary, abdominal, or lumbar, which are included in our study.
Our study has some limitations though. One of them is sample size, which may condition the lack of statistically significant differences in the reduction of the DLQI score before and after seton placement. Another limitation is the short follow-up time (4–6 weeks), which prevents knowing if later relapses occur.
In conclusion, this study shows a statistically significant reduction in both the visual analog scale for pain and the number of flares per month after 4–6 weeks of using setons in the treatment of fistulas in patients with hidradenitis suppurativa. These results reinforce the hypothesis that the use of setons is also useful in the treatment of fistulas presented by these patients, including it as another alternative for their treatment.