Folliculitis decalvans (FD) and lichen planopilaris (LPP) are primary cicatricial alopecias classified according to the predominant cell-type infiltrate on histopathology. FD is characterized by a neutrophilic infiltrate, while LPP is marked by a lymphocytic inflammation.1 Clinically, FD presents as a patch cicatricial alopecia with tufted hairs, pustules, follicular papules and crusts, while LPP mainly exhibits perifollicular erythema and perifollicular scales.2 Recently, an overlap of FD and LPP has been described as Folliculitis Decalvans and Lichen Planopilaris Phenotypic Spectrum (FDLPPPS), which combines clinical, trichoscopic and histopathological features of both diseases.2–9 We report the case of a 21-year-old female patient with FDLPPPS associated with pityriasis amiantacea (PA), misdiagnosed as refractory seborrheic dermatitis.
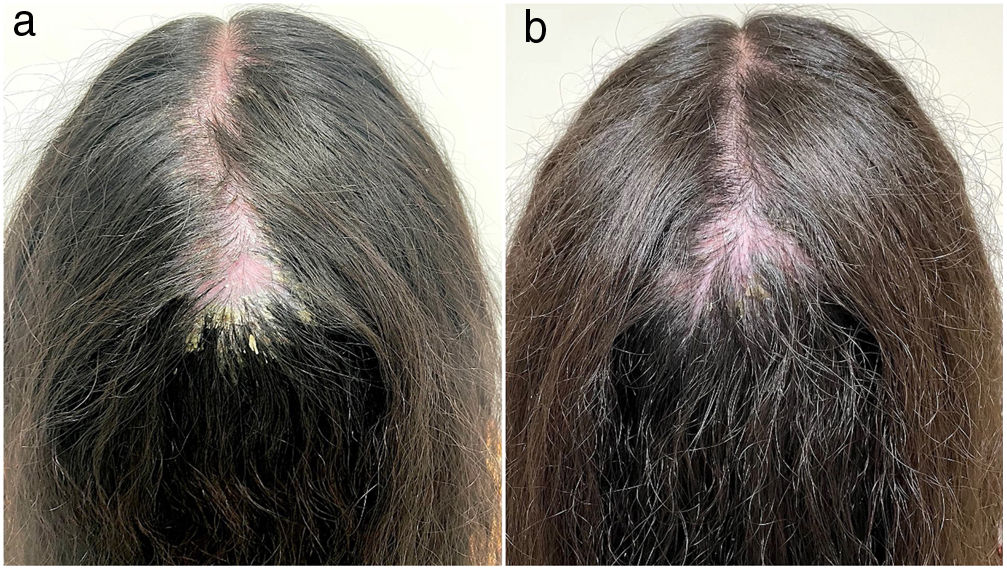
