Patients with Hidradenitis Suppurativa (HS) have higher hospitalization rates than those with other skin diseases; however, in our country, healthcare resource utilization has been scarcely studied.1,2 The objective was to describe the epidemiology of HS-related hospitalizations in Spain and to determine whether sex-based differences exist.
A retrospective observational study was designed using data from the Spanish Ministry of Health's Specialized Care Registry within the Minimum Basic Data Set between January 1, 2016, and December 31, 2021.3 Discharges coded as L73.2 under ICD-10 (corresponding to HS) as the principal diagnosis were selected. Demographic and hospitalization-related data were analyzed. Hospitalization rates were calculated using population data from the National Institute of Statistics.4
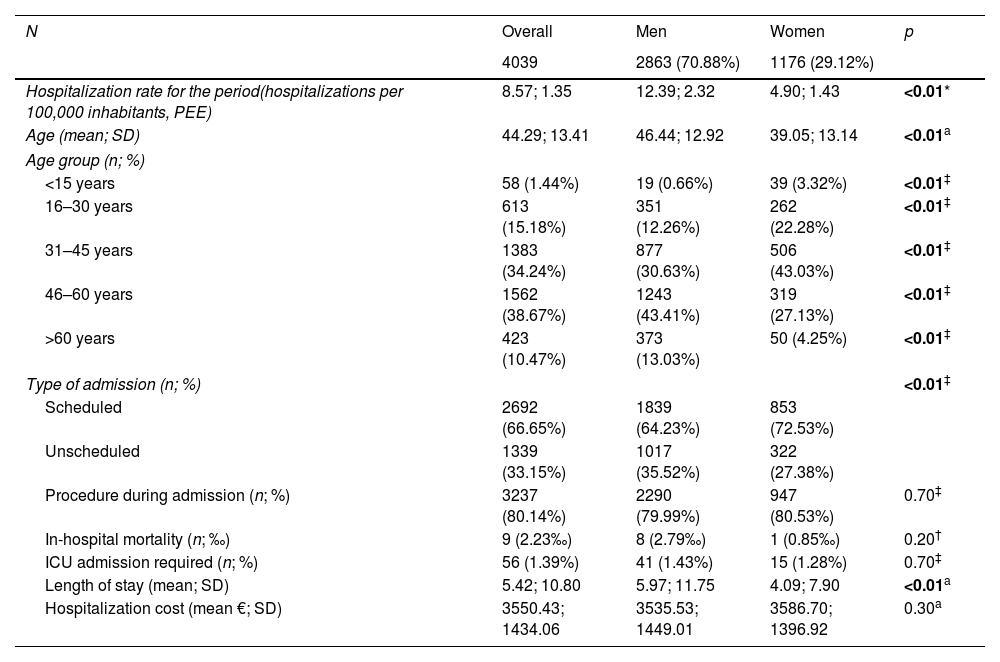
Among 4039 hospitalizations with a diagnosis of HS during 2016–2021 (Table 1), 70.88% were men. The overall hospitalization rate was 8.57 per 100,000 person-years, higher among men (12.39 vs 4.90; p<0.01). Regarding age distribution, the mean age was lower among women (39.05 years vs 46.44; p<0.01), and 88.09% of hospitalized patients were between 16 and 60 years old. Women predominated in the pediatric age group (p<0.01).
Crude and sex-stratified hospitalization rates for the study period, and demographic and health care parameters of interest for patients hospitalized for HS in Spain between 2016 and 2021.
