Histoid leprosy is a rare variant of multibacillary leprosy.1 It has unique clinical, histologic, and immunologic characteristics.2 Most cases occur as a relapse of lepromatous leprosy, whereas de novo cases are rarer. The histoid lesions have a high bacillus content, which favors growth of resistant strains and, therefore, represents a public-health problem.3 We report a patient from a poor social environment with clinical and histopathologic characteristics of de novo histoid leprosy.
Case DescriptionA 35-year-old homeless man from Cali was evaluated due to lesions located on the extremities and back, which had appeared 6 months earlier. The skin lesions were accompanied by weight loss, general malaise, and fever that had not been measured. The patient was a drug abuser and reported having been in contact with his stepfather, who had been diagnosed with Hansen disease.
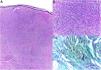
The physical examination revealed multiple skin-colored papules and nodules with an infiltrated appearance, some of which were ulcerated, and others had a central hematic crust. The lesions were located on the upper limbs and back. The lower limbs and buttocks presented papules that coalesced to form brownish-red plaques (Fig. 1). Lack of feeling on palpation was found in all the lesions.
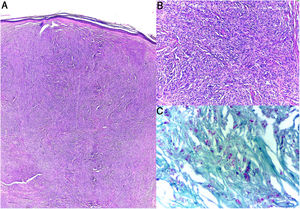
Blood tests revealed that the patient was negative for HIV and FTA-ABS, and blood count, liver function, and kidney function were normal. Skin biopsies were taken. Histopathology findings revealed nodular dermal aggregates composed of fusiform histoid cells in a storiform pattern (Fig. 2A and 2B). Fite-Faraco staining revealed abundant acid-fast and alcohol-fast bacilli (Fig. 2C). A diagnosis of histoid leprosy was made. The patient decided to leave the hospital and it was not, therefore, possible to instate treatment.
DiscussionHistoid leprosy (HL) is a rare variant of lepromatous leprosy. It was first described in 1963 by Wade.1 Most reported cases of HL are relapses in patients with multibacillary leprosy or patients receiving inadequate or irregular treatment. De novo cases exist, in which HL develops with no evidence of other types of leprosy. These cases are even more rare,4 as in the case of this patient.
The entity usually presents in men between the ages of 30 and 50 years.5–7 Mos5t patients are of low socioeconomic status and have a history of contact with leprosy.7 These sociodemographic characteristics concur with those of our patient.
HL has unique clinical, histologic, and immunologic characteristics.2 Classical clinical findings are well defined skin-colored or erythematous shiny papules and cutaneous or subcutaneous plaques and nodules arising from normal skin.8 The usual location is on the back, buttock, extremities, and face. It rarely involves the ear lobes and, unlike lepromatous leprosy, madarosis is not present. Loss of feeling in the lesions is typical.
Histopathologic findings include epidermic atrophy and a dermis with a Grenz zone and circumscribed collections of fusiform histoid cells distributed in a storiform pattern. Fite-Faraco staining supports the diagnosis by revealing acid-fast and alcohol-fast bacilli.9 The findings in our patient agree with those described in the literature.
The pathogenesis of this unusual variant is not fully understood. It is thought to be the result of multiple factors, combining genetic factors, abnormal immune response, and incomplete treatments. A hyperreactive response is thought to exist with increased cellular immunity due to the presence of necrosis and ulceration in some lesions, which is thought to be an effort to combat the Mycobacterium.10 This theory may explain the ulceration observed in several of the nodules in our patient.
The histoid lesions contain a high number of bacilli and are therefore reservoirs for resistant strains of infection.3 This is a public-health problem, as it makes eradication of the disease difficult—more so when patients have little access to health care, as in our patient, who was a homeless man and who decided not to undergo treatment. Treatment of HL is that recommended by the World Health Organization (WHO) for multibacillary leprosy, with clofazimine, dapsone, and rifampicin for 12 months.
ConclusionsHistoid leprosy is a rare variant and is thought to be underdiagnosed. It is important to recognize the atypical forms of Hansen disease in order to make the appropriate diagnosis and prescribe the correct treatment when required, as well as to prevent the physical and psychological damage that patients may suffer.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Calvache N, Arias DA, Delgado VM. Lepra histioide, un enemigo aún no erradicado. Actas Dermosifiliogr. 2021;112:280–281.