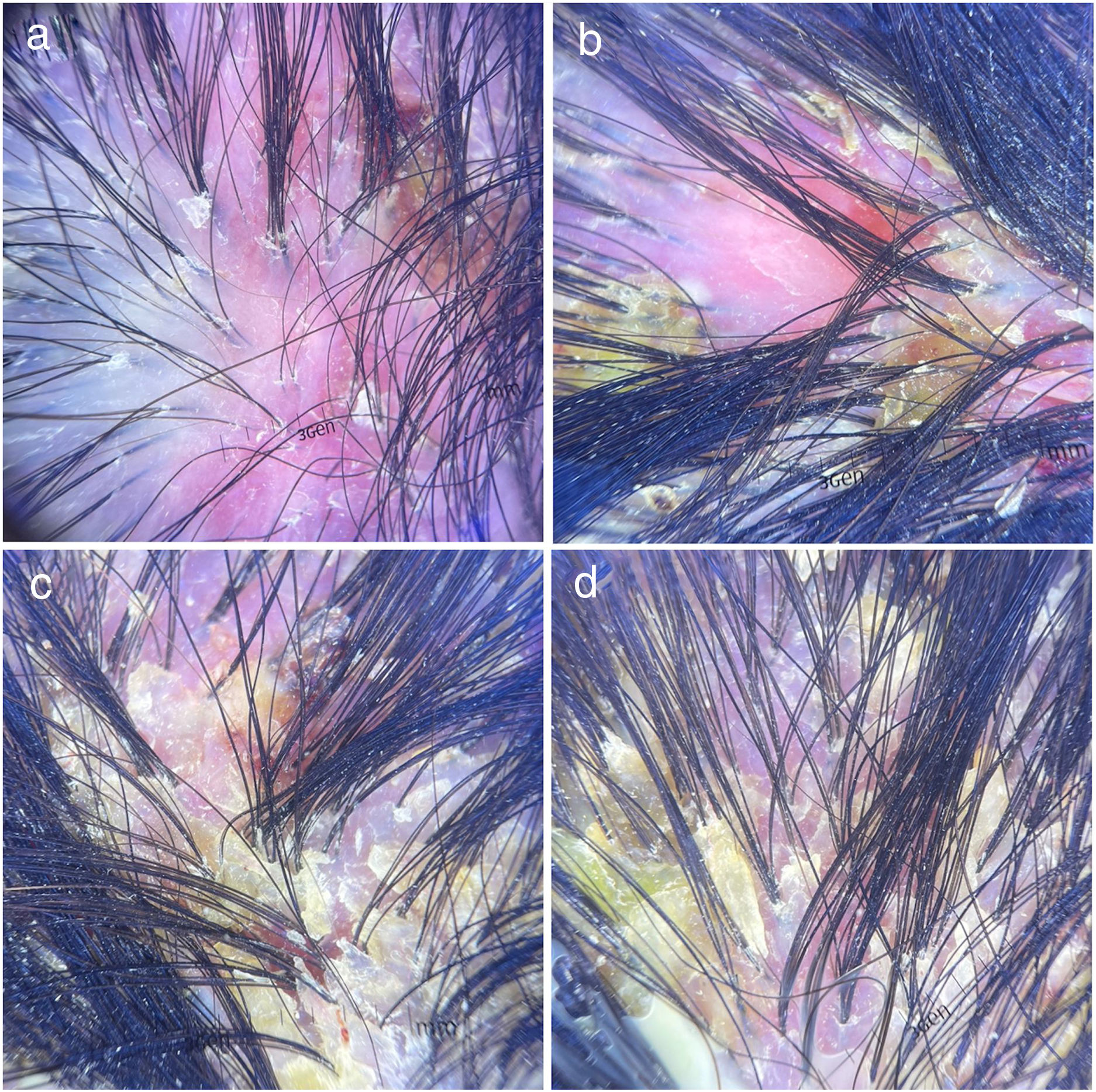
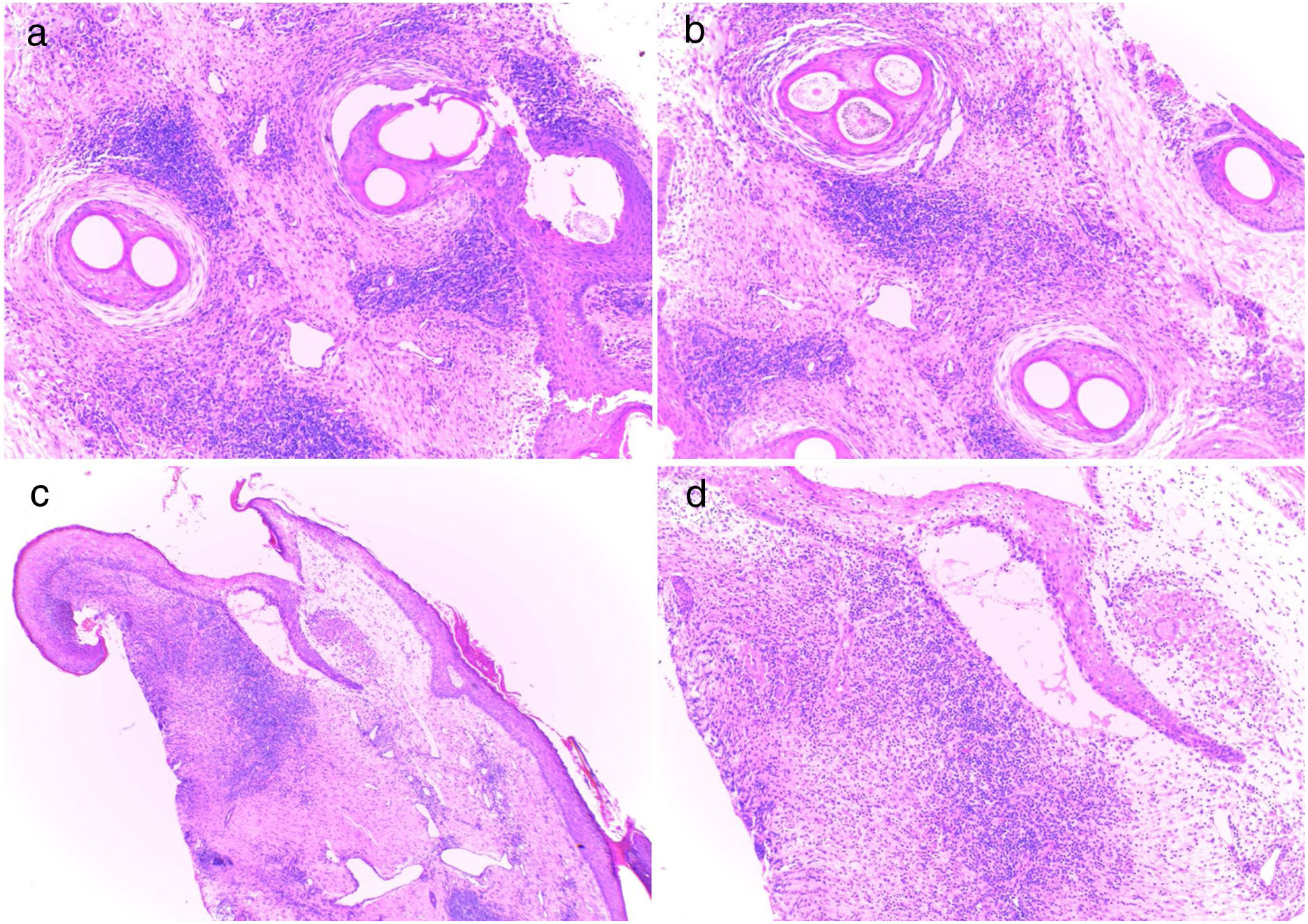
A healthy 21-year-old female presented with a 13-year history of intense desquamation, pruritus and alopecia on her scalp. She referred multiple consultations with general practitioners, being repeatedly treated for seborrheic dermatitis, without improvement. The patient had no relevant family medical history. A year ago, she experienced a worsening of symptoms with pain and hair loss. She also had erythema, pustules and adherent crusts on her scalp. Dermatological examination revealed a large patch of cicatricial alopecia on the vertex and crown, extending to left and right parietal scalp; intense erythema, adherent scales, yellow/hemorrhagic crusts, pustules and polytrichia (Fig. 1a). Trichoscopy indicated decreased hair follicles density, perifollicular and interfollicular white scales, hair tufts, hemorrhagic crusts, milky-red areas, dilated blood vessels, and interfollicular erythema (Fig. 2). Histopathological study identified hyperkeratosis, absence of sebaceous glands, interstitial lymphoplasmacytic infiltrates, scarce neutrophils, plasma cells dermal aggregates, perifollicular concentric fibrosis, and granulomas around fragmented hair shafts (Fig. 3). These findings suggested FDLPPPS associated with PA. We prescribed trimethoprim/sulfamethoxazole 160–800mg twice a day, clobetasol propionate emulsion 0.05% daily, salicylic acid shampoo 2% in alternate days and oral prednisone 20mg daily for 2 months. After this therapeutical approach, the lesions showed satisfactory improvement (Fig. 1b). Maintenance treatment was adopted with doxycycline 100mg daily and oral prednisone 40mg/day in weekend pulse. There was no progression of alopecia after 4 months of follow-up.