| N | Overall | Men | Women | p |
|---|---|---|---|---|
| 4039 | 2863 (70.88%) | 1176 (29.12%) | ||
| Hospitalization rate for the period(hospitalizations per 100,000 inhabitants, PEE) | 8.57; 1.35 | 12.39; 2.32 | 4.90; 1.43 | <0.01* |
| Age (mean; SD) | 44.29; 13.41 | 46.44; 12.92 | 39.05; 13.14 | <0.01a |
| Age group (n; %) | ||||
| <15 years | 58 (1.44%) | 19 (0.66%) | 39 (3.32%) | <0.01‡ |
| 16–30 years | 613 (15.18%) | 351 (12.26%) | 262 (22.28%) | <0.01‡ |
| 31–45 years | 1383 (34.24%) | 877 (30.63%) | 506 (43.03%) | <0.01‡ |
| 46–60 years | 1562 (38.67%) | 1243 (43.41%) | 319 (27.13%) | <0.01‡ |
| >60 years | 423 (10.47%) | 373 (13.03%) | 50 (4.25%) | <0.01‡ |
| Type of admission (n; %) | <0.01‡ | |||
| Scheduled | 2692 (66.65%) | 1839 (64.23%) | 853 (72.53%) | |
| Unscheduled | 1339 (33.15%) | 1017 (35.52%) | 322 (27.38%) | |
| Procedure during admission (n; %) | 3237 (80.14%) | 2290 (79.99%) | 947 (80.53%) | 0.70‡ |
| In-hospital mortality (n; ‰) | 9 (2.23‰) | 8 (2.79‰) | 1 (0.85‰) | 0.20† |
| ICU admission required (n; %) | 56 (1.39%) | 41 (1.43%) | 15 (1.28%) | 0.70‡ |
| Length of stay (mean; SD) | 5.42; 10.80 | 5.97; 11.75 | 4.09; 7.90 | <0.01a |
| Hospitalization cost (mean €; SD) | 3550.43; 1434.06 | 3535.53; 1449.01 | 3586.70; 1396.92 | 0.30a |
PEE: population standard error; SD: standard deviation; ICU: intensive care unit; *tests used.
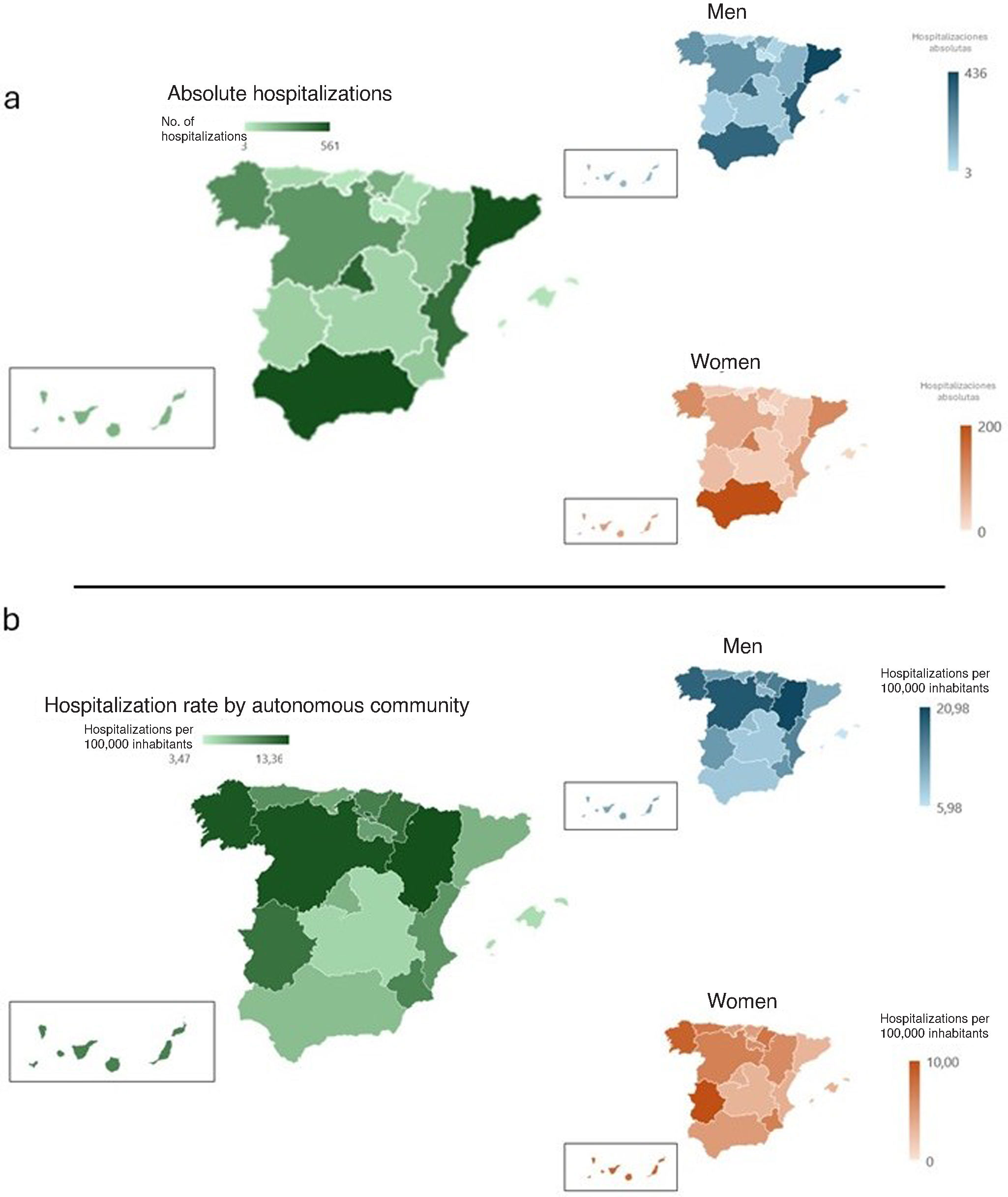