(a) A large patch of cicatricial alopecia on the vertex and crown, extending to left and right parietal scalp; intense erythema, adherent scales, yellow/hemorrhagic crusts, pustules and polytrichia. (b) Satisfactory improvement after therapeutical approach: reduction of erythema, pustules and scales, hair growth, and no progression of alopecia.
Trichoscopy: (a) Intense erythema, decreased hair follicles density, perifollicular and interfollicular white scales, hair tufts, hemorrhagic crusts, milky-red areas, dilated blood vessels. (b) Intense erythema, decreased hair follicles density, perifollicular white scales, hair tufts, yellow/hemorrhagic crusts, milky-red areas. (c) Hair tufts, adherent scales, yellow/hemorrhagic crusts. (d) Perifollicular white scales, hair tufts, adherent yellow crusts.
Histopathological study: (a, b) Vertical section showing absence of sebaceous glands, interstitial lymphoplasmacytic infiltrates, scarce neutrophils, plasma cells dermal aggregates, perifollicular concentric fibrosis, and granulomas around fragmented hair shafts (hematoxylin–eosin stain; ×100). (c) Horizontal section showing hyperkeratosis, perifollicular and interstitial lymphoplasmacytic infiltrates, scarce neutrophils, and a granuloma around the hair follicle (hematoxylin–eosin stain; ×40). (d) Horizontal section showing perifollicular and interstitial lymphoplasmacytic infiltrates, scarce neutrophils, and a granuloma around the hair follicle (hematoxylin–eosin stain, ×100).
In 2017, Morais et al.8 reported a case series of “LPP with pustules” revealing an atypical LPP presentation with crusts, follicular tufts and pustules. Later, the existence of FD-LPP phenotypic spectrum has been proposed.2,3 This disease can appear as a biphasic alopecia with FD preceding LPP or as the concomitant presence of both,3,4 as we described. The pathogenesis is still unclear, but Yip et al.5 proposed that a microbiome dysbiosis may stimulate an abnormal cell recruitment and collapse hair follicle immune privilege, exposing follicular neoantigens and promoting an exacerbated inflammatory response.
The phenotypic spectrum usually affects the vertex through hairless patches and can be asymptomatic or exhibit pruritus, burning and pain.8 Trichoscopic findings include hair tufts (2–5 hairs), loss of follicular openings, milky red areas, perifollicular and interfollicular scale, erythema, yellow/hemorrhagic crusts, and pustules.2–4 The childhood-onset of FDLPPPS reported herein is rare, and we were able to find only three cases in the literature.2,4
Histopathological analysis reveals loss of sebaceous glands, multicompound follicular structures, perifollicular fibrosis, atrophy of the follicular epithelium, lymphohistiocytic infiltrate with granulomas, prominent plasma cells, and scarce or absent neutrophils.2–4 Differential diagnosis includes tinea capitis, psoriasis and central centrifugal cicatricial alopecia.4,8 PA is commonly associated with psoriasis and seborrheic dermatitis, but can also appear on primary cicatricial alopecias.10 The onset of PA secondary to FDLPPPS had not been described yet, but it can occur due to the severe inflammatory condition and long duration until diagnosis. There is no standard treatment, but some cases have improved with the combination of antibacterial and oral, intralesional or topical corticosteroids.2,4,9
In conclusion, scarring alopecias are responsible for a strongly negative impact on patients’ quality of life, considering the physical and psychological implications associated with the condition. Further studies are needed to elucidate the pathogenesis of this distinctive alopecia and allow the establishment of treatment guidelines.
Conflict of interestsThe authors declare that they have no conflict of interest.