Catalonia (n=561; 13.99%), Andalusia (n=560; 13.86%), the Community of Madrid (n=484; 11.98%), and the Valencian Community (n=457; 11.31%) had the highest absolute number of hospitalizations (Fig. 1). However, northern regions showed the highest rates, led by Aragón, Castile and León, and Galicia (13.37, 13.07, and 12.94 cases per 100,000 person-years, respectively).
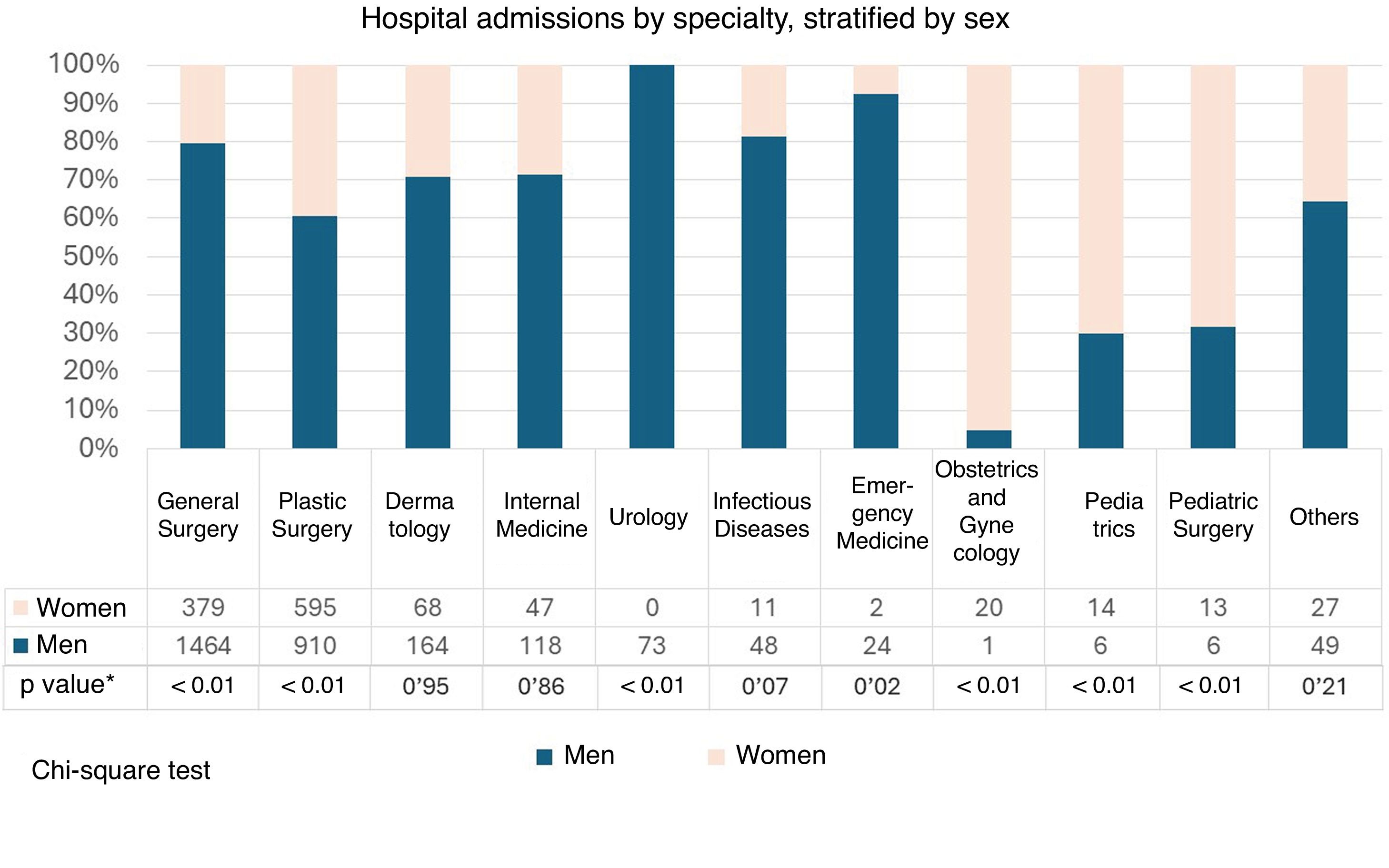
Regarding admission characteristics (Table 1), 66.65% were scheduled, and 80.14% involved surgery. The mean length of stay was 5.42 days, and the mean cost was €3550.43. Women had significantly higher rates of scheduled admissions (72.53% vs 64.23%; p<0.01) and a shorter mean length of stay (4.09 vs 5.97 days; p<0.01). General surgery (45.63%) and plastic surgery (37.26%), followed by dermatology (5.74%), were the departments admitting the most cases (Fig. 2). By sex, women had significantly more admissions in plastic surgery, gynecology and obstetrics, pediatrics, and pediatric surgery (p<0.01), whereas men had higher rates in general surgery, emergency medicine, and urology.
Of note, most patients were of working age and, on average, spent 5 days hospitalized. This, along with probable postoperative convalescence, may explain the high rates of lost workdays among individuals with HS.5 Of note, the mean length of stay was relatively high considering that HS interventions are increasingly less invasive and outpatient-based.6
Additionally, although the HS Barometer indicates that most patients identify a dermatologist as their reference specialist, <6% were admitted under dermatology during hospitalization.5 Structural variability within the specialty across Spain may account for this finding and aligns with geographic rate patterns observed in the study.7
Although HS prevalence is higher among women, hospitalization rates in men are 3 times higher. Moreover, women show higher rates of scheduled admissions, at younger ages, and in different hospital departments. Altogether, these observations reinforce a sex-based disparity, likely reflecting differences in healthcare-seeking behavior and access.8
Among neighboring countries, only Portuguese studies have conducted similar analyses, showing comparable hospitalization and intervention rates but differing in sex and age distributions. Those studies reported male predominance and slightly older mean age, and included a broader set of variables.9 In Spain, studies exist for other chronic immune-mediated dermatologic diseases with relapsing courses—such as atopic dermatitis and psoriasis—which show lower hospitalization rates but similar geographic disparities.10,11
Some limitations include potential miscoding under ICD-10 in non-dermatologic specialties, the fact that private hospitals are not required to report data, and the inability to analyze hospital-based interventions not requiring admission. However, to our knowledge, this is the first study addressing HS-related hospitalizations in Spain.
In conclusion, the profile of hospitalized HS patients in Spain appears to be a middle-aged man, admitted electively for surgical intervention for a non-negligible duration, with sex-based differences in relevant parameters and regional heterogeneities that warrant deeper investigation.
Conflict of interestThe authors declare that they have no conflict of interest.